MRV Brain : Protocol and Planning
Introduction
MRV stands for magnetic resonance venography. MRV is used to assess abnormalities in venous drainage of the brain. Two-dimensional (2D) time-of-flight (TOF) MR venography (MRV) and three-dimensional (3D) phase-contrast (PC) are the techniques commonly used to assess the cerebral venous sinuses because they are easy to perform and do not require contrast administration.
Time-of-flight (TOF)
TOF (Time-of-Flight) sequence is a magnetic resonance imaging (MRI) technique that utilizes the movement of blood to generate contrast in the images. By taking advantage of the differences in magnetization between flowing blood and stationary tissues, TOF sequence produces images that highlight blood vessels and their flow dynamics. This method uses the longitudinal magnetization vector to capture the signal from the flowing blood, resulting in clear visualization of vascular structures and improved diagnosis of vascular conditions.
Phase contrast (PC)
The MRI Phase Contrast (PC) sequence is a specialized imaging technique that enables the measurement and visualization of blood flow within the body. It achieves contrast between stationary tissues and flowing blood by manipulating the phase of magnetization. In this technique, the phase of magnetization from stationary spins is zero, while the phase from moving spins is non-zero. The phase reflects the extent of the magnetization process from the time it is oriented in the transverse plane until it is detected. To minimize the signal from stationary tissue, a bipolar gradient pulse with equal magnitude but opposite direction is employed.
Phase contrast angiography (PCA) utilizes the transverse magnetization vector. In phase difference images, the signal intensity is directly proportional to the velocity of the spins. Fast-moving spins exhibit a stronger signal, appearing bright (white) in the scan when moving in one direction, while spins moving in the opposite direction appear dark (black). Phase contrast methods are sensitive to a range of velocities, requiring careful user selection. Different velocity encoding values can be applied in different scans to highlight specific vessels.
High velocity encoding, typically in the range of 40-70 cm/sec, is used for arteries due to their fast arterial flow. In contrast, low velocity encoding, usually around 10-20 cm/sec, is utilized for veins as their venous flow is slower.
Phase contrast scans can be employed for both 2D and 3D imaging, providing valuable insights into blood flow dynamics in various anatomical structures.
Indications for magnetic resonance venography (MRV) brain
- Evaluation of thrombosis
- Tumour of the cerebral venous sinus
- Drowsiness and confusion accompanying a headache
Contraindications magnetic resonance venography (MRV) brain
- Any electrically, magnetically or mechanically activated implant (e.g. cardiac pacemaker, insulin pump biostimulator, neurostimulator, cochlear implant, and hearing aids)
- Intracranial aneurysm clips (unless made of titanium)
- Pregnancy (risk vs benefit ratio to be assessed)
- Ferromagnetic surgical clips or staples
- Metallic foreign body in the eye
- Metal shrapnel or bullet
Patient preparation magnetic resonance venography (MRV) brain
- A satisfactory written consent form must be taken from the patient before entering the scanner room
- Ask the patient to remove all metal objects including keys, coins, wallet, cards with magnetic strips, jewellery, hearing aid and hairpins
- If possible provide a chaperone for claustrophobic patients (e.g. relative or staff )
- Offer earplugs or headphones, possibly with music for extra comfort
- Explain the procedure to the patient
- Instruct the patient to keep still
- Note the hight and weight of the patient
Positioning magnetic resonance venography (MRV) brain
- Head first supine
- Position the head in the head coil and immobilise with cushions
- Give cushions under the legs for extra comfort
- Centre the laser beam localiser over the glabella

Recommended MRV Brain Protocols, Parameters, and Planning
localiser
A three-plane localizer must be taken at the beginning to localize and plan the sequences. Localizers are usually less than 25 seconds and are T1-weighted low-resolution scans.

T2 tse axial
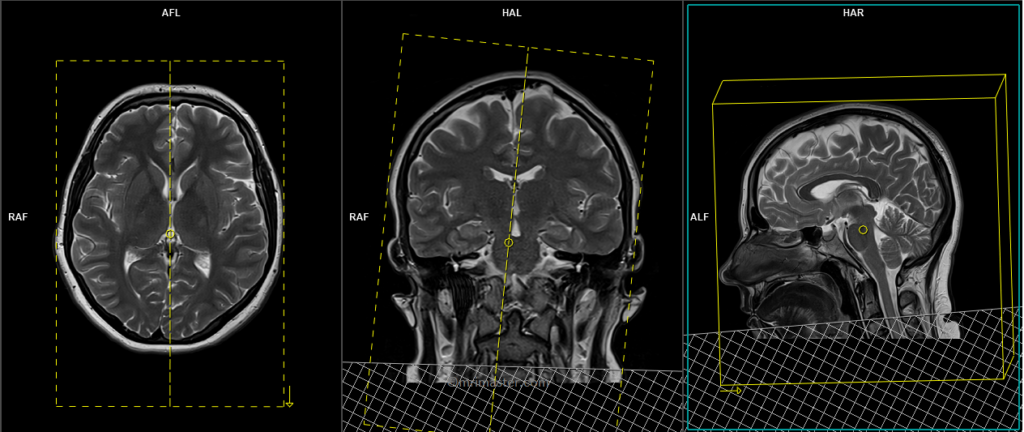
Plan the axial slices on the sagittal plane and position the block parallel to the genu and splenium of the corpus callosum. Verify the planning block in the other two planes and ensure that an appropriate angle is maintained in the coronal plane, making it perpendicular to the line of the midline of the brain and the 4th ventricle. Ensure that the number of slices is sufficient to cover the entire brain from the vertex to the line of the foramen magnum.

Parameters
TR 3000-4000 | TE 100-120 | SLICE 5MM | FLIP 130-150 | PHASE R>L | MATRIX 320X320 | FOV 210-230 | GAP 10% | NEX(AVRAGE) 2 |
3D phase-contrast (PC) sagittal
Plan the sagittal 3D block on the axial plane and position the block parallel to the midline of the brain. Verify the planningg block in the coronal plane, ensuring it is parallel to the line along the midline and 3rd ventricle. Place the saturation band at the bottom of the block in the sagittal planes to avoid capturing arterial signals. Ensure that the number of slices is sufficient to cover the entire brain from one temporal lobe to the other.

Parameters
3D phase-contrast (PC)
TR 68-75 | TE 8-9 | FLIP 15 | NEX 2 | SLICE 1MM | MATRIX 256×256 | FOV 280 | PHASE A>P | GAP 20% | Velocity 10 |
Optional 2D TOF planning for the old generation scanners
2D time-of-flight (TOF) sagittal
Plan the sagittal 3D or 2D block on the axial plane and angle the positioning block by 10° towards the midline of the brain. Verify the planning block in the coronal plane and angle it by 10° towards the midline of the brain. This angulation is intended to minimize in-plane saturation effects. Place the saturation band at the bottom of the block in the sagittal and coronal planes to avoid arterial signals. Ensure that the number of slices is sufficient to cover the entire brain from the temporal lobe to the temporal lobe.
Parameters
2D time-of-flight (TOF)
TR 28-35 | TE 5-8 | FLIP 60 | NEX 1 | SLICE 2MM | MATRIX 256×256 | FOV 250 | PHASE A>P | GAP -50% | MTC ON |
Maximum intensity projection (MIP)
MIP (Maximum Intensity Projection) is a widely used post-processing technique in MRI vascular studies. It involves the reconstruction of a 2D projection image from 3D volumetric data using a ray-tracing algorithm. This algorithm selects the highest intensity signal within the examined volume at each location and assigns it to a white pixel in the resulting image. By utilizing the maximum intensity values, MIP provides a visual representation that emphasizes the blood vessels’ highest signal intensity, enhancing their visibility and aiding in the evaluation of vascular structures. MIP images are particularly valuable in identifying vascular abnormalities, such as stenoses, aneurysms, and vascular malformations, as they highlight the regions with the strongest contrast enhancement.

