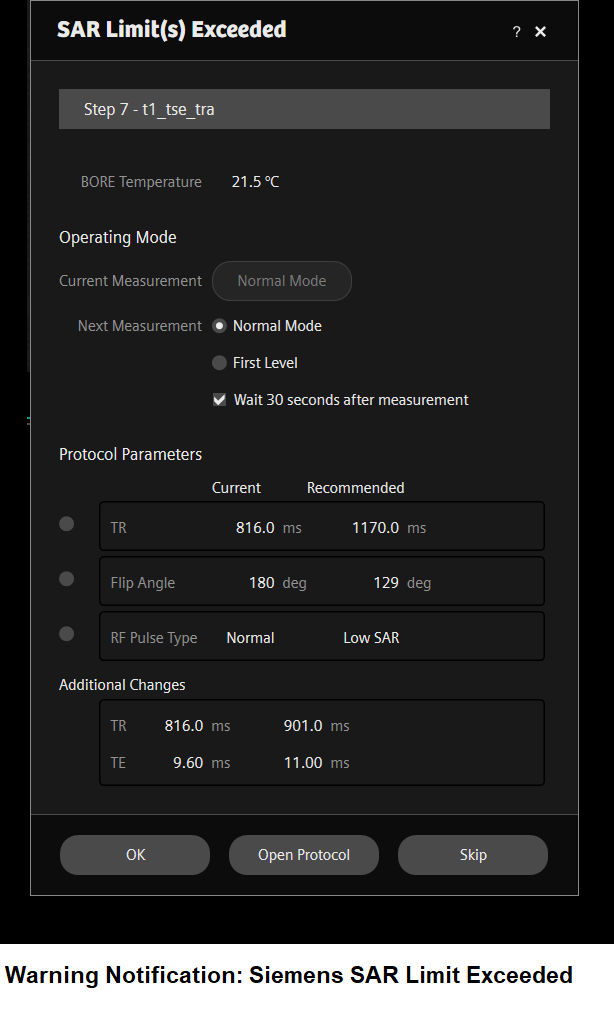
MRI Specific Absorption Rate(SAR)
Specific Absorption Rate
SAR stands for Specific Absorption Rate and is a measure of the rate at which energy is absorbed by the body when exposed to radiofrequency (RF) electromagnetic fields during an MRI scan. SAR is typically expressed in units of watts per kilogram (W/kg).
During an MRI scan, the RF pulses used to excite the protons in the body can cause heating of the tissues. SAR quantifies the amount of energy absorbed by the body per unit mass over time. It is an important safety consideration in MRI to ensure that the amount of energy absorbed does not exceed safe limits to prevent tissue heating and potential adverse effects. While MRI is generally considered a safe imaging modality, excessive tissue heating can cause burns, nerve stimulation, and other adverse effects
Generally, higher magnetic field strengths, such as those used in 3 Tesla MRI, may result in higher SAR values due to increased RF power deposition.
In the United States, the FDA has established SAR limits for MRI scanning, which vary depending on the magnetic field strength of the scanner and the duration of the scan. For example, for a 15-minute scan on a 1.5 Tesla scanner, the maximum whole-body average SAR is 4 watts per kilogram (W/kg), while for a 3 Tesla scanner, the maximum whole-body average SAR is 3.2 W/kg.
In Europe, the IEC has established similar SAR limits for MRI, which are typically lower than those used in the United States. For example, the IEC allows a maximum whole-body average SAR of 2 W/kg for a 15-minute scan on a 1.5 Tesla scanner.
Factors Affecting Specific Absorption Rate (SAR)
Magnetic field strength: SAR is directly proportional to the square of the magnetic field strength (B0). Therefore, higher magnetic field strengths, such as 3T and 7T, can result in higher SAR compared to 1.5T.
Pulse sequence parameters: The choice of pulse sequence, as well as its specific parameters, can significantly affect SAR. For example, sequences with high flip angles, short repetition times (TR), and short echo times (TE) tend to have higher SAR.
Patient size and position: SAR can vary depending on the size and position of the patient in the scanner. Larger patients may absorb more RF energy, resulting in higher SAR. Additionally, patients who are positioned closer to the RF coil may experience higher SAR.
Tissue properties: Tissue properties, such as conductivity and permittivity, can affect the amount of RF energy absorbed by the tissue, which can influence SAR. Tissues with higher conductivity, such as muscle, tend to absorb more RF energy than tissues with lower conductivity, such as bone.
Coil design and placement: The design and placement of the RF coil can affect SAR. Dedicated coils designed for specific body parts can result in higher SAR because they concentrate the RF energy in a smaller area.
Scanner hardware and software: The specific hardware and software of the MRI scanner can also affect SAR. Newer scanners with advanced technology, such as parallel imaging and RF shimming, may have lower SAR compared to older scanners.
How to reduce Specific Absorption Rate (SAR) in MRI:
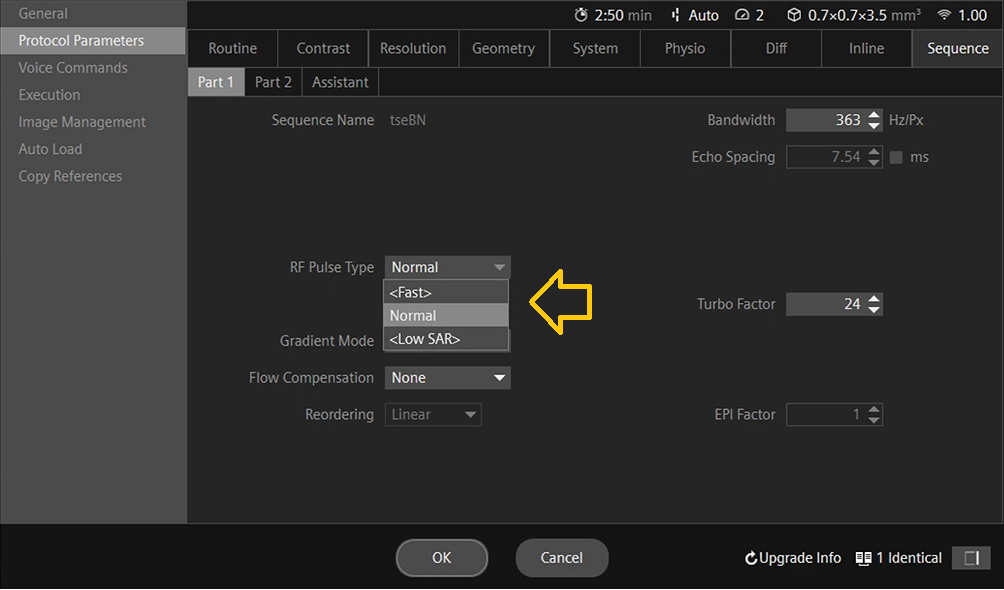
Change RF pulse type: Certain manufacturers offer users a choice of three pulse types: fast, normal, and low SAR pulse. Opting for the low SAR mode in terms of RF pulse type leads to a shift to a low bandwidth pulse characterized by reduced SAR levels.
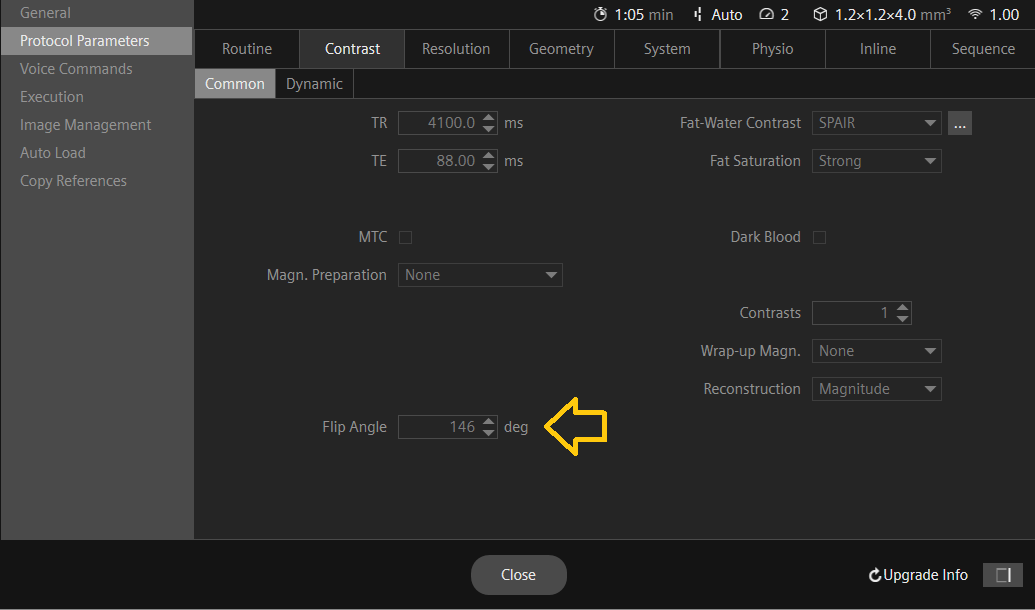
Reduce the flip angle: The flip angle is the angle at which the RF pulse is applied to the tissue. By reducing the flip angle, the amount of RF energy absorbed by the tissue can be reduced, which can in turn reduce SAR. However, reducing the flip angle may also reduce the signal-to-noise ratio (SNR) and image quality, so it should be done with caution.
Increase the TR: The repetition time (TR) is the time between successive RF pulses. By increasing the TR, the amount of time between RF pulses can be increased, which can reduce the amount of RF energy absorbed by the tissue and lower SAR.

Use a lower field strength: The SAR is directly proportional to the magnetic field strength. Therefore, using a lower field strength, such as 1.5T instead of 3T, can significantly reduce SAR. However, this may also affect the image quality, and may not be feasible for certain clinical applications.
Use a different coil: The type of coil used can also affect SAR. A smaller coil can reduce SAR because it concentrates the RF energy in a smaller area. Additionally, multi-channel coils can reduce SAR by using multiple smaller coils instead of a single larger coil.
Limit the scan time: Reducing the scan time can also reduce SAR. However, this may not always be feasible for certain clinical applications.
Use shorter pulse durations: Shorter pulse durations can reduce SAR by reducing the duration of the RF pulse and the amount of RF energy absorbed by the tissue.
Use time-interleaved acquisition: Time-interleaved acquisition is a technique that can reduce SAR by interleaving multiple acquisitions with different RF pulse timings. This technique can reduce the amount of RF energy absorbed by the tissue.
Specific Absorption Rate (SAR) Calculations
Specific Absorption Rate (SAR) calculations in different MRI scanners can vary depending on several factors, including the specific scanner model, imaging parameters, and software used.
Here’s an example of the formula for calculating the specific absorption rate (SAR) for an MRI sequence using imaging parameters:
Let’s assume we have an MRI sequence with the following imaging parameters:
Repetition time (TR): 2000 ms
Echo time (TE): 25 ms
Flip angle: 70 degrees
Slice thickness: 5 mm
Field of view (FOV): 240 mm
Matrix size: 256 x 256
Number of slices: 20
Specific absorption rate per unit B1 field (SAR/B1): 0.1 W/kg
B1 amplitude: 1 microTesla
Patient weight: 70 kg
Using the following formula:
SAR = [(0.5 x γ x B1rms x √(TR x TE) x SAR/B1) / (π x FOV x slice thickness)] x number of slices x patient weight
Where:
γ: gyromagnetic ratio = 42.58 MHz/T
B1rms: root-mean-square (RMS) of the B1 field
SAR/B1: specific absorption rate per unit B1 field
TR: repetition time
TE: echo time
FOV: field of view
Substituting the values, we get:
B1rms = (0.5 x 1 x 10^-6) / √2 = 0.0003536
SAR = [(0.5 x 42.58 x 0.0003536 x √(2000 x 25) x 0.1) / (π x 240 x 5)] x 20 x 70
SAR = 0.015 W/kg
In this example, the SAR for the given MRI sequence is 0.015 W/kg. It’s important to note that the SAR calculation can vary based on several factors, including the specific MRI sequence parameters, the patient’s size and position, and the scanner hardware. The above formula provides a general approach for calculating SAR and should only be used as an example. MRI manufacturers provide SAR information for their scanners and sequences, and it is important to monitor and control SAR levels during MRI scans to ensure patient safety.
References
- Hayes, C. E., & Edelstein, W. A. (1987). Schenck JF, Mueller OM, Eash M. An efficient, highly homogeneous radiofrequency coil for whole-body NMR imaging at 1.5 T. Journal of Magnetic Resonance (1969), 73(1), 144-149.
- Collins, C. M., & Smith, M. B. (2001). Signal-to-noise ratio and absorbed power as functions of main magnetic field strength, and definition of “90 degrees” RF pulse for the head in the birdcage coil. Magnetic Resonance in Medicine, 45(4), 684-691.
- Kainz, W., Chen, J., Oberacker, E., & Kellom, T. (2009). Specific Absorption Rate (SAR) as an MRI safety parameter: applications, challenges and future directions. Magnetic Resonance Imaging, 27(3), 423-436.
- Lu, M., Börnert, P., Eggers, H., & Rasche, V. (2004). Noninvasive temperature mapping with MRI using a proton resonance frequency technique: feasibility study in pigs. Magnetic Resonance in Medicine, 51(5), 1060-1065.
- Collins, C. M., & Liu, W. (2018). The effects of RF coil excitation on MRI: A review of the basic physics and considerations for human brain imaging. eMagRes, 7(2), 43-61.
- Atalar, E., & Hardy, C. J. (1991). Accuracy of the temperature measurement using the proton resonance frequency shift technique. Journal of Magnetic Resonance Imaging, 1(4), 446-454.
- Zollner, F. G., & Gleich, B. (2008). SAR and power implications of parallel transmission. NMR in Biomedicine, 21(9), 904-918.
- Collins, C. M., & Smith, M. B. (2001). SAR and B1 field distributions in a heterogeneous human head model within a birdcage coil. Magnetic Resonance in Medicine, 45(3), 434-438.
Note ****
The SAR calculations provided above are for illustrative purposes only and should not be used for calculating the SAR during scanning. These values can vary depending on the scanner and software used. For accurate values, please refer to the manufacturer’s guide and consult with an MRI physicist.


