MRI Parallel Imaging Artifacts
Parallel imaging artifact is a type of artifact that can occur in magnetic resonance imaging (MRI) when using parallel imaging techniques. Parallel imaging is a method used to accelerate MRI scans by simultaneously acquiring data from multiple receiver coils. However, it can introduce artifacts such as the following:
Noise amplification artifact: Due to the reconstruction of high-frequency information from the aliased signal, the noise is amplified.
Geometric distortion artifact: Due to the sensitivity of the coil array and image reconstruction methods, there can be errors in the image geometry.
Ghosting artifact: Due to incomplete phase correction, there can be residual ghosts in the image.
Signal loss artifact: Due to variations in coil sensitivity, the signal can be lost in certain regions of the image.

Here are some strategies to minimize or avoid Parallel Imaging Artifacts
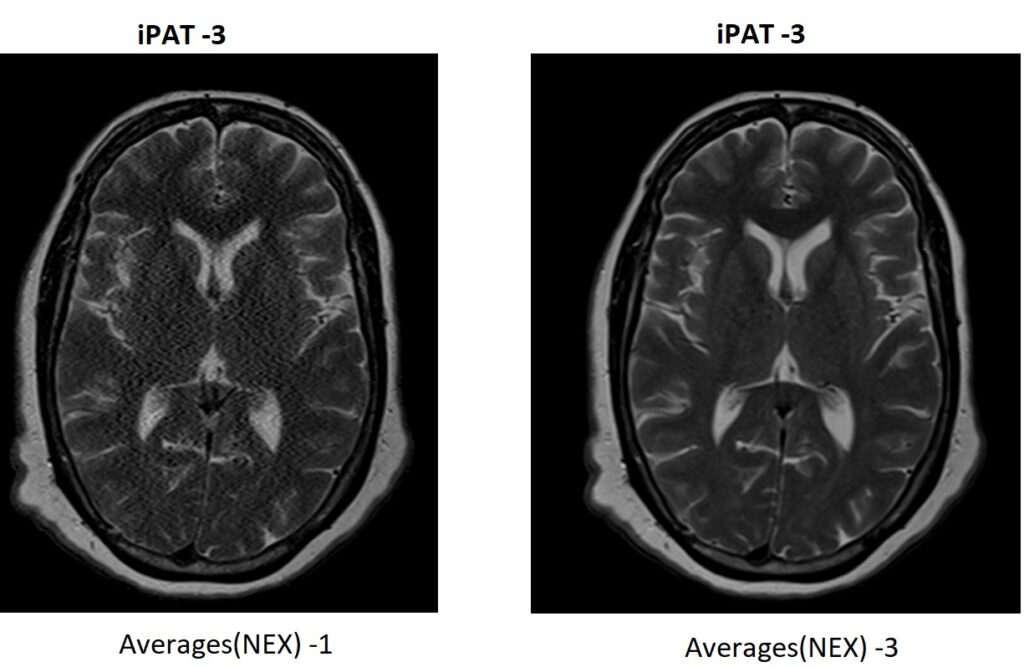
Increase signal-to-noise ratio (SNR): Higher SNR can help mitigate artifacts. Techniques such as using larger field-of-view (FOV), increasing the number of signal averages, or utilizing higher magnetic field strengths can enhance SNR and reduce artifacts.
Number of receiver coils : Increasing the number of receiver coils to improve the signal-to-noise ratio and reduce the amount of aliasing

Reconstruction algorithms: Appropriate reconstruction algorithms designed for parallel imaging, such as sensitivity encoding (SENSE) or generalized autocalibrating partially parallel acquisitions (GRAPPA), can help reduce artifacts. These algorithms exploit the
References:
- Barmet, C., et al. (2008). “Parallel imaging in MRI.” NMR in Biomedicine 21(3): 24-35.
- Griswold, M. A., et al. (2002). “Generalized autocalibrating partially parallel acquisitions (GRAPPA).” Magnetic Resonance in Medicine 47(6): 1202-1210.
- Pruessmann, K. P., et al. (1999). “SENSE: sensitivity encoding for fast MRI.” Magnetic Resonance in Medicine 42(5): 952-962.
