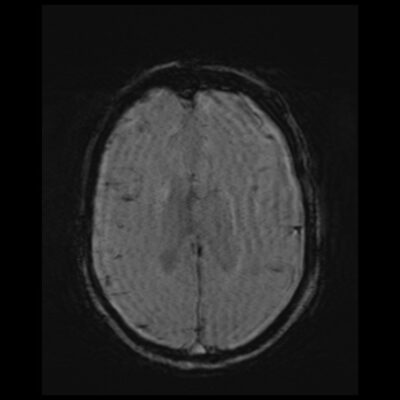
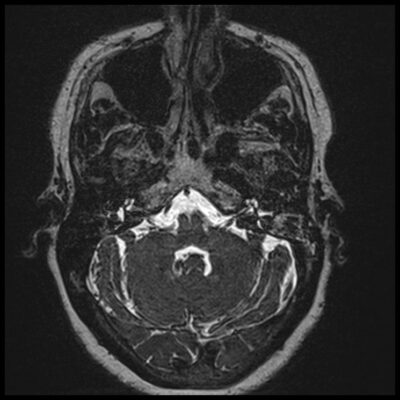
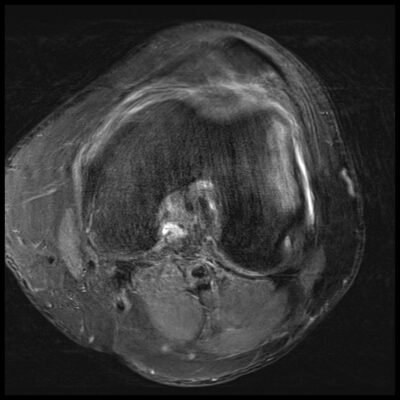
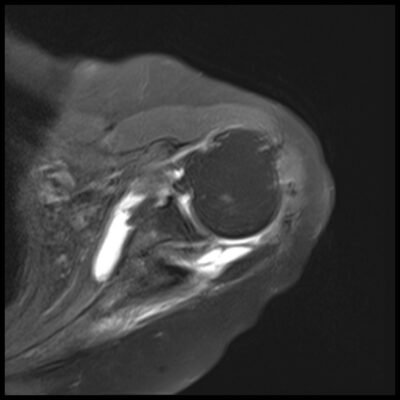
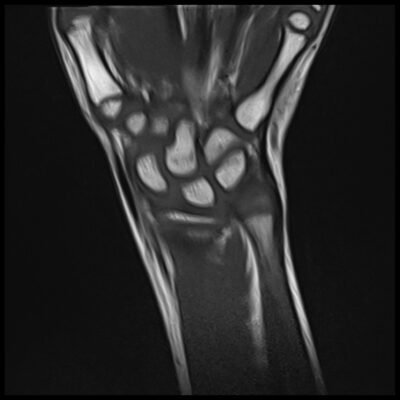
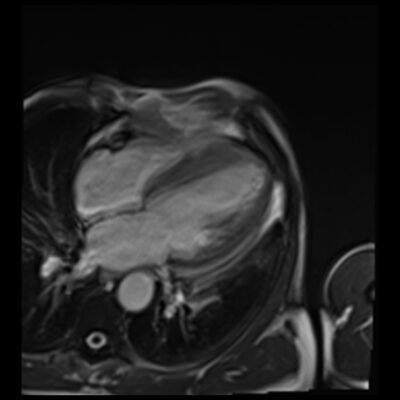
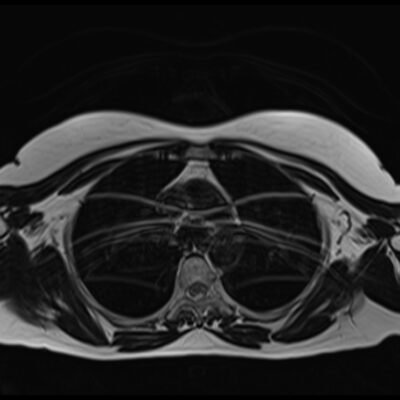
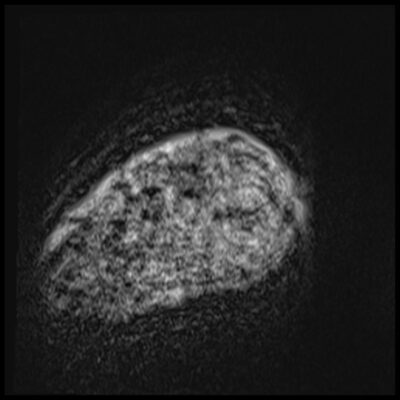
MRI Motion Artifacts (Ghosting Artifact)
Artifacts are features that appear on a reconstructed image but are not part of the original anatomy. They may make the image unclear and harder to interpret, or they can mimic the appearance of pathology. The radiographer’s aim is to minimise artifacts. However, some artifacts have clinical/diagnostic uses.
Common artifacts include:
Movement/Physiological Artifacts
Motion artifact due to physical movements
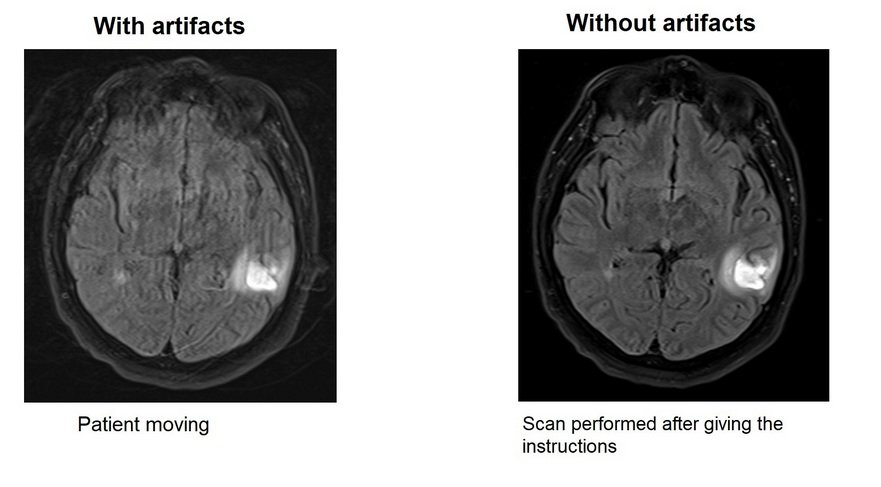
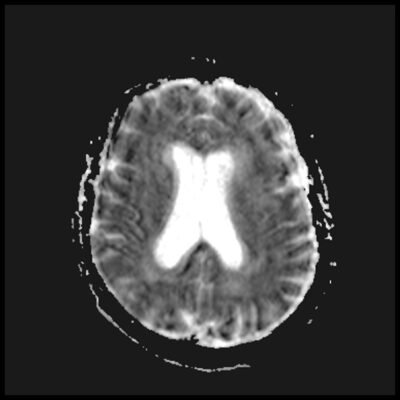
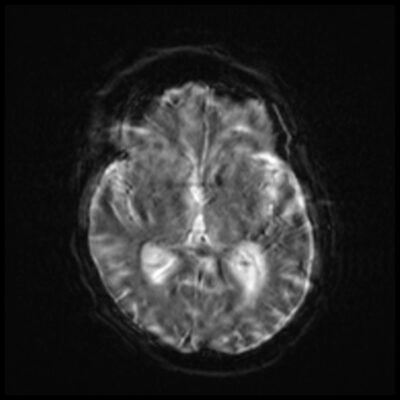
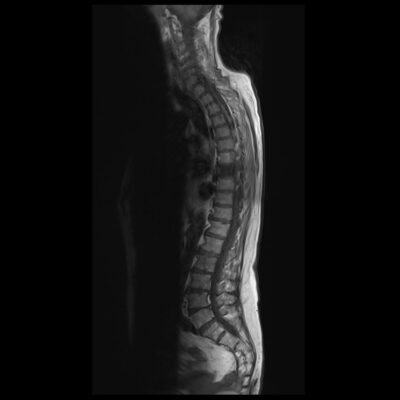
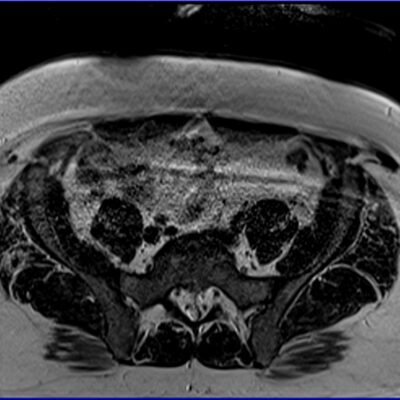
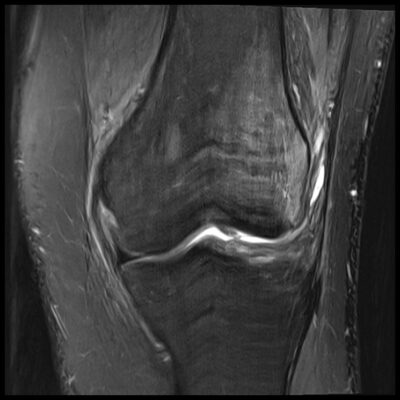
Motion artifact in MRI refers to the image degradation caused by patient or object motion during image acquisition. It can result in blurred, distorted, or ghosted images, and can significantly affect image quality and diagnostic accuracy.
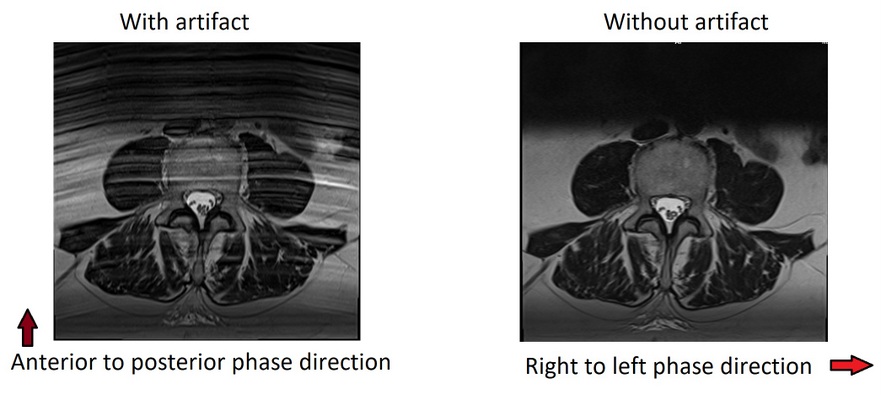
Effect on image: Artifacts usually appear as generalised blurring, ghosting, signal loss or undesired signals in the field of view especially in phase encoding direction. Artifacts mostly appear in the phase encoding direction. This is due to the phase encoding sampling time being slower than the frequency encoding. Movement of anatomy while K space is encoded in that direction means multiple images of anatomy are acquired at different times. This leads to the production of generalised blurring or ghosting on the image.
How to reduce or minimise the motion or Ghosting artifacts
- Give clear instructions to patient before the scan
- Constantly communicate to claustrophobic patients
- Make the patient comfortable
- Use immobilization equipment or paddings
- Feed and wrap the infants
- Use oral or IV sedation
- Perform the scans under GA
- reduce scan time using fast scan techniques
- use radial k-space sampling techniques
- Adjust phase and frequency encoding directions to project artifact away from anatomy
- Use compressed sensing techniques
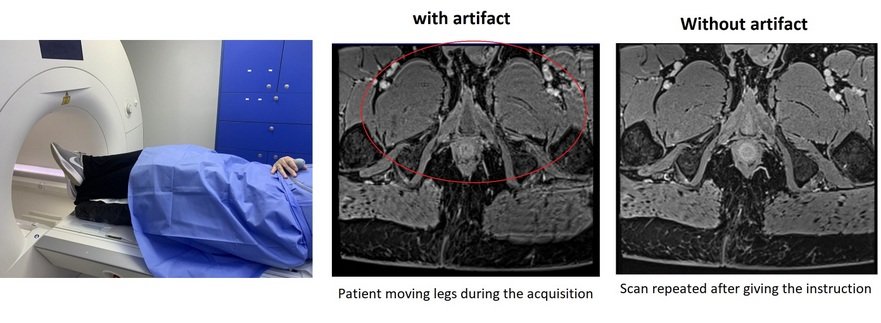
Instructing patients: Properly instructing patients is crucial to minimize motion artifacts in MRI. Patients may involuntarily move due to unexpected loud noises or vibrations from the scanner table. Radiographers should educate patients on the importance of staying still during the procedure to ensure the quality of the MRI images. Clear and concise communication with patients can help minimize motion artifacts and optimize the diagnostic accuracy of the MRI.
Patients may mistakenly believe that moving body parts away from the area being scanned, such as crossing or uncrossing their legs during a pelvic or lumbar spine scan, is permissible. However, such movements can cause localized blurring of the image, which can be difficult to detect.
Claustrophobic patients: MRI claustrophobia is a severe anxiety disorder triggered by the confined space inside the MRI tunnel, which may cause patients to move or shift their position during the scan. To alleviate this, patients with claustrophobia should be positioned with their feet first whenever possible. It is crucial to maintain constant communication and reassurance with claustrophobic patients. Skilled MRI radiographers should regularly inform the patients about the scan and sequence timing. Fast imaging techniques may also enhance the patient’s overall experience.

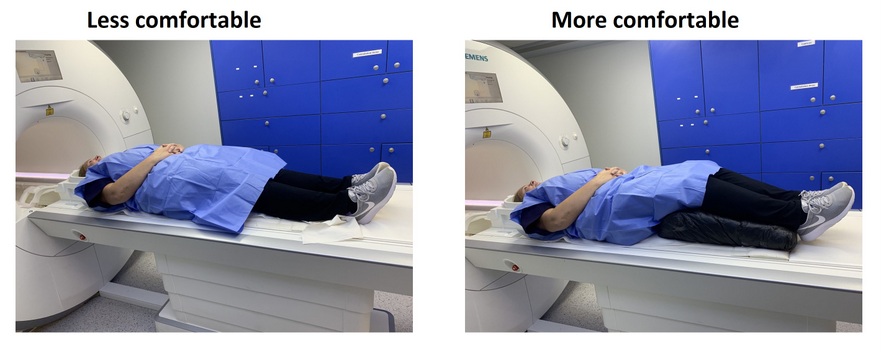
Patient comfort: The risk of motion artifacts increases significantly if the patient is uncomfortable during the MRI scan. Discomfort can be caused by incorrect positioning on the MRI table, such as in the case of a patient with backache who may benefit from a cushion under their legs. To help improve patient comfort, scanner manufacturers often provide a variety of positioning wedges for different types of examinations. Radiographers should have a good understanding of when and where to use these wedges to optimize patient comfort and reduce the likelihood of motion-related artifacts.
Immobilization equipments: Immobilization support in MRI scanners includes various tools such as wedges, cushions, straps, and sandbags. These tools are used to restrict patient movement during the scan and reduce motion-related artifacts. Manufacturers of MRI scanners typically provide immobilization kits consisting of wedges, sandbags, and straps. To ensure proper use of these materials, refer to the accompanying photographs that demonstrate their application.

Feed and wrap technique: The feed and wrap technique involves the feeding and swaddling of infants to facilitate natural sleep, and it serves as an alternative to sedation or anesthesia during MRI procedures. Radiographers and MRI administrators should provide parents with instructions for preparation, which includes keeping the infant awake for several hours before the appointment to aid in sleep during the scan, ensuring that the infant is hungry and due for a feed before the appointment to promote uninterrupted sleep during the scan, and dressing the infant in clothing without zips or metal poppers.
Sedation or general anaesthesia: To ensure minimal motion during an MRI scan, sedation or anesthesia is often administered to patients who are unable to remain still for various reasons, including confusion, autism, or pediatric patients. The image quality obtained under sedation or anesthesia is superior to that obtained using fast gradient echo sequences or motion correction techniques.
Fast sequences:
Performing an MRI scan on moving patient is extremely difficult. When scanning a moving object, the radiographers’ aim should be to achieve a diagnostic quality scan in a shortest possible time period. There are number of ways to perform fast scans.
Gradient echo sequence: Gradient echo sequences are a type of MRI pulse sequence that utilize changes in the magnetic field gradient to produce image contrast. Gradient echo sequences are generally faster than spin echo sequences, making them useful for imaging moving structures and for reducing scan time. There are several types of gradient echo (GRE) sequences, including:
Spoiled gradient echo sequence (SPGR): This is a fast and commonly used GRE sequence that is ideal for imaging tissues with high T1 relaxation times, such as brain white matter and fat.
Balanced steady-state free precession (bSSFP) sequence (TrueFISP): This GRE sequence is used for cardiac and musculoskeletal imaging due to its high signal-to-noise ratio (SNR) and excellent contrast between tissues.
Gradient recalled echo (GRE) sequence: This is a classic GRE sequence that can be used for various applications, including functional MRI (fMRI) and dynamic contrast-enhanced MRI (DCE-MRI).
Echo-planar imaging (EPI) sequence: This GRE sequence is used for fast imaging, including functional MRI and diffusion-weighted imaging (DWI).
Fast low angle shot (FLASH) sequence: This GRE sequence is used for high-resolution imaging of the brain and is particularly useful for imaging cortical layers and small structures.

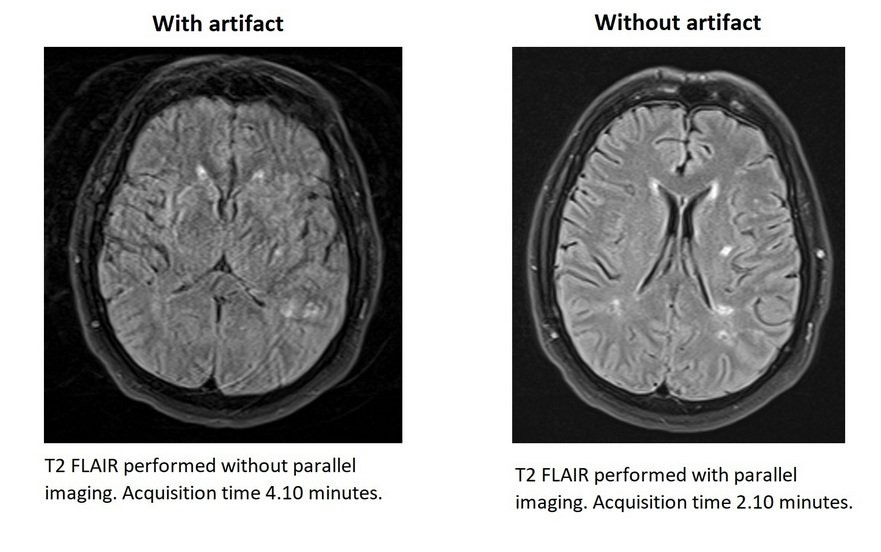
Parallel imaging: To minimize motion artifacts caused by occasional patient movement, parallel imaging techniques can be employed to reduce scan time. Using multiple receiver coils, parallel imaging can decrease the amount of data required, leading to faster scanning times. Advanced MRI scanners using parallel imaging can achieve higher acceleration factors, allowing for diagnostic-quality scans in less than a minute.
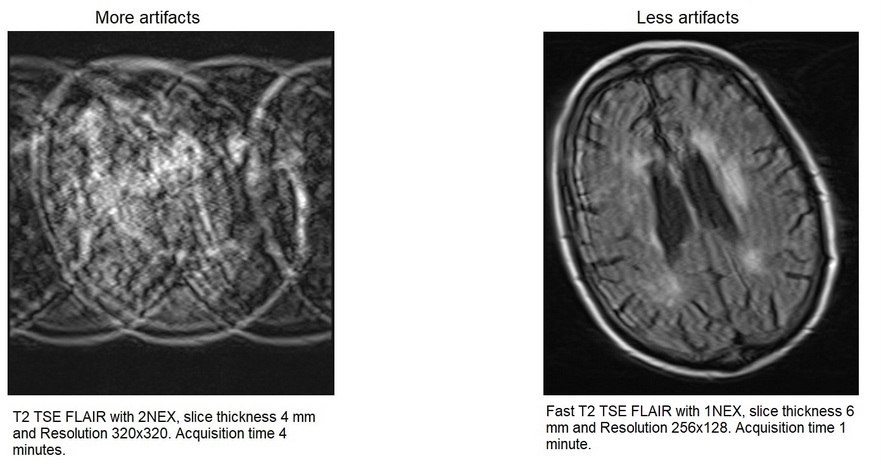
Other techniques: A skilled radiographer has the ability to reduce the scanning time by adjusting various parameters such as slice thickness, field of view (FOV), resolution, bandwidth, and number of signal averages (NSA).
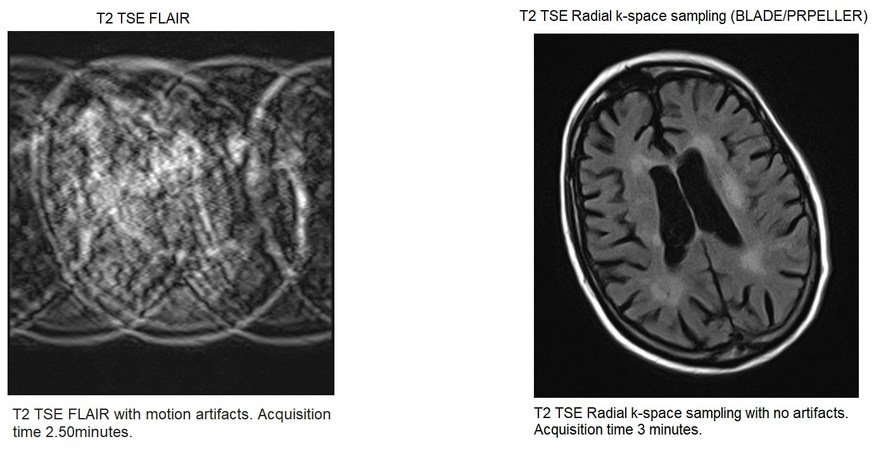
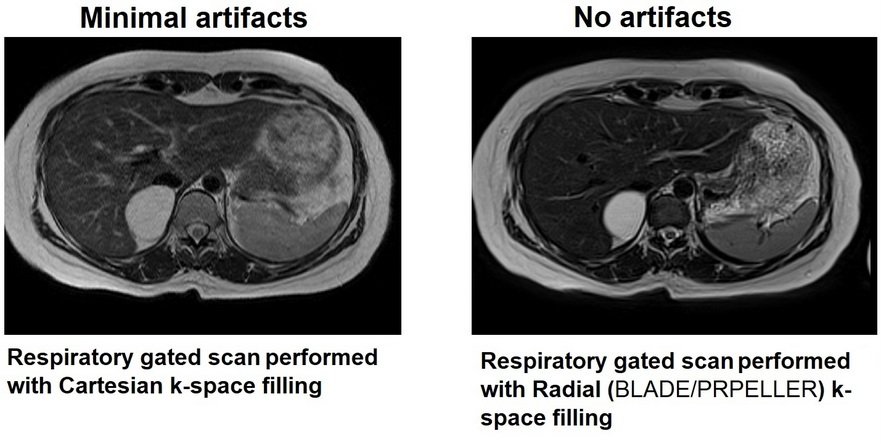
Radial k-space sampling (BLADE/PRPELLER): Radial k-space sampling is a technique used in advanced MRI to reduce the effect of motion artifacts on image quality. The method involves acquiring k-space data in concentric rectangular strips that rotate around the k-space origin. The central part of k-space, which contains essential information, is sampled more frequently during each strip acquisition. To minimize phase, translation, and rotation artifacts, an average strip is used. However, this technique may introduce its own artifacts, such as curved “ghosts” or fine “halo” effects of bands/streaks in head imaging.
Compressed sensing
Compressed sensing MRI is a relatively new imaging technique that allows for the acquisition of high-quality images with reduced scan time and data acquisition. The technique uses a sophisticated signal processing technique that allows for the acquisition of high-quality MRI images from a reduced number of measurements. CS employs a random under-sampling method that reduces the number of k-space samples during data acquisition, resulting in a reduced scan time. By combining compressed sensing with parallel imaging, the acquisition time can be further shortened, providing a higher acceleration factor. By using CS techniques, an isotropic 3D MRI scan can be acquired in under 3 minutes, which is a significant improvement over traditional MRI scans.

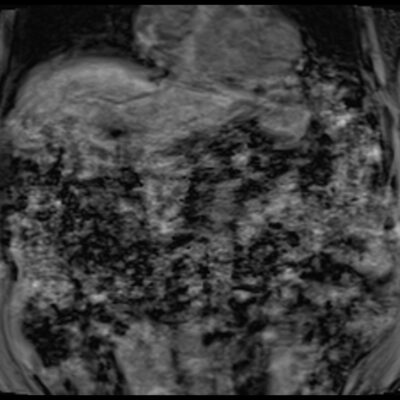
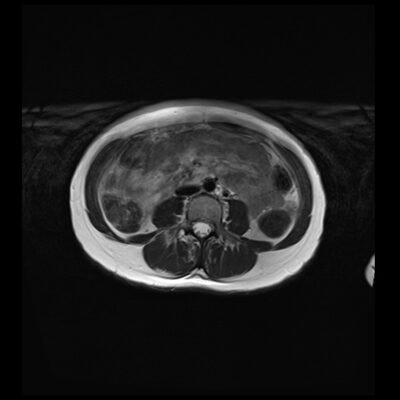
Respiratory Motion Artifacts
Breathing is one of the main sources of motion artifacts in MRI. Continues breathing during the image acquisition can cause ghosting, blurring, misregistration, or signal loss in the reconstructed images.
How to reduce or minimise the artifacts
- perform the scans under breath hold
- use respiratory gated sequences
- use radial k-space sampling techniques
- adjust phase and frequency encoding directions to project artifact away from anatomy
- use compressed sensing techniques
- increase the number of signal averaging
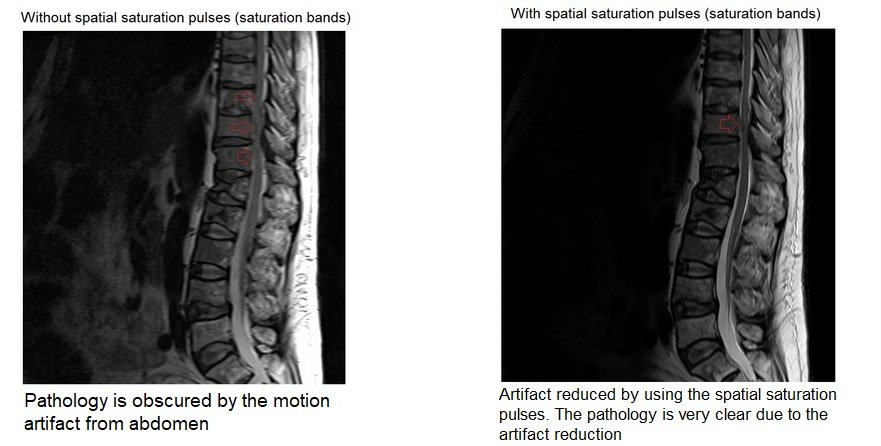
- Spatial saturation pulses (saturation bands) over the moving anatomy
- use fat suppression sequences
Breath hold Imaging techniques
To mitigate respiratory artifacts during MRI acquisition, breath hold imaging techniques are commonly employed. However, some patients may not be able to hold their breath for an extended period, leading to difficulties in image acquisition. In such cases, reducing the acquisition time or utilizing multiple breath holds can be useful. Various techniques such as parallel imaging, compressed sensing, and adjusting the resolution and phase FOV can also be employed to overcome this issue.

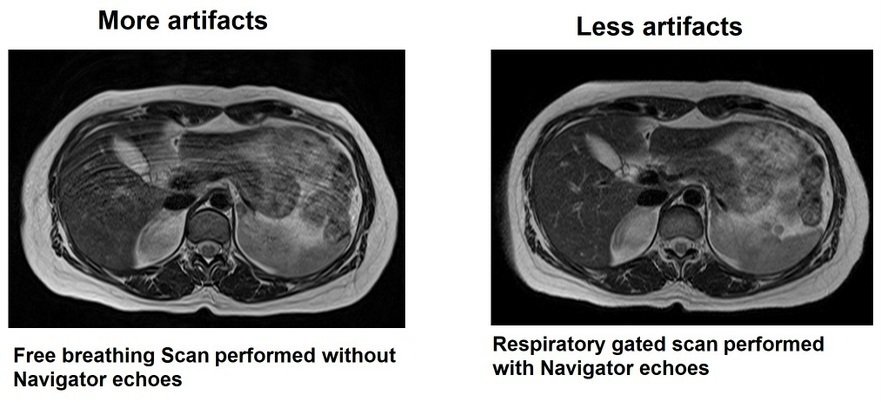
Respiratory gated scans
When patients are unable to hold their breath for prolonged periods, respiratory gated sequences can be used as an alternative. In this technique, the data acquisition is triggered during expiration, and several respiratory gating methods are available on most MRI scanners. These methods include respiratory gating equipment or the use of navigator echoes during scanning.
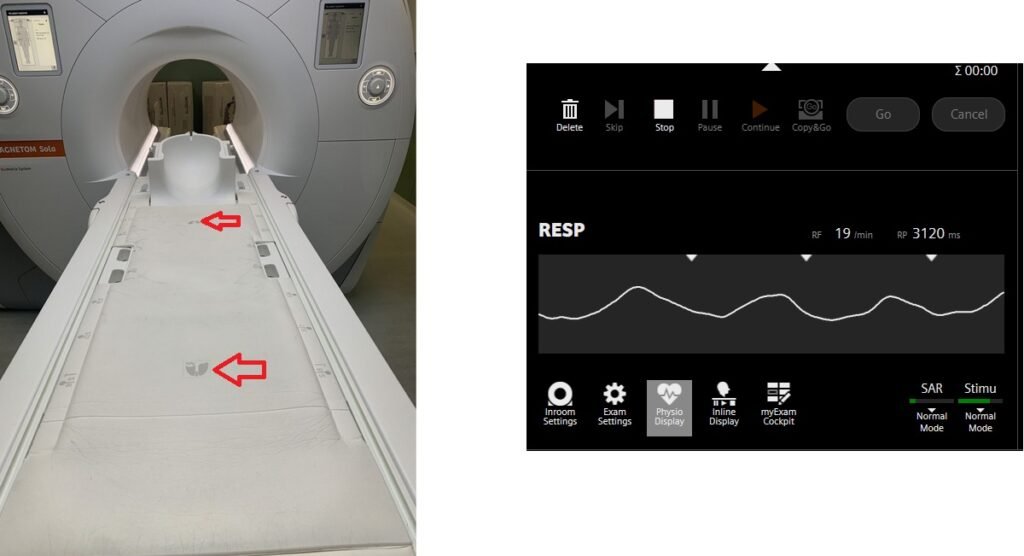
Respiratory gating equipment (respiratory bellows, respiratory table sensers or respiratory belts)
The respiratory gating equipment comprises a sensor, belt, and tubing. When positioning the patient, the respiratory sensor should be placed on the lower chest or mid abdomen and secured with the respiratory belt. The belt should be tightened sufficiently to allow the sensor to detect the patient’s breathing. Next, connect the tubing from the sensor to the MRI system. Radiographers can verify the sensor’s placement accuracy by monitoring the respiratory waveform on the scanning monitor’s gating window.
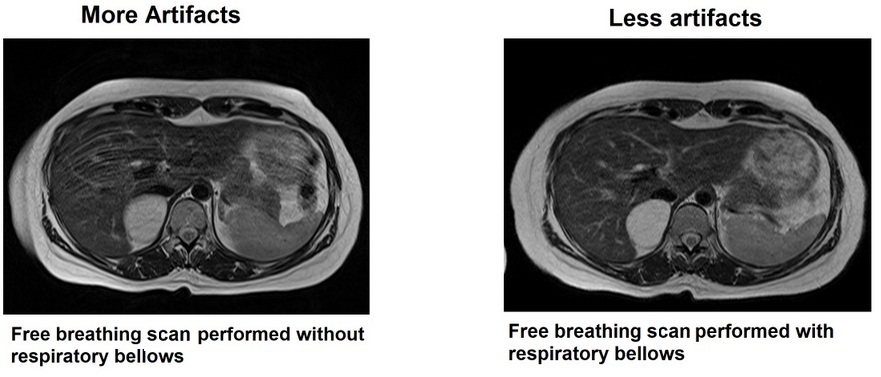
Advanced MRI scanners are equipped with built-in table sensors that detect the respiratory waveform and trigger data acquisition during the expiration phase of the respiratory cycle. Proper patient positioning over the sensor is critical for accurate respiratory gating. This method eliminates the need for external respiratory gating equipment, such as sensors and belts.
Navigator echoes
The respiratory navigator technique is a novel approach that enables motion artifact-free imaging of the chest and abdomen without requiring breath-holding. The technique employs navigator echoes, which consist of a two-dimensional pulse that excites a cylinder of spins, followed by a readout gradient in the direction of the long axis of the cylinder to acquire a 1-dimensional profile of the area of interest. The navigator pulse has a low flip angle (10) to reduce saturation, and the sharp signal intensity change of the lungs and liver along the axis of the box is used to determine the diaphragm position. The navigator pulse is executed intermittently every 200 milliseconds, and a scan acceptance window is determined from the preliminary pre-scan data, after which the actual scan acquisition begins.
In the case of abdomen and chest imaging, the navigator box is placed over the diaphragm. During each slice acquisition, the navigation box detects the position of the diaphragm, and imaging only takes place when the diaphragm falls within the expiration acceptance window.
Phase and frequency encoding directions
The majority of respiratory motion artifacts typically manifest in the phase encoding direction. To address this, changing the phase and frequency encoding directions can project the motion artifacts away from the region of interest. This technique is commonly utilized in spinal and pelvic imaging to eliminate artifacts caused by motion in the abdomen and chest.
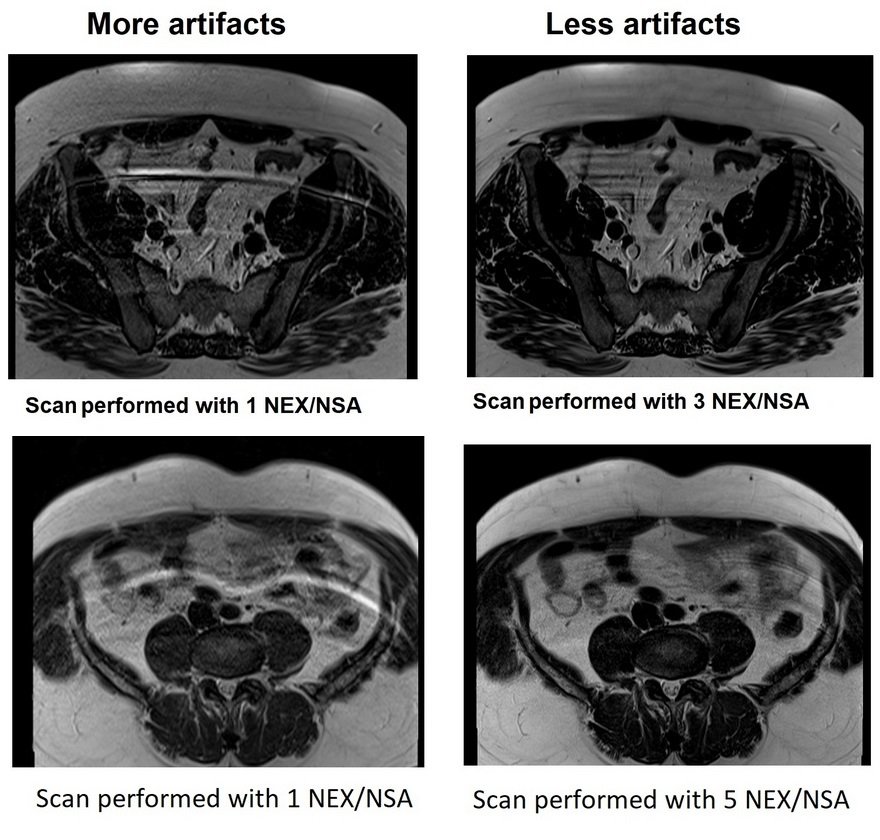
Number of signal averaging (NSA/averages)
Number of excitations (NEX) or number of signal averages/acquisitions (NSA) is a measurement parameter. It is used to represent the number of times each line of k-space data is acquired. Increasing the number of signal averaging increases the SNR and reduces artifacts.
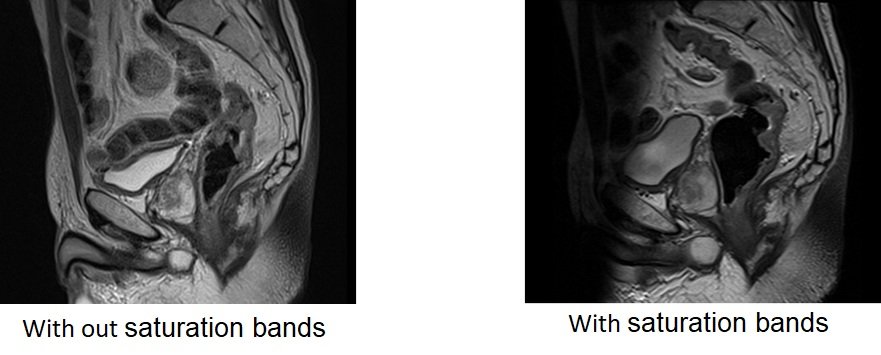
Spatial saturation pulses
MRI uses spatial saturation pulses (also known as saturation bands) to reduce motion artifacts caused by moving tissues outside the area of interest. This technique involves applying an additional radiofrequency (RF) pulse before the imaging sequence to eliminate the signal from unwanted tissue. Spatial saturation pulses are particularly useful in spine and pelvic imaging to minimize motion artifacts from breathing, peristalsis, pulsation, and swallowing.
Radial k-space sampling
To eliminate motion artifacts in abdominal and chest imaging, advanced scanners use a combination of radial k-space sampling and breath hold techniques. Radial k-space sampling is a method of data acquisition in which the centre of k-space is acquired more frequently than the outer parts. This technique is combined with breath hold TSE scans to produce high-quality images. Compared to traditional TSE breath hold sequences, breath hold TSE scans with radial k-space sampling are slightly superior. In pelvic imaging, TSE-based radial k-space sampling sequences without breath hold are used to minimize artifacts from breathing, peristalsis, and flow.
Compressed sensing GRASP VIBE
Compressed sensing GRASP VIBE is a specific MRI acquisition technique that combines compressed sensing (CS) and golden-angle radial sparse parallel (GRASP) imaging with volumetric interpolated breath-hold examination (VIBE) sequence. This technique allows for high spatiotemporal resolution dynamic imaging of the liver and other organs, while reducing acquisition time and motion artifacts. The GRASP sampling strategy and the CS reconstruction method provide the ability to recover images with high temporal fidelity from undersampled k-space data.. By using compressed sensing, dynamic contrast-enhanced abdominal imaging can be performed under free-breathing.

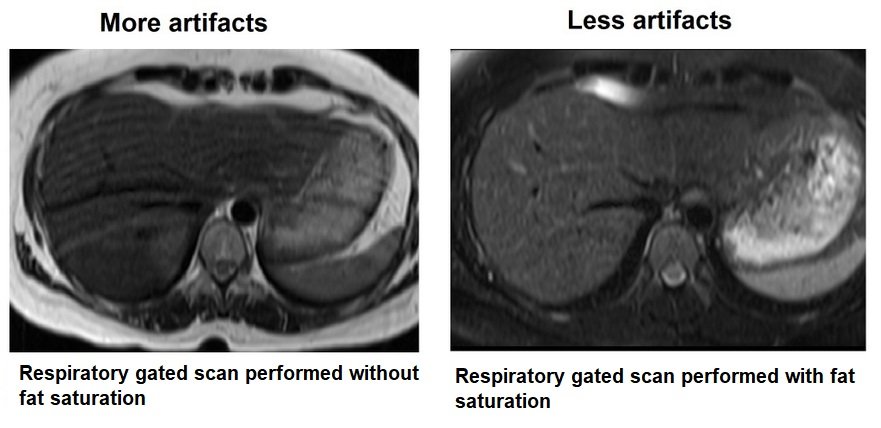
Fat suppression sequences
Many fat suppression techniques are used in MRI to supress the signals from adipose tissues. The most commonly used fat suppression methods are STIR, Hybrid spectral and inversion recovery, DIXON, CHESS, chemical fat saturation and water excitation. Suppressing the fat signal reduces the high signal from subcutaneous fat which contributes towards the motion artifacts.
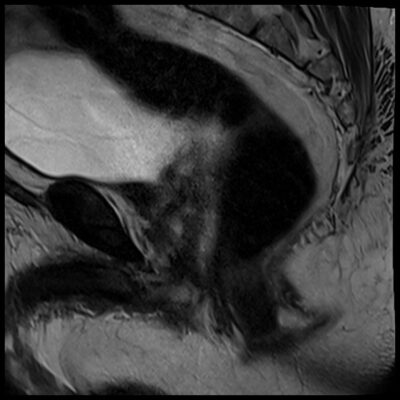
Motion artifact due to swallowing
swallowing is one of the main sources of motion artifact in the neck, carotid artery, and oral cavity imaging. Artifacts appeared as generalised blurring, ghosting, or undesired signals in the field of view especially in phase encoding direction.
How to reduce or minimise the artifacts
- Ask the patient to stop swallowing during the acquisition

- Use radial k-space sampling techniques
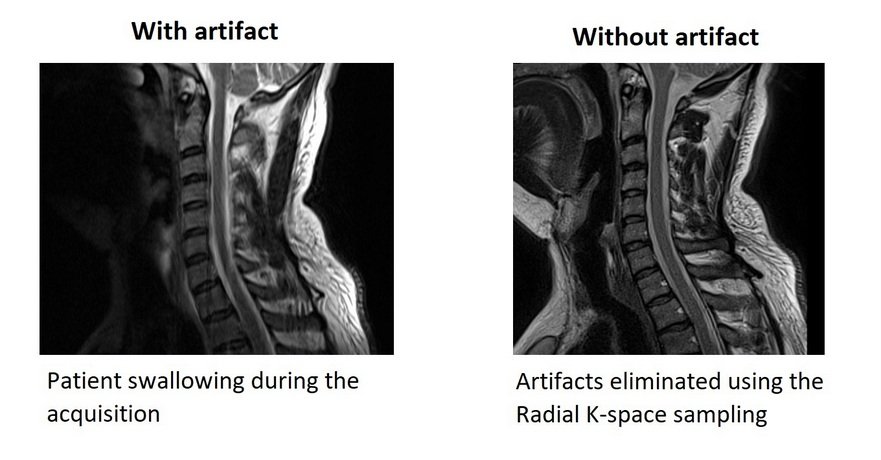
- adjust phase and frequency encoding directions to project artifact away from anatomy
- increase the number of signal averaging
- Use spatial saturation pulses over moving anatomy
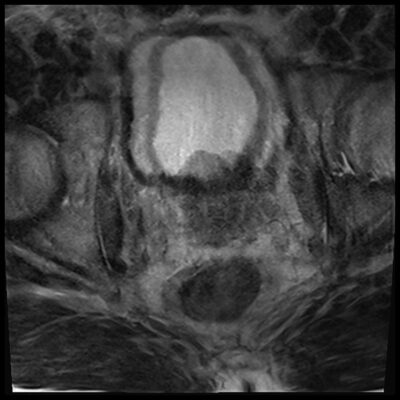
Motion Artifact due to Peristalsis
Peristaltic motion is one of the main sources of artifacts in the abdominal and pelvic magnetic resonance (MR) imaging. Peristalsis related motion artifacts appeared as generalised blurring or ghosting.
How to reduce or minimise the artifacts
- Use antispasmodic medication
- Use fast gradient echo scans
- Use Spatial saturation pulses over the moving anatomy
Antispasmodic drugs are administered in MRI to relax the smooth muscles of the gastrointestinal tract. The commonly used antispasmodics include hyoscine butylbromide (buscopan) and glucagon. Within 20 to 30 seconds of intravenous administration, antispasmodics stop peristalsis. Peristalsis usually recovers a few minutes after the administration of antispasmodics. To take advantage of the period of reduced motion, it is advisable to use fast breath-hold sequences immediately after the administration of IV antispasmodics.

Fast gradient echo scans
Ultra-fast single-shot gradient and turbo spin echo sequences, such as TrueFISP (balanced FFE, FIESTA) and HASTE (SSFFE, SSTSE), are commonly used in MRI imaging due to their short acquisition times and reduced motion artifacts. TrueFISP is a steady-state coherent sequence that can acquire a single slice image in just a fraction of a second. Similarly, HASTE sequences are also fast and less sensitive to motion artifacts. These sequences are ideal for imaging body parts that are prone to motion, such as the chest and abdomen.
Saturation bands
Use Spatial saturation pulses (saturation bands) over the moving anatomy
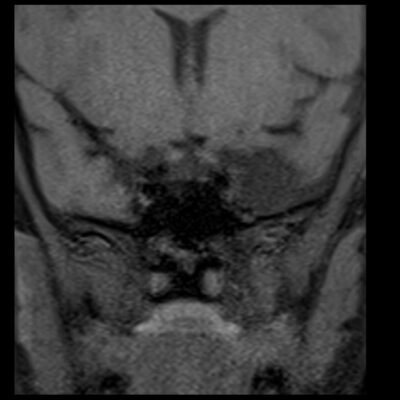
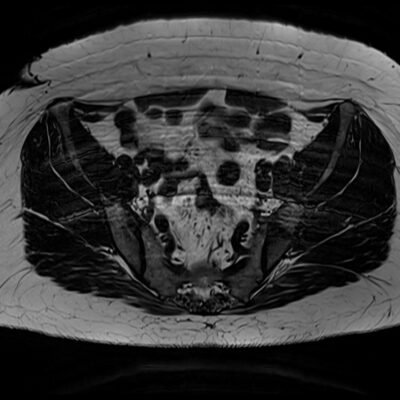
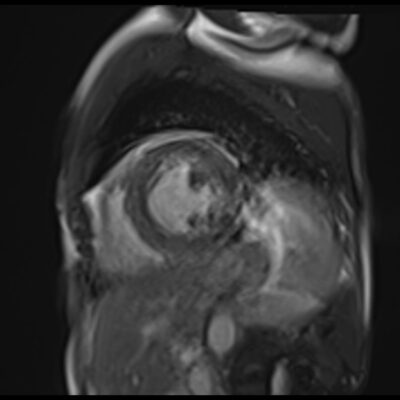
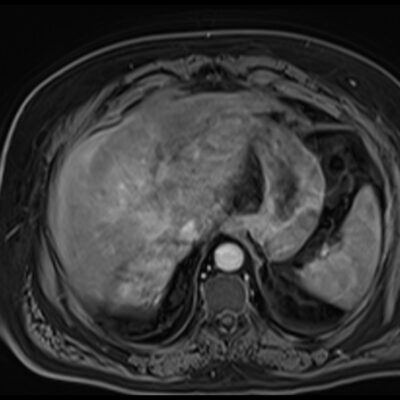
Motion artifact image gallery















References
- Krupa K, Bekiesińska-Figatowska M. Artifacts in Magnetic Resonance Imaging. Pol J Radiol. 2015;80:93-106. Published online 2015 Feb 23. doi: 10.12659/PJR.892628. PMCID: PMC4340093. PMID: 25745524.
- Noda, C., Venkatesh, B. A., Wagner, J. D., Kato, Y., Ortman, J. M., & Lima, J. A. C. (2022). Primer on Commonly Occurring MRI Artifacts and How to Overcome Them. RadioGraphics, 42(3).
- Hargreaves, B. A., Worters, P. W., Pauly, K. B., Pauly, J. M., Koch, K. M., & Gold, G. E. (September 2011). Metal-Induced Artifacts in MRI. American Journal of Roentgenology, 197(3).
- Dietrich, O., Reiser, M. F., & Schoenberg, S. O. (2008). Artifacts in 3-T MRI: Physical background and reduction strategies. European Journal of Radiology, 65(1), 29-35.
- Ferreira, P. F., Gatehouse, P. D., Mohiaddin, R. H., & Firmin, D. N. (2013). Cardiovascular magnetic resonance artefacts. Journal of Cardiovascular Magnetic Resonance, 15, 41.
- Havsteen, I., Ohlhues, A., Madsen, K. H., Nybing, J. D., Christensen, H., & Christensen, A. (2017). Are Movement Artifacts in Magnetic Resonance Imaging a Real Problem?—A Narrative Review. Frontiers in Neurology, Volume 8, Section Stroke.
- Zaitsev M, Maclaren J, Herbst M. “Motion Artefacts in MRI: a Complex Problem with Many Partial Solutions.” J Magn Reson Imaging. 2015 Oct; 42(4): 887–901. Published online 2015 Jan 28. doi: 10.1002/jmri.24850. PMID: 25630632. PMCID: PMC4517972. NIHMSID: NIHMS651865.
- Blumenthal, J. D., Zijdenbos, A., Molloy, E., & Giedd, J. N. (2002). Motion Artifact in Magnetic Resonance Imaging: Implications for Automated Analysis. NeuroImage, 16(1), 89-92.
- Gutierrez, P. A., Dulcich, G., Soubielle, A., De Felippo, A., Puech, P., & Pietrani, M. (2023). Oops I did it again! : How to identify MRI artifacts and correct them on time. Certificate of Merit. Presented at ECR 2023, Poster Number C-14718, Educational Exhibit. DOI: 10.26044/ecr2023/C-14718.
