IAM'S (Ménière’s disease protocol)
Ménière’s disease
Ménière’s disease, also known as endolymphatic hydrops, is a disorder of the inner ear that affects both hearing and balance. It is named after the French physician Prosper Ménière, who first described the condition in the 1860s.
The main symptoms of Ménière’s disease include:
Vertigo: A sensation of spinning or dizziness that can be severe and disabling.
Tinnitus: Ringing, buzzing, or other noises in the ear.
Hearing loss: Episodes of hearing loss, which may fluctuate and eventually become permanent in some cases.
A feeling of fullness or pressure in the affected ear.
The exact cause of Ménière’s disease is not fully understood, but it is believed to be related to a build-up of fluid in the inner ear, known as endolymphatic hydrops. This fluid imbalance disrupts the normal functioning of the inner ear structures responsible for hearing and balance.
Ménière’s disease can occur at any age, but it is most common in individuals between the ages of 40 and 60. The condition can be unpredictable, with sudden attacks of vertigo and other symptoms that may last for hours to days. Over time, it can lead to permanent hearing loss and ongoing balance issues.
Treatment for Ménière’s disease aims to manage symptoms and includes dietary changes, medication to control vertigo and nausea, and sometimes surgical interventions in severe cases.
The latest advancements in MRI have enabled radiologists to identify cochlear or vestibular EH by utilizing post-contrast FLAIR 3D imaging. This particular imaging is conducted after the administration of IV gadolinium, approximately 4 hours later. For optimal results, it is recommended to conduct these scans using a 3T scanner.
Indications for the scan
- Ménière’s disease
Contraindications of MRI scan
- Any electrically, magnetically or mechanically activated implant (e.g. cardiac pacemaker, insulin pump biostimulator, neurostimulator, cochlear implant, and hearing aids)
- Intracranial aneurysm clips (unless made of titanium)
- Pregnancy (risk vs benefit ratio to be assessed)
- Ferromagnetic surgical clips or staples
- Metallic foreign body in the eye
- Metal shrapnel or bullet
Patient preparation internal auditory meatus(iams) MRI scan
- A satisfactory written consent form must be taken from the patient before entering the scanner room
- Ask the patient to remove all metal objects including keys, coins, wallet, cards with magnetic strips, jewellery, hearing aid and hairpins
- If possible provide a chaperone for claustrophobic patients (e.g. relative or staff )
- Contrast injection risk and benefits must be explained to the patient before the scan
- Gadolinium should only be given to the patient if GFR is > 30
- Offer earplugs or headphones, possibly with music for extra comfort
- Explain the procedure to the patient
- Instruct the patient to keep still
- Note the hight and weight of the patient
Positioning
- Head first supine
- Position the head in the head coil and immobilise with cushions
- Give cushions under the legs for extra comfort
- Centre the laser beam localiser over the glabella

MRI Ménière’s disease Protocols, Parameters, and Planning
localiser
A three-plane localizer must be taken at the beginning to localize and plan the sequences. Localizers are usually less than 25 seconds and are T1-weighted low-resolution scans.

T2 tse axial 5mm
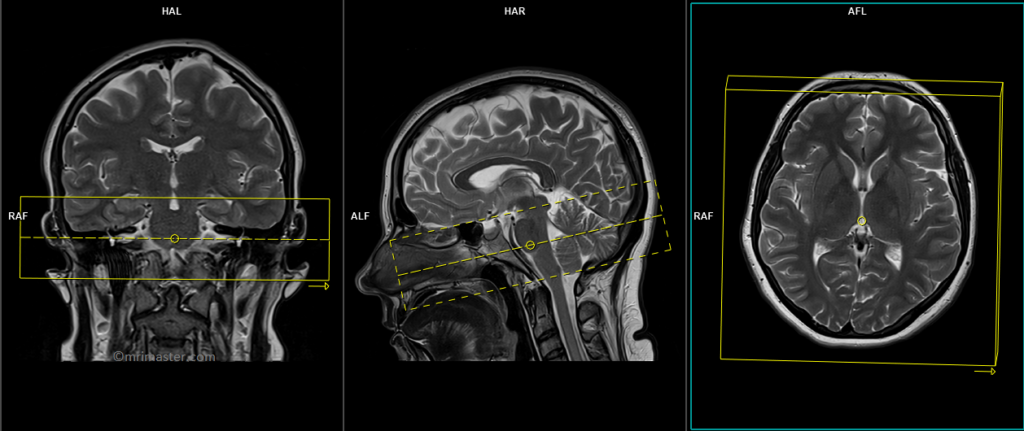
Plan the axial slices on the sagittal plane and position the block parallel to the genu and splenium of the corpus callosum. Verify the planning block in the other two planes and ensure that an appropriate angle is maintained in the coronal plane, making it perpendicular to the line of the midline of the brain and the 4th ventricle. Ensure that the number of slices is sufficient to cover the entire brain from the vertex to the line of the foramen magnum.

Parameters
TR 3000-4000 | TE 100-120 | SLICE 5MM | FLIP 130-150 | PHASE R>L | MATRIX 320X320 | FOV 210-230 | GAP 10% | NEX(AVRAGE) 2 |
T2 TSE coronal 3mm
Plan the coronal slices on the axial plane and angle the planning block parallel to the line along the right and left Internal Auditory Meatus (IAMS) (as shown in the diagram). Verify the planning block in the other two planes. Ensure an appropriate angle is maintained in the sagittal plane, parallel to the brain stem. The number of slices should be sufficient to cover the IAMS from the posterior border of the sphenoid sinus up to the line of the fourth ventricle.These coronal T2 scans are performed to aid in the planning of axial 3D scans.

Parameters
TR 3000-4000 | TE 110 | FLIP 130 | NEX 2 | SLICE 3MM | MATRIX 256X256 | FOV 150-180 | PHASE R>L | GAP 10% | SLICE 10-20% |
T2 3D SPACE (3D CISSor 3DFIESTA) axial .5mm
Plan the axial slices on the coronal plane and angle the planning block parallel to the line along the right and left internal auditory meatus (IAMS), as shown in the diagram. Verify the planning block in the other two planes. Ensure an appropriate angle is maintained in the sagittal plane, perpendicular to the brain stem. The number of slices should be sufficient to cover the IAMS from the hippocampus up to the line of the C1 vertebral body.

Parameters CISS
TR 12-15 | TE 6-7 | SLICE .8mm | FLIP 80 | PHASE R>L | MATRIX 384X320 | FOV 210-230 | GAP 10% | NEX(AVRAGE) 1 |
For contrast enhanced delayed scans
T2 SPACE FLAIR 3D axial .8mm Delayed 4 hours
Plan the axial slices on the coronal plane and angle the planning block parallel to the line along the right and left internal auditory meatus (IAMS), as shown in the diagram. Verify the planning block in the other two planes. Ensure an appropriate angle is maintained in the sagittal plane, perpendicular to the brain stem. The number of slices should be sufficient to cover the IAMS from the hippocampus up to the line of the C1 vertebral body.
T2 SPACE FLAIR 3D axial .8mm images

T2 SPACE FLAIR 3D coronal reconstructed images

Parameters
TR 6000-7000 | TE 300-400 | SLICE .7mm | TI 2050 | PHASE R>L | MATRIX 224X224 | FOV 200-230 | GAP 10% | NXA(AVRAGE) 2 |


