Magnetic Resonance Cholangiopancreatography (MRCP): Protocol and Planning
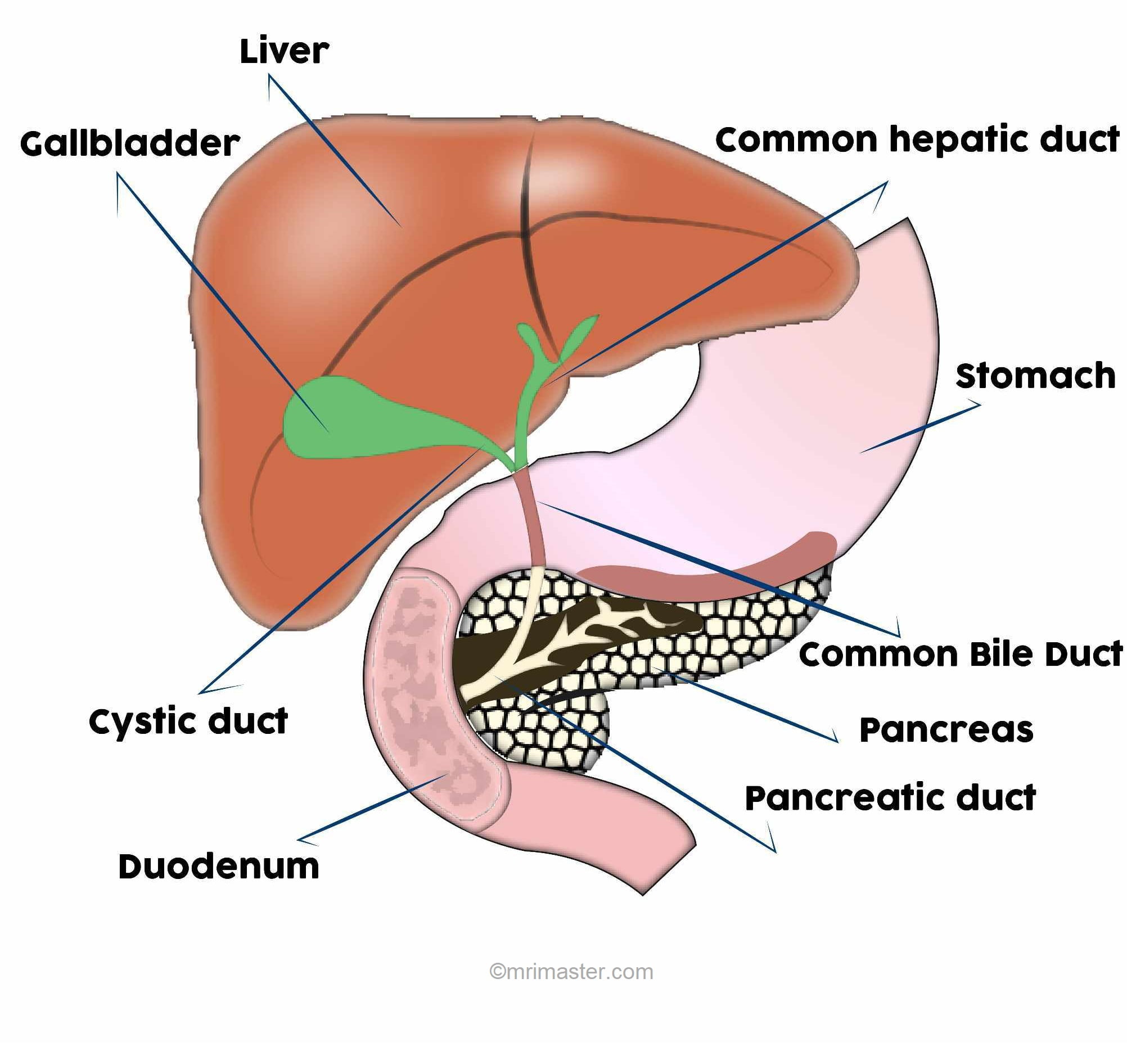
Anatomy of biliary system
The anatomy of the biliary system is of utmost importance in radiology as it plays a crucial role in the diagnosis and treatment of biliary disorders. The biliary system consists of various interconnected structures that facilitate the production, transportation, and storage of bile.
Starting with the liver, the intrahepatic bile ducts collect bile produced by hepatocytes. These ducts merge to form the right and left hepatic ducts, which exit the liver and join together to form the common hepatic duct. The common hepatic duct combines with the cystic duct from the gallbladder to form the common bile duct.
The common bile duct runs through the head of the pancreas and usually joins the main pancreatic duct, forming the hepatopancreatic ampulla (ampulla of Vater). The ampulla opens into the duodenum through the sphincter of Oddi, allowing the release of bile into the digestive system.
Please check our new video tutorial for protocols and planning
Indications for magnetic resonance cholangiopancreatography
- Biliary obstruction (choledocholithiasis, benign and malignant strictures)
- Bile ducts, surgery or postsurgical biliary tract alterations
- Biliary cystadenoma and cystadenocarcinoma
- Congenital anomalies
- Pancreatic pseudocyst
- Chronic pancreatitis
- Acute cholecystitis
- Bile ducts, calculi
- Pancreatic cancer
- Pancreas divisum
Contraindications
- Any electrically, magnetically or mechanically activated implant (e.g. cardiac pacemaker, insulin pump biostimulator, neurostimulator, cochlear implant, and hearing aids)
- Intracranial aneurysm clips (unless made of titanium)
- Pregnancy (risk vs benefit ratio to be assessed)
- Ferromagnetic surgical clips or staples
- Metallic foreign body in the eye
- Metal shrapnel or bullet
Patient preparation for MRCP
- A satisfactory written consent form must be taken from the patient before entering the scanner room
- Ask the patient to remove all metal objects including keys, coins, wallet, cards with magnetic strips, jewellery, hearing aid and hairpins
- Ask the patient to undress and change into a hospital gown
- Instruct the patient to hold their breath for the breath hold scans and breathe gently for the gated scans. It is recommended to provide coaching to the patient two to three times before initiating the scan.
- Claustrophobic patients may be accompanied into the scanner room e.g. by staff member or relative with proper safety screening
- Patients should fast for 4 -6 hours before the exam (nothing to eat or drink)
- Offer headphones for communicating with the patient and ear protection
- Explain the procedure to the patient and answer questions
- Note down the weight of the patient
Positioning for MRCP
- Position the patient in supine position with head pointing towards the magnet (head first supine)
- Position the patient over the spine coil and place the body coil over the upper abdomen (nipple down to iliac crest)
- Securely tighten the body coil using straps to prevent respiratory artefacts
- Give a pillow under the head and cushions under the legs for extra comfort
- Centre the laser beam localizer over xiphoid process of sternum

Recommended MRI MRCP Protocols, Parameters, and Planning
localiser
To localize and plan the sequences, it is essential to acquire a three-plane T2 HASTE localizer initially. These fast single-shot localizers have an acquisition time of under 25 seconds and are highly effective in accurately localizing abdominal structures.

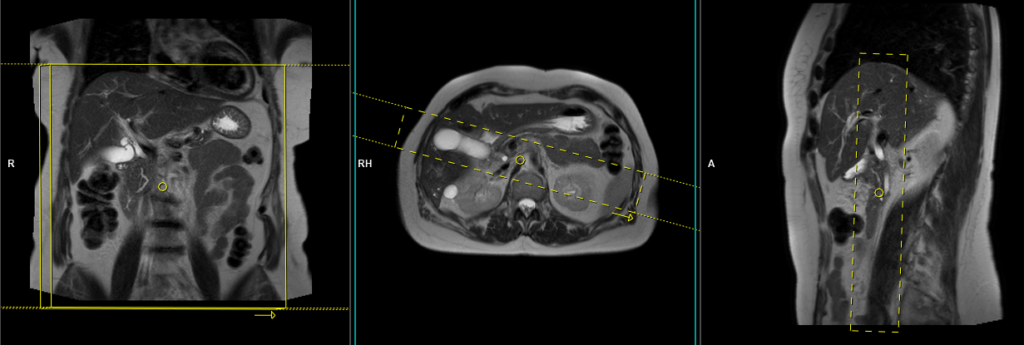
T2 HASTE 5 mm breath hold coronal
Plan the coronal slices on the axial localizer and position the block horizontally across the liver as depicted. Verify the position in the other two planes. Establish an appropriate angle in the sagittal plane, aligning it vertically across the liver. Ensure that the slices adequately cover the entire liver, extending from the anterior abdominal wall to the erector spinae muscles. The phase direction should be from right to left to minimize ghosting artifacts from the lungs and heart. Employ phase oversampling to prevent wrap-around artifacts. Instruct the patient to hold their breath during image acquisition. (In our department, we typically advise patients to breathe in and out twice before providing the instruction to “breathe in and hold”.)
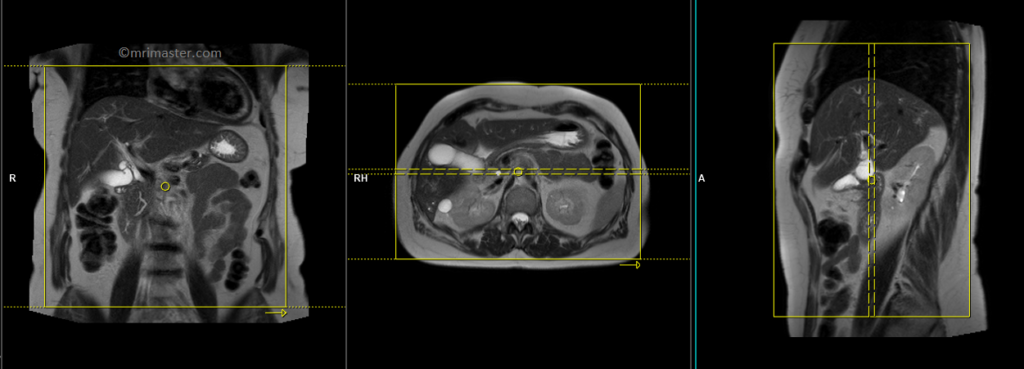
Parameters
TR 2000-2500 | TE 90-110 | FLIP 130 | NEX 1 | SLICE 5MM | MATRIX 320×256 | FOV 350 | PHASE R>L | OVERSAMPLE 50% | TRIGGER NO |
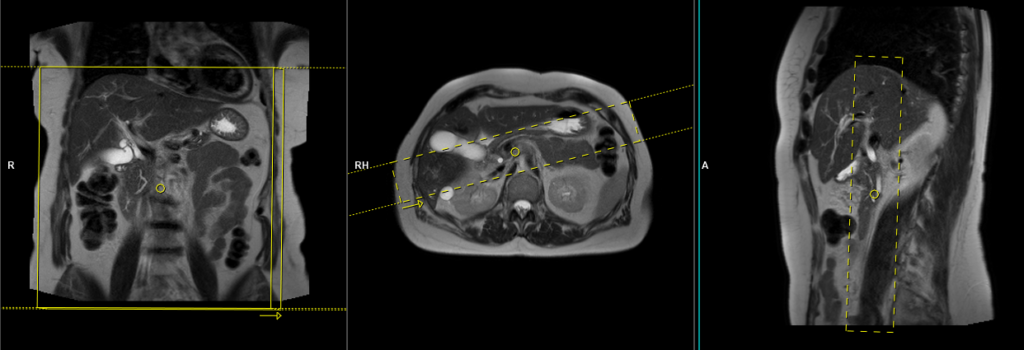
T2 HASTE 5 mm breath hold axial
Plan the axial slices on the coronal breath hold images and position the block horizontally across the liver as shown. Verify the positioning in the other two planes. Establish an appropriate angle in the sagittal plane, aligning it horizontally across the liver. The slices must be sufficient to cover the entire liver from the diaphragm down to the C loop of the duodenum. The phase direction should be from right to left to minimize ghosting artifacts from the anterior abdominal wall. Use phase oversampling to prevent wrap-around artifacts. Instruct the patient to hold their breath during image acquisition. (In our department, we typically instruct patients to take two breaths in and out before providing the “breathe in and hold” instruction.)
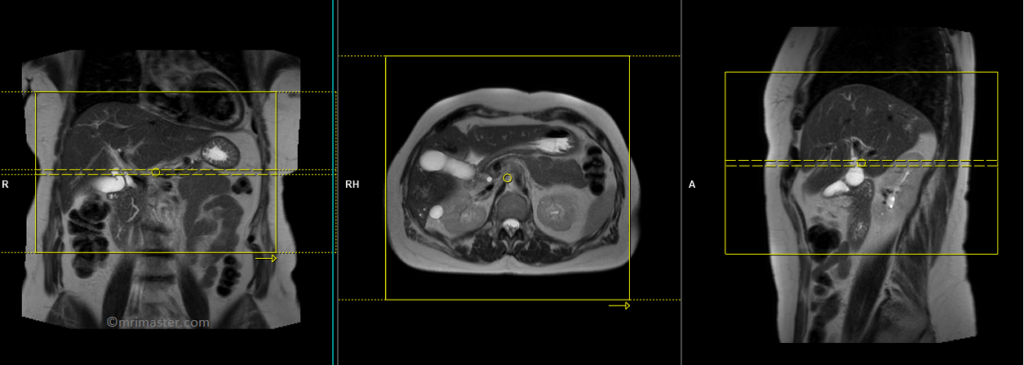

TR 2500-3000 | TE 90-110 | FLIP 130 | NEX 1 | SLICE 5MM | MATRIX 256×256 | FOV 350 | PHASE R>L | OVERSAMPLE 50% | TRIGGER NO |
T2 HASTE fat sat 5mm breath hold axial
Plan the axial slices on the coronal breath hold images and position the block horizontally across the liver as shown. Verify the positioning in the other two planes. Establish an appropriate angle in the sagittal plane, aligning it horizontally across the liver. The phase direction should be from right to left to minimize ghosting artifacts from the anterior abdominal wall. Use phase oversampling to prevent wrap-around artifacts. Instruct the patient to hold their breath during image acquisition. (In our department, we typically instruct patients to take two breaths in and out before providing the “breathe in and hold” instruction.)
Parameters
TR 3000-4000 | TE 110 | FLIP 150 | NEX 1 | SLICE 5 MM | MATRIX 320X320 | FOV 400-450 | PHASE A>P | OVERSAMPLE 50% | IPAT Off |
T2 HASTE thick 40mm breath hold coronal oblique (single slice)
Plan the coronal oblique (left anterior oblique) thick slab on the axial HASTE sequence. Position the block across the common bile duct and rotate it 20-30 degrees clockwise to include both the common bile duct and gall bladder. Verify the positioning in the other two planes. Establish an appropriate angle in the sagittal plane, aligning it horizontally across the bile duct. Ensure that the slice thickness is sufficient to cover the entire common bile duct and gall bladder. Use phase oversampling to prevent wrap-around artifacts. Instruct the patient to hold their breath during image acquisition.
Parameters
TR 4000-5000 | TE 500 | FLIP 150 | NEX 1 | SLICE 40MM | MATRIX 320X320 | FOV 350-450 | PHASE R>L | OVERSAMPLE 50% | IPAT ON |
T2 HASTE thick 40mm breath hold coronal (single slice)
Plan the coronal thick slab on the axial HASTE sequence. Position the block across both the common bile duct and pancreatic duct (without concern for excluding part of the gallbladder). Verify the positioning in the other two planes. Establish an appropriate angle in the sagittal plane, aligning it horizontally across the bile duct. Ensure that the slice thickness is sufficient to cover the entire common bile duct and pancreatic duct. Use phase oversampling to prevent wrap-around artifacts. Instruct the patient to hold their breath during image acquisition.

Parameters
TR 4000-5000 | TE 500 | FLIP 150 | NEX 1 | SLICE 40MM | MATRIX 320X320 | FOV 350-450 | PHASE R>L | OVERSAMPLE 50% | IPAT ON |
T2 HASTE thick 40mm breath hold coronal oblique(single slice)
Plan the coronal oblique (right anterior oblique) thick slab on the axial HASTE sequence. Position the block across the common bile duct and rotate it 20-30 degrees counterclockwise to include both the common bile duct and pancreatic duct (without concern for excluding part of the gallbladder). Verify the positioning in the other two planes. Establish an appropriate angle in the sagittal plane, aligning it horizontally across the bile duct. Ensure that the slice thickness is sufficient to cover the entire common bile duct and pancreatic duct. Use phase oversampling to prevent wrap-around artifacts. Instruct the patient to hold their breath during image acquisition.
Parameters
TR 4000-5000 | TE 500 | FLIP 150 | NEX 1 | SLICE 40MM | MATRIX 320X320 | FOV 350-450 | PHASE R>L | OVERSAMPLE 50% | IPAT ON |
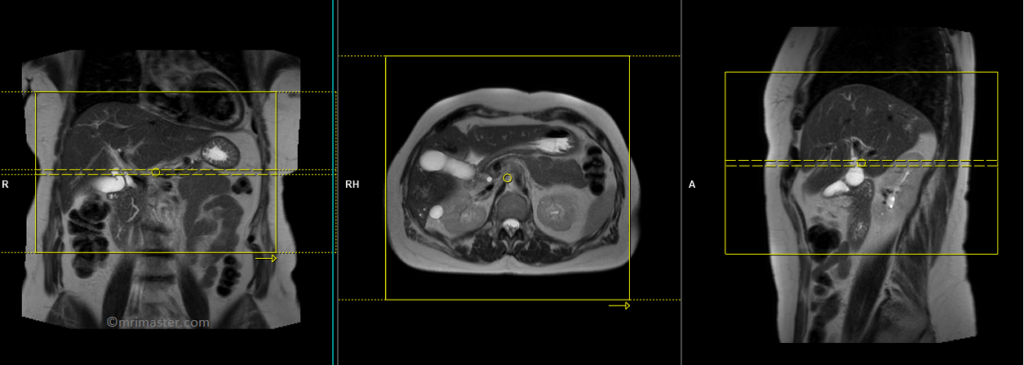
T2 SPACE 3D(or T2 TSE) coronal respiratory gated 1MM
Plan the coronal 3D sequence on the axial HASTE scan. Position the block across the common bile duct and pancreatic duct. Verify the positioning in the other two planes. Establish an appropriate angle in the sagittal plane, aligning it horizontally across the bile duct. Ensure that the slices adequately cover the entire common bile duct, pancreatic duct, and gall bladder. Use phase oversampling to prevent wrap-around artifacts.
For respiratory gated scans, it is crucial to accurately position the respiratory navigator box. Place it in the middle of the right dome of the diaphragm, with half of the box over the right lobe of the liver (segment 8) and the other half over the lungs. Planning should be performed in a non-breath hold localizer, as the diaphragm pushes down the liver during inhalation, which can lead to improper slice planning and positioning of the respiratory navigator box.
Instruct the patient to breathe gently throughout the sequence. Very shallow or erratic breathing can reduce the effectiveness of the navigator.
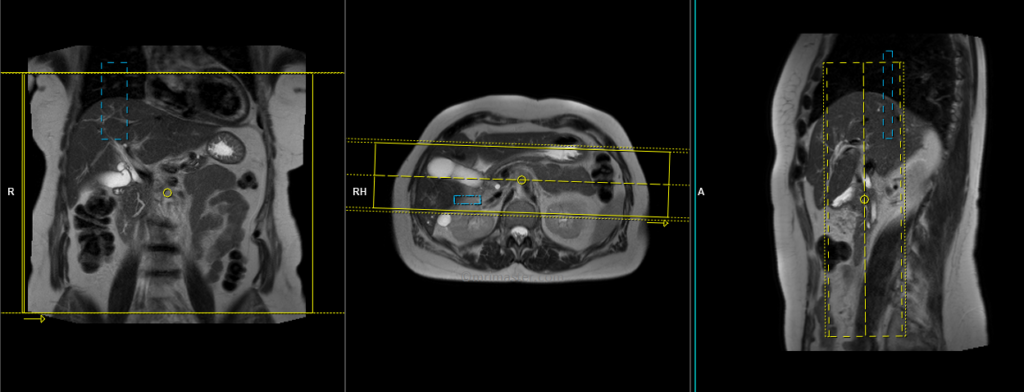
Parameters
TR 2500-3000 | TE 500-700 | FLIP 12 | NEX 1 | SLICE 1MM | MATRIX 320X320 | FOV 350 | PHASE R>L | OVERSAMPLE 50% | IPAT ON |
T2 HASTE thick 40mm breath hold coronal oblique(radial)
Plan the coronal radial thick slab slices on the axial HASTE sequence. Position the center of the block over the common bile duct . Verify the positioning in the other two planes. Establish an appropriate angle in the sagittal plane, aligning it horizontally across the bile duct. Ensure that the slices adequately cover the entire common bile duct and pancreatic duct. Use phase oversampling to prevent wrap-around artifacts. Instruct the patient to hold their breath during image acquisition.

Parameters
TR 4000-5000 | TE 500 | FLIP 150 | NEX 1 | SLICE 40MM | MATRIX 320X320 | FOV 300-400 | PHASE R>L | OVERSAMPLE 50% | IPAT ON |
