PANCREAS (respiratory gated)
Indications for pancreas mri scan
- Characterization of suspected parenchymal abnormalities found on CT or ultrasound
- Detection of small non-organ-deforming pancreatic ductal adenocarcinomas
- Evaluation of acute and chronic pancreatitis when CT is not diagnostic
- Detection of choledocholithiasis as a cause of acute pancreatitis
- Detection of intraluminal pancreatic duct calculi
- Detection and staging of pancreatic neoplasms
- Characterization of cystic pancreatic lesions
- Detection of endocrine tumours
- Pancreatic cancer
- Pancreas divisum
Contraindications
- Any electrically, magnetically or mechanically activated implant (e.g. cardiac pacemaker, insulin pump biostimulator, neurostimulator, cochlear implant, and hearing aids)
- Intracranial aneurysm clips (unless made of titanium)
- Pregnancy (risk vs benefit ratio to be assessed)
- Ferromagnetic surgical clips or staples
- Metallic foreign body in the eye
- Metal shrapnel or bullet
Patient preparation
- A satisfactory written consent form must be taken from the patient before entering the scanner room
- Ask the patient to remove all metal objects including keys, coins, wallet, cards with magnetic strips, jewellery, hearing aid and hairpins
- Ask the patient to undress and change into a hospital gown
- Instruct the patient to breathe gently during the gated scans.
- An intravenous line must be placed with extension tubing extending out of the magnetic bore
- Claustrophobic patients may be accompanied into the scanner room e.g. by staff member or relative with proper safety screening
- Offer headphones for communicating with the patient and ear protection
- Explain the procedure to the patient and answer questions
- Note down the weight of the patient
Positioning
- Position the patient in supine position with head pointing towards the magnet (head first supine)
- Position the patient over the spine coil and place the body coil over the upper abdomen (nipple down to iliac crest)
- Securely tighten the body coil using straps to prevent respiratory artefacts
- Give a pillow under the head and cushions under the legs for extra comfort
- Centre the laser beam localizer over xiphoid process of sternum

Suggested protocols, parameters and planning
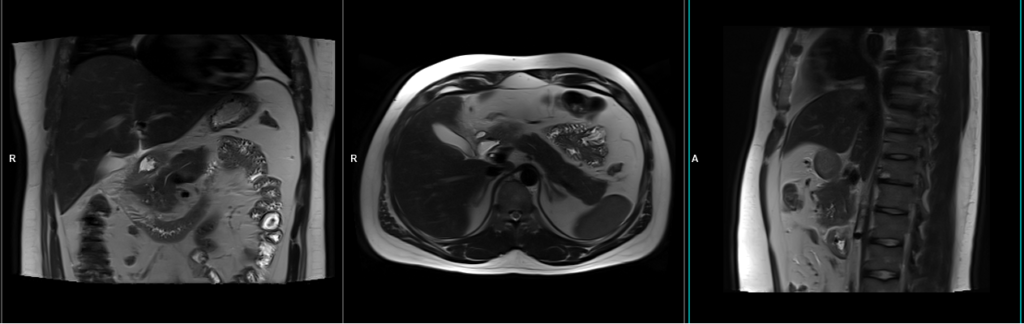
localiser free breathing
To localize and plan the sequences, it is essential to acquire a three-plane T2 HASTE localizer initially. These fast single-shot localizers have an acquisition time of under 25 seconds and are highly effective in accurately localizing abdominal structures.
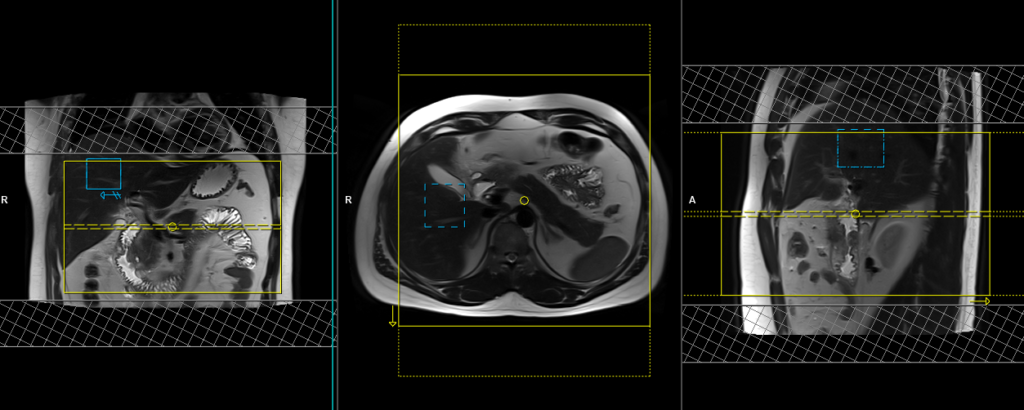
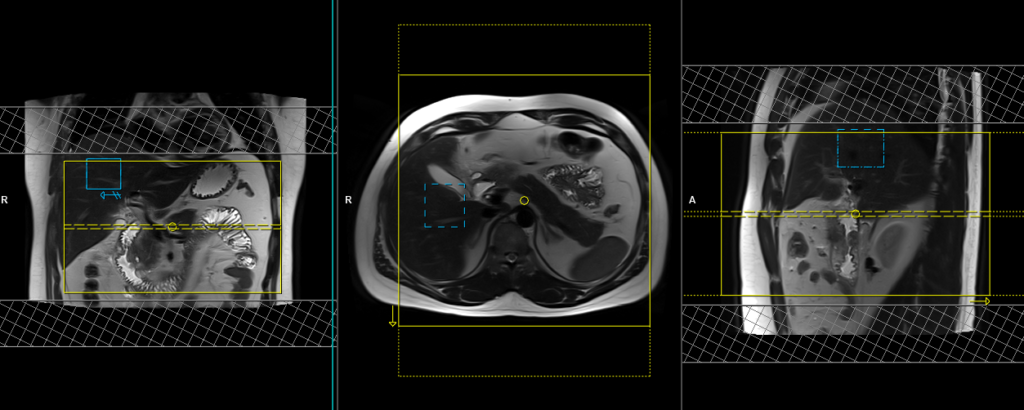
T2 HASTE coronal 4mm sfov respiratory gated
Plan the coronal slices using the axial localizer and position the block horizontally across the abdomen as shown. Verify the position in the other two planes. Establish an appropriate angle in the sagittal plane, aligning it vertically across the abdomen. Ensure that the slices adequately cover the entire pancreas, extending from the anterior abdominal wall to the vertebral body. The phase direction should be from right to left to minimize ghosting artifacts from the lungs and heart. Employ phase oversampling to prevent wrap-around artifacts. Additionally, consider adding saturation bands at the top and bottom of the block to minimize artifacts caused by fat signal, arterial pulsation, and breathing. Instruct the patient to breathe gently throughout the sequence, as very shallow or erratic breathing can diminish the effectiveness of the navigator.
In modern scanners, respiratory gating is achieved using phase scout navigators placed inside the liver tissues. In older generation scanners, the liver dome respiratory trigger method can be utilized. However, in our department, we prefer using phase scout navigators. For respiratory gated scans utilizing phase scout navigators, it is essential to accurately position the respiratory navigator box within the liver. Ensure that no part of the navigation box extends beyond the liver boundaries. Planning should be conducted using a free breathing localizer, as the diaphragm’s downward movement during inhalation can result in improper slice planning and positioning of the respiratory navigator box.

Parameters
TR 2000-2500 | TE 90-110 | FLIP 130 | NEX 1 | SLICE 4MM | MATRIX 256×256 | FOV 280 | PHASE R>L | OVERSAMPLE 50% | TRIGGER Yes |
Phase scout respiratory gating
Phase scout respiratory gating is a technique used to synchronize image acquisition with the patient’s respiratory motion. It involves acquiring a low-resolution, single-shot MR image during free breathing, referred to as a phase scout or navigator scan. This scout image is typically acquired in the liver region, as it exhibits prominent respiratory motion.
The acquired phase scout image is used to track the patient’s respiratory motion by monitoring changes in the position of anatomical structures, such as the diaphragm or liver dome, between successive acquisitions. The position information is then used to trigger the start of image acquisition at specific phases of the respiratory cycle, typically during end-expiration when motion artifacts are minimal.
By employing phase scout respiratory gating, scanner can acquire images at specific respiratory phases, resulting in reduced motion artifacts and improved image quality. This technique is particularly beneficial when imaging anatomical regions affected by respiratory motion, such as the liver, allowing for clearer and more accurate diagnostic images.

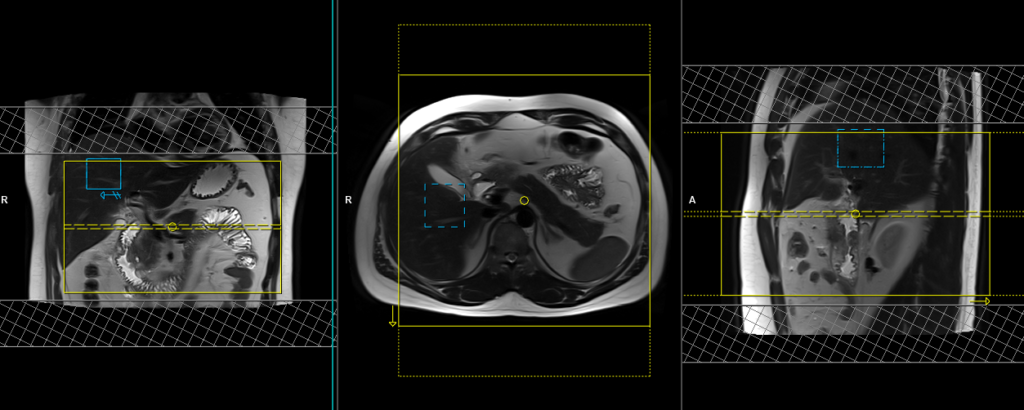
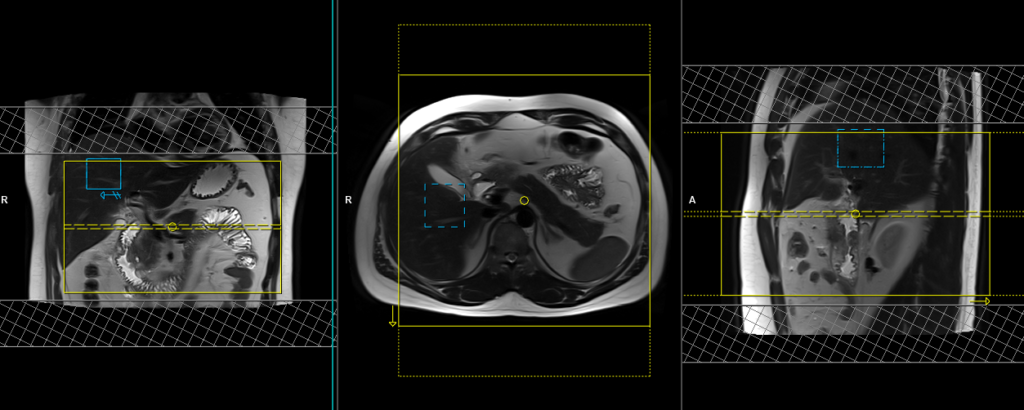
T2 BLADE\HASTE 4mm respiratory gated
Plan the axial slices on the coronal respiratory-gated images and position the block horizontally across the abdomen, as shown. Verify the positioning in the other two planes. Establish an appropriate angle in the sagittal plane, aligning it horizontally across the abdomen. The slices should sufficiently cover the entire pancreas, starting one inch above the pancreatic tail and extending down to the C loop of the duodenum. The phase direction should be from right to left to minimize ghosting artifacts from the anterior abdominal wall. Use phase oversampling to prevent wrap-around artifacts. Consider adding saturation bands at the top and bottom of the block to minimize artifacts caused by fat signal, arterial pulsation, and breathing. Instruct the patient to hold their breath during image acquisition. Instruct the patient to breathe gently throughout the scan.
Parameters HASTE
TR 2000-2500 | TE 90-110 | FLIP 130 | NEX 1 | SLICE 4MM | MATRIX 256×256 | FOV 280 | PHASE R>L | OVERSAMPLE 50% | TRIGGER Yes |
T2 BLADE\HASTE fat saturated 4mm respiratory gated
Plan the axial slices on the coronal respiratory-gated images and position the block horizontally across the abdomen, as shown. Verify the positioning in the other two planes. Establish an appropriate angle in the sagittal plane, aligning it horizontally across the abdomen. The slices should sufficiently cover the entire pancreas, starting one inch above the pancreatic tail and extending down to the C loop of the duodenum. The phase direction should be from right to left to minimize ghosting artifacts from the anterior abdominal wall. Use phase oversampling to prevent wrap-around artifacts. Consider adding saturation bands at the top and bottom of the block to minimize artifacts caused by fat signal, arterial pulsation, and breathing. Instruct the patient to hold their breath during image acquisition. Instruct the patient to breathe gently throughout the scan.
Parameters HASTE FS
TR 2000-2500 | TE 90-110 | FAT SAT SPAIR | NEX 1 | SLICE 4MM | MATRIX 256×256 | FOV 280 | PHASE R>L | OVERSAMPLE 50% | TRIGGER Yes |
T1 In-phase 4mm respiratory gated 4mm
Plan the axial slices on the coronal respiratory-gated images and position the block horizontally across the abdomen, as shown. Verify the positioning in the other two planes. Establish an appropriate angle in the sagittal plane, aligning it horizontally across the abdomen. The slices should sufficiently cover the entire pancreas, starting one inch above the pancreatic tail and extending down to the C loop of the duodenum. The phase direction should be from right to left to minimize ghosting artifacts from the anterior abdominal wall. Use phase oversampling to prevent wrap-around artifacts. Consider adding saturation bands at the top and bottom of the block to minimize artifacts caused by fat signal, arterial pulsation, and breathing. Instruct the patient to hold their breath during image acquisition. Instruct the patient to breathe gently throughout the scan.
Parameters
TR 2000 | TE 1.44 | FLIP 15 | NXA 1 | SLICE 4 MM | MATRIX 256×224 | FOV 280 | PHASE A>P | OVERSAMPLE 20% | TI 700 |
T1 out-of-phase respiratory gated 4mm
Plan the axial slices on the coronal respiratory-gated images and position the block horizontally across the abdomen, as shown. Verify the positioning in the other two planes. Establish an appropriate angle in the sagittal plane, aligning it horizontally across the abdomen. The slices should sufficiently cover the entire pancreas, starting one inch above the pancreatic tail and extending down to the C loop of the duodenum. The phase direction should be from right to left to minimize ghosting artifacts from the anterior abdominal wall. Use phase oversampling to prevent wrap-around artifacts. Consider adding saturation bands at the top and bottom of the block to minimize artifacts caused by fat signal, arterial pulsation, and breathing. Instruct the patient to hold their breath during image acquisition. Instruct the patient to breathe gently throughout the scan.
Parameters
TR 2000 | TE 2.31 | FLIP 15 | NXA 1 | SLICE 4 MM | MATRIX 256×224 | FOV 280 | PHASE A>P | OVERSAMPLE 20% | TI 900 |
DWI epi 3 scan trace axial 4mm free breathing
Plan the axial slices on the coronal respiratory-gated images and position the block horizontally across the abdomen, as shown. Verify the positioning in the other two planes. Establish an appropriate angle in the sagittal plane, aligning it horizontally across the abdomen. The slices should sufficiently cover the entire pancreas, starting one inch above the pancreatic tail and extending down to the C loop of the duodenum. The phase direction should be from right to left to minimize ghosting artifacts from the anterior abdominal wall. Use phase oversampling to prevent wrap-around artifacts. Consider adding saturation bands at the top and bottom of the block to minimize artifacts caused by fat signal, arterial pulsation, and breathing. Instruct the patient to hold their breath during image acquisition. Instruct the patient to breathe gently throughout the scan.

Parameters
TR 6000-7000 | TE 90 | IPAT ON | NEX 3 5 8 | SLICE 4 MM | MATRIX 192X192 | FOV 300-330 | PHASE R>L | GAP 10% | B VALUE 0 |
T2 tse coronal 3D fat sat 1mm respiratory gated
Plan the coronal slices based on the axial images, angling the position parallel to the pancreatic body. Verify the position in the other two planes. Establish an appropriate angle in the sagittal plane, aligning it vertically across the abdomen. Ensure that the slices are sufficient to cover the entire pancreas from head to tail.
For respiratory gating scans, it is important to correctly position the respiratory navigator box. Place it in the middle of the right dome of the diaphragm, with half of the box over the right lobe of the liver (segment 8) and the other half over the lungs. Planning should be done using a non-breath-hold localizer, as the diaphragm will push down the liver during inhalation, leading to improper planning of slices and the respiratory navigator box.
It is important to instruct the patient to breathe gently throughout the sequence. The effectiveness of the navigator will be reduced with very shallow or erratic breathing.

Navigators:-
Recently, navigators have been introduced in order to enable motion-free scans of the abdomen and chest, eliminating the presence of artifacts caused by motion. A navigator is a periodic two-dimensional pulse that excites a group of spins, followed by a readout gradient along the long axis of the group to obtain a one-dimensional profile of the region of interest. This imaging sequence utilizes a low flip angle (10) to minimize signal saturation, and the abrupt change in signal intensity between the lungs and liver is utilized to determine the position of the diaphragm. The navigator pulse has a duration of approximately 20 milliseconds and is executed every 200 milliseconds. A scan acceptance window is determined based on preliminary pre-scan data, after which the actual scan acquisition begins. During each slice acquisition, the navigation box detects the position of the diaphragm, and imaging only takes place when the diaphragm falls within the acceptance window.
Parameters
TR 3000-4000 | TE 90 | FLIP 140 | NEX 1 | SLICE 1MM | MATRIX 256×256 | FOV 300 | PHASE R>L | OVERSAMPLE 100% | TRIGGER YES |
T1 Compressed Sensing GRASP-VIBE axial Dynamic free breathing
Compressed Sensing GRASP-VIBE is an innovative MRI technique that combines Compressed Sensing (CS) and GRASP-VIBE (Golden-angle Radial Sparse Parallel MRI with View-sharing) to transform abdominal imaging. The dynamic liver sequence of Compressed Sensing GRASP-VIBE comprises multiple scans with high temporal resolution and incorporates motion correction. The entire sequence lasts approximately 5 minutes and includes one pre-contrast acquisition followed by several post-contrast acquisitions.
During the scan, the scanner provides a 20-second countdown for the administration of contrast injection. Within this timeframe, the scanner performs the pre-contrast scans. As a user, you simply need to initiate the sequence, monitor the countdown, and administer the contrast agent once the countdown concludes. This streamlined process minimizes user involvement, allowing for efficient and hassle-free implementation of the technique.
Plan the axial slices on the coronal breath hold images and position the block horizontally across the liver as shown. Verify the positioning in the other two planes. Establish an appropriate angle in the sagittal plane, aligning it horizontally across the liver. The slices must be sufficient to cover the entire liver from the diaphragm down to the C loop of the duodenum. Use phase oversampling to prevent wrap-around artifacts.

Parameters
TR 4-5 | TE 2 | FLIP 12 | NEX 1 | SLICE 3MM | MATRIX 256X256 | FOV 320 | PHASE A>P | DYNAMIC | IPAT ON |
Compressed Sensing GRASP-VIBE
Compressed Sensing GRASP-VIBE combines the principles of Compressed Sensing and GRASP-VIBE to revolutionize abdominal MRI. This technique allows for high-resolution dynamic abdominal imaging under free-breathing conditions, expanding the patient population eligible for the procedure. Patients who have limited breath-hold capability or difficulty following breathing commands can now undergo this exam with ease.
With its intelligent reconstruction and processing framework, Compressed Sensing GRASP-VIBE automatically identifies different phases of liver dynamics and outputs only the clinically relevant information. This streamlines the workflow and brings the advantages of this technique to daily clinical routines.
The acquisition is performed in one continuous run using a golden-angle stack-of-stars radial scheme, providing robustness against motion and the flexibility to choose temporal resolution. Reconstruction utilizes a Compressed Sensing GPU accelerated iterative algorithm with through-time regularization, resulting in improved image quality. This combination enables free-breathing abdominal exams with both diagnostic image quality and high temporal resolution to capture dynamic contrast enhancement phases.
Additional features include auto bolus detection, configuration of exam phases, auto-labeling of relevant phases, self-gating for further motion reduction, and inline reconstruction using GPU acceleration for quick image access. Compressed Sensing GRASP-VIBE offers protocols for both abdomen and prostate imaging, making it a versatile technique.
Optional Scans
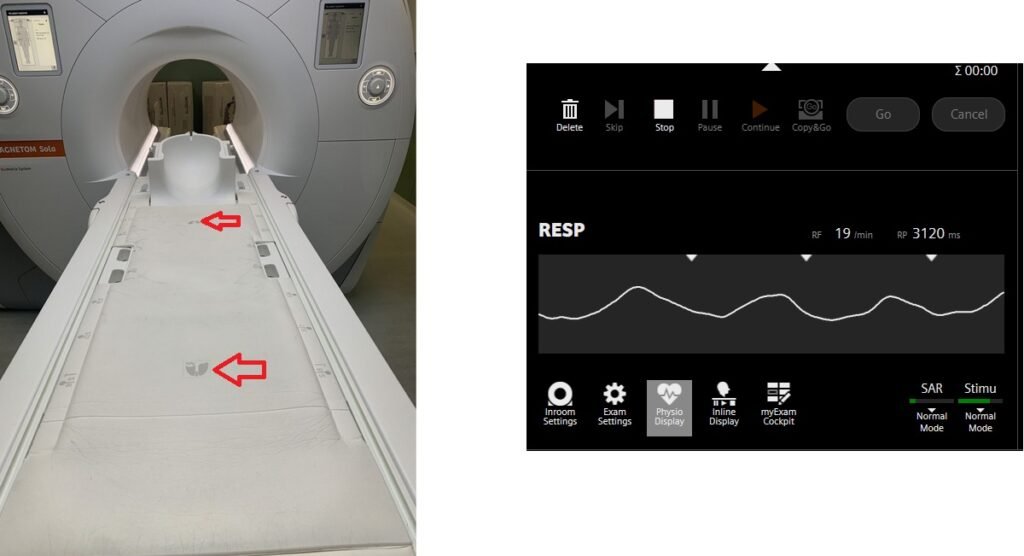
T2 HASTE axial 4 mm respiratory gated using table respiratory sensor
Respiratory gating in modern scanners can now be accomplished using built-in table respiratory sensors. This feature proves particularly beneficial when patients have irregular breathing patterns or are at risk of falling asleep during the scan. The advantage of table sensors is that they do not necessitate any specific planning. The only requirement is to ensure that the patient’s chest is accurately positioned over the table sensors to enable accurate monitoring of breathing. Additionally, it is important to select the appropriate gating option, such as the table sensor gating, in the protocol settings.
Plan the axial slices on the coronal respiratory-gated images and position the block horizontally across the abdomen, as shown. Verify the positioning in the other two planes. Establish an appropriate angle in the sagittal plane, aligning it horizontally across the abdomen. The slices should sufficiently cover the entire pancreas, starting one inch above the pancreatic tail and extending down to the C loop of the duodenum. The phase direction should be from right to left to minimize ghosting artifacts from the anterior abdominal wall. Use phase oversampling to prevent wrap-around artifacts. Consider adding saturation bands at the top and bottom of the block to minimize artifacts caused by fat signal, arterial pulsation, and breathing. Instruct the patient to hold their breath during image acquisition. Please advise the patient to maintain a gentle and steady breathing pattern throughout the entire scan.

Parameters
TR 2000-3000 | TE 130 | FLIP 150 | NEX 1 | SLICE 4MM | MATRIX 288X256 | FOV 280-320 | PHASE R>L | OVERSAMPLE 50% | IPAT ON |
Table sensors
Advanced MRI scanners are equipped with built-in table sensors that detect the respiratory waveform and trigger data acquisition during the expiration phase of the respiratory cycle. Proper patient positioning over the sensor is critical for accurate respiratory gating. This method eliminates the need for external respiratory gating equipment, such as sensors and belts.