Endometriosis MRI Protocol and Planning
Endometriosis
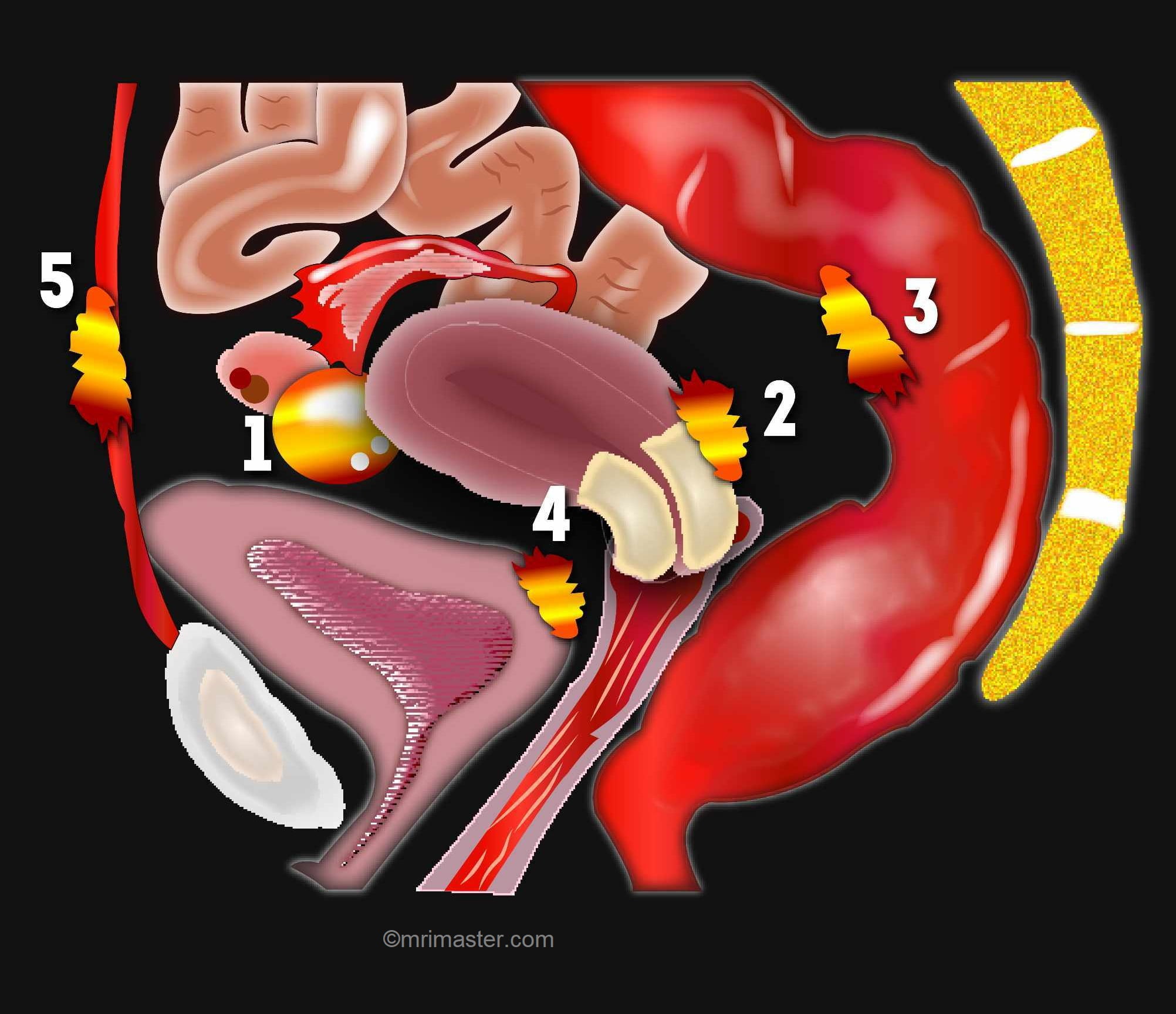
Endometriosis is a complex and chronic gynecological condition that impacts numerous women globally. It is characterized by the abnormal growth of endometrial tissue beyond the uterus, commonly found in the pelvic region, ovaries, fallopian tubes, and even in remote organs like the intestines or lungs. This displaced tissue reacts to hormonal changes, resulting in inflammation, pain, and the development of adhesions.
The symptoms of endometriosis can vary significantly and encompass pelvic pain, dysmenorrhea, dyspareunia, infertility, as well as gastrointestinal or urinary disturbances. It’s important to note that some women may experience minimal symptoms or remain asymptomatic.
Diagnosing endometriosis typically involves a comprehensive approach that combines clinical assessment, imaging techniques such as ultrasound, and laparoscopic surgery accompanied by a biopsy. Early detection plays a critical role in preventing disease progression and minimizing associated complications.
Treatment options for endometriosis span from pain management using nonsteroidal anti-inflammatory drugs (NSAIDs) to hormonal therapies like oral contraceptives, progestins, or gonadotropin-releasing hormone (GnRH) agonists. In severe cases or when fertility is affected, surgical intervention may be necessary to excise endometrial implants or adhesions.
Endometriosis MRI is an invaluable diagnostic modality for assessing endometriosis. By offering precise imaging of the pelvic area, it enables the accurate visualization and evaluation of endometrial lesions and their extent.
The significance of MRI becomes particularly apparent when endometriosis is suspected but not easily detectable using alternative imaging techniques. It proves highly effective in identifying deep infiltrating lesions that may affect structures like the bowel, bladder, and ureters. Additionally, MRI assists in assessing the severity of endometriosis, ascertaining the presence of adhesions, and determining the involvement of adjacent organs.
Indications for Endometriosis MRI Scan
- Long-term lower back and pelvic pain
- Endometriosis
- Heavy menstrual bleeding
Contraindications
- Any electrically, magnetically or mechanically activated implant (e.g. cardiac pacemaker, insulin pump biostimulator, neurostimulator, cochlear implant, and hearing aids)
- Intracranial aneurysm clips (unless made of titanium)
- Pregnancy (risk vs benefit ratio to be assessed)
- Ferromagnetic surgical clips or staples
- Metallic foreign body in the eye
- Metal shrapnel or bullet
Patient preparation for Endometriosis MRI Scan
- A satisfactory written consent form must be taken from the patient before entering the scanner room
- Ask the patient to remove all metal objects including keys, coins, wallet, cards with magnetic strips, jewellery, hearing aid and hairpins
- Ask the patient to undress and change into a hospital gown
- Buscopan injection risk and benefits must be explained to the patient before the scan
- Claustrophobic patients may be accompanied into the scanner room e.g. by staff member or relative with proper safety screening
- Offer earplug or headphones possibly with music for extra comfort.
- Explain the procedure to the patient and answer questions
- Note down the weight of the patient
Positioning for Endometriosis MRI Scan
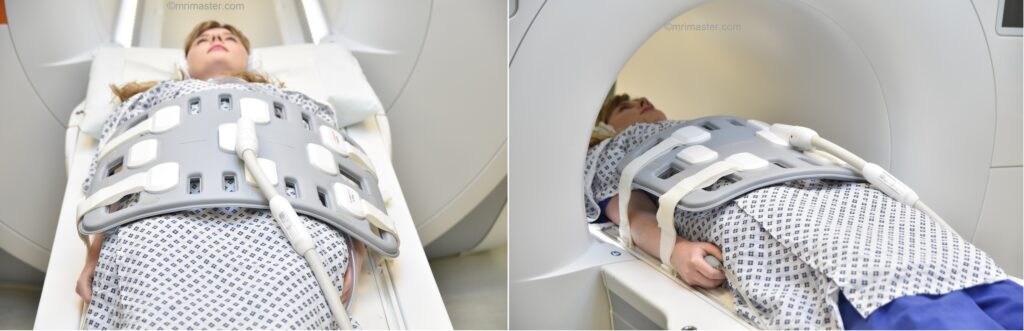
- Position the patient in supine position with head pointing towards the magnet (head first supine)
- Position the patient over the spine coil and place the body coil over abdomen and pelvis (nipple down to three inches below symphysis pubis)
- Securely tighten the body coil using straps to prevent respiratory artefacts
- Give a pillow under the head and cushions under the legs for extra comfort
- Centre the laser beam localiser over the iliac crest
- Register the patient in the scanner as head first supine
Recommended Endometriosis MRI Protocols and Planning
Endometriosis MRI Scan localiser
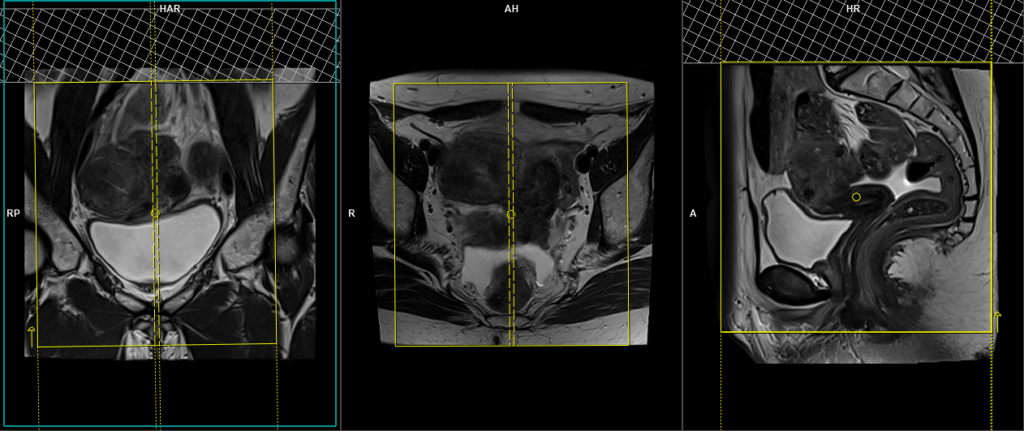
A three-plane localiser must be taken at the beginning to localise and plan the sequences. Localisers are normally less than 25 seconds and are T2-weighted low-resolution scans.

Pause for buscopan injection
Warning
* Buscopan injection should not be administered to patients with myasthenia gravis, megacolon, narrow angle glaucoma, tachycardia, prostatic enlargement with urinary retention, mechanical stenoses in the region of the gastrointestinal tract or paralytic ileus.*
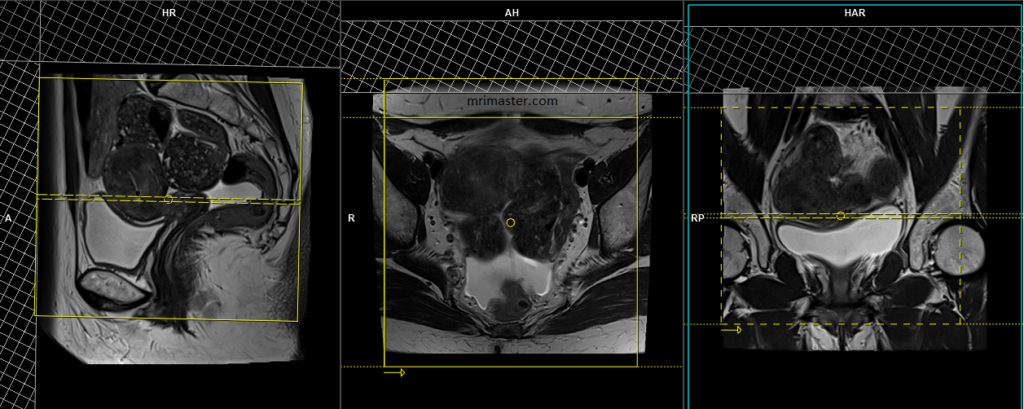
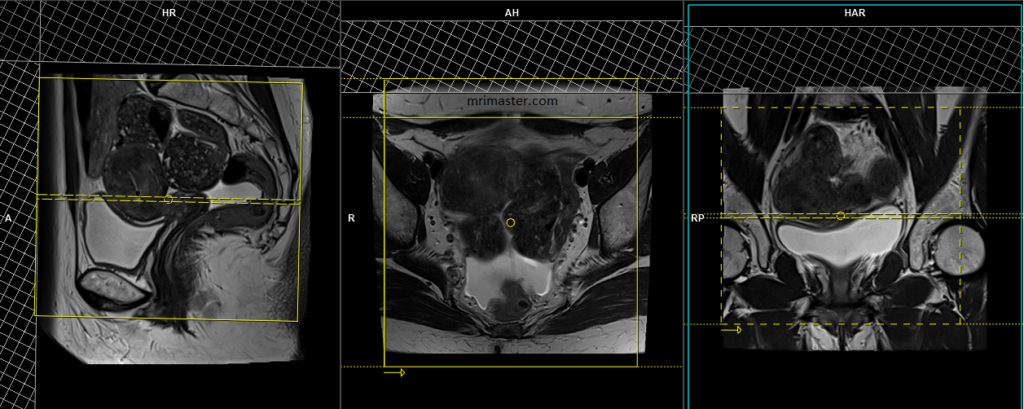
T2 tse sagittal 3mm SFOV
Plan the sagittal slices on the axial plane and align the positioning block parallel to the linea alba and median sacral crest. Verify the positioning block in the other two planes. In the coronal plane, ensure an appropriate angle that parallels the lumbosacral spine. Make sure that the slices cover the entire pelvis, ranging from the right acetabulum to the left acetabulum. The field of view (FOV) should be sufficiently large to encompass the fibroids, typically ranging from 270mm to 300mm. To minimize artifacts caused by arterial pulsation, peristalsis, and breathing, consider adding saturation bands on top and in front of the sagittal block. Ensure an adequate level of phase oversampling to prevent any wrap-around artifacts.
Due to the increased signal-to-noise ratio (SNR) in new generation scanners, motion artifacts can be significant when acquiring images in the anterior-posterior phase direction. This is primarily attributed to the movement of abdominal fat, which exhibits higher signal intensity and can cause ghosting effects over the sagittal images. Therefore, to mitigate this issue, scans are typically performed using a head-to-feet phase direction.
Parameters
TR 4000-6000 | TE 100-120 | SLICE 3 MM | FLIP 130-150 | PHASE H>F | MATRIX 320X320 | FOV 270-300 | GAP 10% | NEX(AVRAGE) 3 |
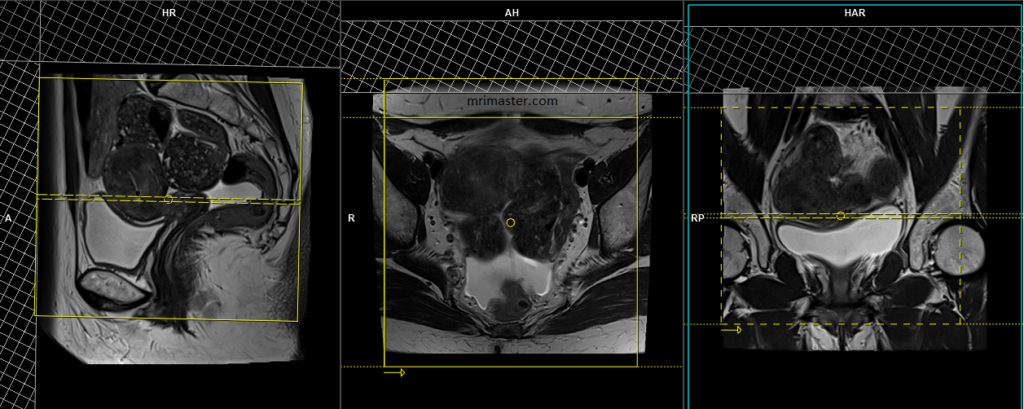
T2 tse axial 3mm SFOV pelvis
Plan the axial slices on the sagittal plane and position the block horizontally across the pelvis. Verify the positioning block in the other two planes. Determine an appropriate angle in the coronal plane that is parallel to the right and left hip. Ensure that the slices adequately cover the entire pelvis from the pubic symphysis to the L5-S1 disc. To minimize artifacts caused by arterial pulsation and breathing, consider adding saturation bands on top and in front of the axial block.
In modern scanners, the anterior-posterior phase direction can result in noticeable motion artifacts. This is due to the enhanced signal-to-noise ratio (SNR) and increased signal intensity in abdominal fat. As the abdominal fat moves during the acquisition, it can cause ghosting effects on the axial images. To mitigate this issue, axial scans are typically performed using a right-to-left phase direction.
Parameters
TR 5000-6000 | TE 100-120 | SLICE 3 MM | FLIP 130-150 | PHASE R>L | MATRIX 320X320 | FOV 200-230 | GAP 10% | NEX(AVRAGE) 4 |
T1 tse fat sat axial 3mm SFOV PELVIS
Plan the axial slices on the sagittal plane and position the block horizontally across the pelvis. Verify the positioning block in the other two planes. Determine an appropriate angle in the coronal plane that is parallel to the right and left hip. Ensure that the slices adequately cover the entire pelvis from the pubic symphysis to the L5-S1 disc. To minimize artifacts caused by arterial pulsation and breathing, consider adding saturation bands on top and in front of the axial block.
Parameters
TR 400-650 | TE 15-25 | SLICE 3 MM | FLIP 130 | PHASE R>L | MATRIX 256X256 | FOV 200-230 | GAP 10% | NEX(AVRAGE) 4 |
DWI epi 3 scan trace axial 3mm SFOV PELVIS
Plan the axial slices on the sagittal plane and position the block horizontally across the pelvis. Verify the positioning block in the other two planes. Determine an appropriate angle in the coronal plane that is parallel to the right and left hip. Ensure that the slices adequately cover the entire pelvis from the pubic symphysis to the L5-S1 disc. To minimize artifacts caused by arterial pulsation and breathing, consider adding saturation bands on top and in front of the axial block.
Parameters
TR 6000-7000 | TE 90 | IPAT ON | NEX 3 5 8 | SLICE 3 MM | MATRIX 192X192 | FOV 200-250 | PHASE R>L | GAP 10% | B VALUE 0 |
T2 tse coronal 3mm SFOV pelvis
Plan the coronal slices on the sagittal plane and position the block vertically across the pelvis. Verify the positioning block in the other two planes. Provide an appropriate angle in the axial plane that is parallel to the right and left hip. Ensure that the slices adequately cover the entire pelvis, from the anterior abdominal wall to the sacrum. Adding saturation bands on top and in front of the coronal block will help reduce artifacts caused by arterial pulsation and breathing.
Parameters
TR 5000-6000 | TE 100-120 | SLICE 3 MM | FLIP 130-150 | PHASE R>L | MATRIX 320X320 | FOV 200-230 | GAP 10% | NEX(AVRAGE) 4 |
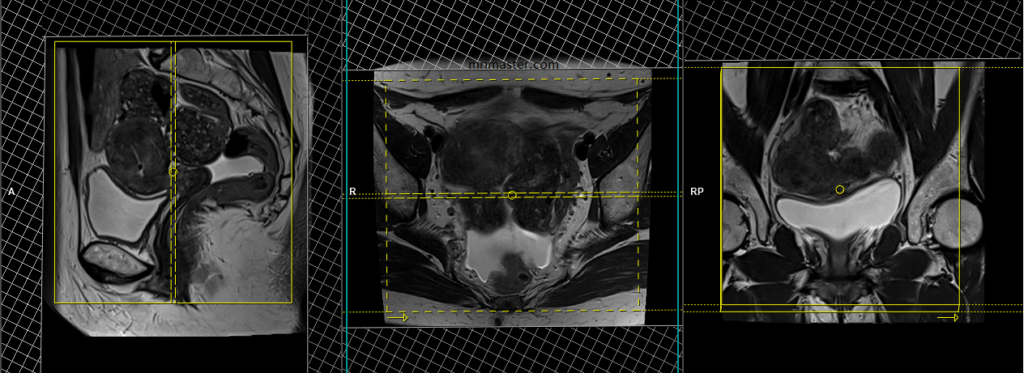
T2 stir coronal 5 mm big FOV
Plan the large field of view (FOV) coronal slices on the sagittal plane and position the block parallel to the lumbar spine. Verify the positioning block in the other two planes as well. Establish an appropriate angle in the axial plane, which runs parallel to the right and left hip joint. The slices should adequately cover the entire abdomen and pelvis, extending from the anterior abdominal wall to the sacrum. The FOV must be large enough to encompass the abdomen and pelvis, typically ranging from 380mm to 400mm. Large FOV scans are usually performed to evaluate the local spread of the pathology and assess the para-aortic and pre-sacral nodes.

Parameters
TR 4000-5000 | TE 110 | FLIP 130 | NEX 2 | SLICE 5MM | MATRIX 384X320 | FOV 380-400 | PHASE R>L | GAP 10% | TI 130 |
T2 tse axial 6 mm large FOV
Plan the large field of view (FOV) axial slices on the coronal plane, positioning the block parallel to the line along the right and left iliac crest. Verify the positioning block in the other two planes as well. Establish an appropriate angle in the sagittal plane, perpendicular to the lumbar spine. The slices should adequately cover the entire lower abdomen and pelvis, extending from the middle of the kidneys down to the symphysis pubis. The FOV should be large enough to encompass the entire pelvis, typically ranging from 350mm to 400mm. To reduce artifacts caused by arterial pulsation and breathing, consider adding saturation bands on top of the axial block. Large FOV scans are usually performed to assess the local spread, para-aortic, and pre-sacral nodes.

Parameters
TR 5000-6000 | TE 100-120 | SLICE 6 MM | FLIP 130-150 | PHASE R>L | MATRIX 384X384 | FOV 350-400 | GAP 10% | NEX(AVRAGE) 2 |
