Peripheral MRA(MRA Legs) : Protocol and Planning
Indications for MRA(magnetic resonance angiography) legs
- Peripheral arterial occlusive disease
- Post operative and stent evaluation
- Arteriovenous malformation
- Chronic critical ischemia
- Chronic arterial disease
- Acute arterial disease
- Congenital disorders
- Aortoiliac disease
- Embolic disease
- Runoff disease
Please check our new video tutorial for protocols and planning
Contraindications
- Any electrically, magnetically or mechanically activated implant (e.g. cardiac pacemaker, insulin pump biostimulator, neurostimulator, cochlear implant, and hearing aids)
- Intracranial aneurysm clips (unless made of titanium)
- Pregnancy (risk vs benefit ratio to be assessed)
- Ferromagnetic surgical clips or staples
- Metallic foreign body in the eye
- Metal shrapnel or bullet
Patient preparation for peripheral MRA
- A satisfactory written consent form must be taken from the patient before entering the scanner room
- Ask the patient to remove all metal object including keys, coins, wallet, any cards with magnetic strips, jewellery, hearing aid and hairpins
- Ask the patient to undress and change into a hospital gown
- Instruct the patient to hold their breath for the breath hold scans (its better to coach the patient two to three times before starting the scan)
- An intravenous line must be placed with extension tubing extending out of the magnetic bore
- Contrast injection risk and benefits must be explained to the patient before the scan
- Gadolinium should only be given to the patient if GFR is > 30
- Claustrophobic patients may be accompanied into the scanner room e.g. by staff member or relative with proper safety screening
- Offer headphones for communicating with the patient and ear protection
- Explain the procedure to the patient and answer questions
- Note down the weight of the patient
Positioning for peripheral MRA
- Position the patient in supine position with feet pointing towards the magnet (feet first supine)
- Position the patient over the spine coil and place the peripheral coil over the legs and two body coils over the abdomen and chest
- Give cushions under the head for extra comfort
- Centre the laser beam localiser over mid lower leg

Recommended Peripheral MRA Protocols and Planning
localiser MRA lower leg
A three plane T1 localiser must be taken initially to localise and plan the sequences. These are fast single shot T1 scans with aqusition time under 25s, which are excellent for localising. Peripheral MRA Protocol should be setup with an auto move of the table after the lower leg localiser acquisition. Usually, in MRA leg protocols an auto move of 380-420 mm set by default, that means after the lower leg localiser table will automatically move towards the feet for the upper leg scans.

localizer MRA upper leg
A three plane T1 localizer must be taken in the upper leg to localize and plan the sequences.

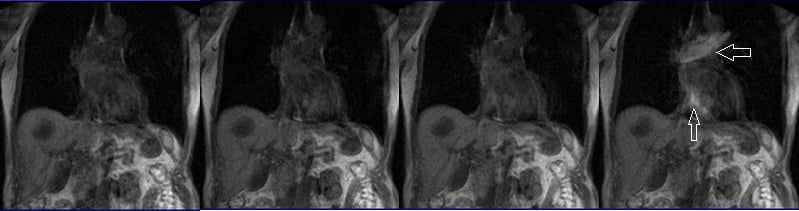
Phase contrast(PC) vessel localiser upper leg

localiser MRA abdomen
A three plane T1 localiser must be taken in the abdomen to localise and plan the sequences.

Phase contrast (PC) vessel localiser abdomen
A Sagittal Phase contrast vessel localiser must be taken in the abdomen for further localisation and planning of the coronal 3D flash sequence. Phase contrast localisers are fast scans with acquisition time less than 1minute, which are excellent for localising vascular structures.

T1 flash 3D coronal 0 .9mm -1.1mm pre-contrast abdomen
Plan the coronal slices on the sagittal Phase contrast vessel localiser; angle the position block parallel to the aorta. Check the positioning block in the other two planes. An appropriate angle must be used in the axial plane (parallel to the long axia of both kidneys). Slices must be sufficient to cover the aorta and iliac arteries. The FOV must be big enough to cover the vessels from the heart to femoral arteries. Enough phase oversampling and slice oversample must be used to avoid wrap- around artifacts. Instruct the patient to hold their breath during image acquisition. (In our department we instruct the patients to breathe in and out twice before the ‘breath in and hold’ instruction). It is highly advisable to use Parallel acquisition technique to reduce the scan time (scan time should be less than 20 seconds to get the best results). Protocol should be setup with an auto move of the table after the abdominal 3D flash acquisition.

Parameters
TR 2-3 | TE 1-2 | FLIP 20 | NEX 1 | SLICE 1 MM | MATRIX 384×384 | FOV 450-470 | PHASE R>L | OVERSAMPLE 50% | IPAT OFF |
Parallel acquisition technique(IPAT)
Parallel imaging is a newly developed technique used to reduce scan time without affecting the scan resolution. Using parallel acquisition MRI techniques, it is possible to reconstruct full-FOV images from under sampled k-space data by using the uncorrelated information from RF array coil elements. The main disadvantage of parallel acquisition techniques is the signal-to-noise ratio (SNR) is degraded because of the reduced data samples and the spatially correlated nature of multiple RF receivers.
T1 flash 3D coronal .9mm -1.1mm pre-contrast upper leg
Plan the coronal slices on the sagittal Phase contrast vessel localiser; angle the position block parallel to the femoral artery. Check the positioning block in the other two planes. An appropriate angle must be given in the axial plane (parallel to the right and left femur). Slices must be sufficient to cover the femoral arteries .FOV must be big enough to cover the vessels from iliac arteries down to popliteal arteries . Phase oversampling and slice oversample, must be used to avoid wrap around artefacts. It’s important to overlap the abdominal and femoral blocks by 1 to 2 centimetres to avoid any misregistration. It is highly advisable to use Parallel acquisition technique to reduce the scan time (scan time should be less than 15 seconds to get best results). Protocol should be setup with an auto move of the table after the upper leg 3D flash acquisition.

Parameters
TR 2-3 | TE 1-2 | FLIP 20 | NEX 1 | SLICE 1 MM | MATRIX 384×384 | FOV 450-470 | PHASE R>L | OVERSAMPLE 30% | IPAT OFF |
T1 flash 3D coronal 1mm -1.3mm pre-contrast lower leg
Plan the coronal slices on the sagittal localiser; angle the position block parallel to the tibia. Check the positioning block in the other two planes. An appropriate angle must be given in the axial plane (parallel to the right and left tibia). Slices must be sufficient to cover the whole lower leg .FOV must be big enough to cover the vessels from knee joint down to ankle joint . Phase oversampling and slice oversample, must be used to avoid wrap around artefacts. It’s important to overlap the upper leg and lower leg blocks by 1 to 2 centimetres to avoid any misregistration. It is highly advisable to use Parallel acquisition technique to reduce the scan time (scan time should be less than 15 seconds to get best results).

Parameters
TR 2-3 | TE 1-2 | FLIP 20 | NEX 1 | SLICE 1 MM | MATRIX 384×384 | FOV 450-470 | PHASE R>L | OVERSAMPLE 30% | IPAT OFF |
contrast administration and timing of scans
Guess timing technique:-
This is one of the simplest methods. It works by estimating the time of contrast travel from the site of injection to the vascular structure of abdomen. This technique is highly dependent upon the site of contrast injection, age of the patient, cardiac output, and vascular anatomy. Generally the contrast takes about 15-20 seconds to travel from the antecubital vein to the arch of aorta. Therefore the post contrast T1 acquisition should start within 15s of contrast administration.
Care bolus technique:-
Care bolus is the most commonly used bolus detection technique. This technique uses a coronal fast gradient refocused sequence. Real-time images are obtained every second through the vascular structure of interest (normally placed over the heart). The operator can then watch the contrast bolus arriving in the heart and then switch to the centric 3D sequence.
Planning care bolus
Plan the coronal care bolus slice on the sagittal plane; angle the slice parallel to the ascending aorta. Check the positioning block in the other two planes.

Care bolus scans must start one second prior to the contrast administration. The operator can then watch the scans live and wait for the contrast bolus to arrive in the heart. When the contrast reaches the heart the care bolus must be stopped immediately and the patient instructed to hold their breath before starting the centric 3D dynamic sequence.
T1 flash 3D coronal 0 .9mm -1.1mm post-contrast abdomen
Plan the coronal slices on the sagittal Phase contrast vessel localiser; angle the position block parallel to the aorta. Check the positioning block in the other two planes. An appropriate angle must be given in the axial plane (parallel to the right and left kidneys). Slices must be sufficient to cover the aorta and iliac arteries .FOV must be big enough to cover the vessels from heart down to femoral arteries . Phase oversampling and slice oversample, must be used to avoid wrap around artefacts. Instruct the patient to hold their breath during image acquisition. (In our department we instruct the patients to breath in and out twice before the “breath in and hold” instruction.).It is highly advisable to use Parallel acquisition technique to reduce the scan time (scan time should be less than 20 seconds to get best results). Protocol should be setup with an auto move of the table after the abdominal 3D flash acquisition.

Parameters
TR 2-3 | TE 1-2 | FLIP 20 | NEX 1 | SLICE 1 MM | MATRIX 384×384 | FOV 450-470 | PHASE R>L | OVERSAMPLE 50% | IPAT OFF |
Parameters of Pre and post contrast T1 scans should be exactly same except from the Sequence preparation time(preparation time should be nil in the post-contrast scans )
T1 flash 3D coronal .9mm -1.1mm post-contrast upper leg
Plan the coronal slices on the sagittal Phase contrast vessel localiser; angle the position block parallel to the femoral artery. Check the positioning block in the other two planes. An appropriate angle must be given in the axial plane (parallel to the right and left femur). Slices must be sufficient to cover the femoral arteries .FOV must be big enough to cover the vessels from iliac arteries down to popliteal arteries . Phase oversampling and slice oversample, must be used to avoid wrap around artefacts. It’s important to overlap the abdominal and femoral blocks by 1 to 2 centimetres to avoid any misregistration. It is highly advisable to use Parallel acquisition technique to reduce the scan time (scan time should be less than 15 seconds to get best results). Protocol should be setup with an auto move of the table after the upper leg 3D flash acquisition.

Parameters
TR 2-3 | TE 1-2 | FLIP 20 | NEX 1 | SLICE 1 MM | MATRIX 384×384 | FOV 450-470 | PHASE R>L | OVERSAMPLE 30% | IPAT OFF |
T1 flash 3D coronal 1mm -1.3mm post contrast lower leg
Plan the coronal slices on the sagittal localiser; angle the position block parallel to the tibia. Check the positioning block in the other two planes. An appropriate angle must be given in the axial plane (parallel to the right and left tibia). Slices must be sufficient to cover the whole lower leg .FOV must be big enough to cover the vessels from knee joint down to ankle joint . Phase oversampling and slice oversample, must be used to avoid wrap around artefacts. It’s important to overlap the upper leg and lower leg blocks by 1 to 2 centimetres to avoid any misregistration. It is highly advisable to use Parallel acquisition technique to reduce the scan time (scan time should be less than 15 seconds to get best results).

Parameters
TR 2-3 | TE 1-2 | FLIP 20 | NEX 1 | SLICE 1 MM | MATRIX 384×384 | FOV 450-470 | PHASE R>L | OVERSAMPLE 30% | IPAT OFF |
CLICK THE SEQUENCES BELOW TO CHECK THE SCANS
- LOCALIZER_3PLANE_LOWERLEG1
- LOCALIZER_3PLANE_UPPERLEG2
- LOCALIZER__PC2D_SAGITAL_UPPERLEG3
- LOCALIZER_3PLANE_ABDOMEN4
- LOCALIZER_PC2D_SAGITAL_ABDOMEN5
- T1_FLASH_3D_CORONAL_ABDOMEN_PRE6
- T1_FLASH_3D_CORONAL_UPPERLEG_PRE7
- T1_FLASH_3D_CORONAL_LOWERLEG_PRE8
- CARE BOLUS
- T1_FLASH_3D_CORONAL_UPPERLEG_POST9
- T1_FLASH_3D_CORONAL_LOWERLEG_POST10
- T1_FLASH 3D_CORONAL_LOWER LEG_POST11


