MRI Warthin's Tumor (Papillary Cystadenoma Lymphomatosum)
Warthin’s tumor, also known as Warthin’s adenoma or papillary cystadenoma lymphomatosum, is a benign glandular salivary gland tumor. It is the second most common benign parotid gland tumor after pleomorphic adenoma. Warthin’s tumor primarily affects the parotid glands, which are located just in front of the ears. It was first described by pathologist Aldred Scott Warthin, and while its exact cause is not known, there are several factors and characteristics associated with it.
Symptoms:
Warthin’s tumor typically presents as a painless, slow-growing mass in the area of the parotid gland. Other symptoms may include:
- A lump in front of or below the ear
- Occasional pain or discomfort in the area of the tumor
- Repeated infections or inflammation in the salivary gland
- Difficulty swallowing or opening the mouth if the tumor grows large enough to impinge on surrounding structures
Treatment:
Treatment for Warthin’s tumor typically involves surgical removal, especially if the tumor is causing symptoms or there is any concern about the possibility of cancer, though Warthin’s tumor is almost always benign. The surgical options include:
- Superficial Parotidectomy: Removal of the superficial lobe of the parotid gland.
- Total Parotidectomy: Removal of the entire parotid gland if the tumor is extensive. This is less common.
- Enucleation: Removal of just the tumor, preserving as much of the salivary gland as possible.
MRI Appearance of Warthin's tumors
T1-Weighted Imaging (T1WI): Warthin’s tumor typically appears as a well-defined mass on T1-weighted images. The signal intensity is often low to intermediate compared to the surrounding muscle. Some parts of the tumor may show high signal intensity if there are areas of hemorrhage or high protein content within cystic spaces.
T2-Weighted Imaging (T2WI): On T2-weighted images, Warthin’s tumors usually have a high signal intensity, reflecting the cystic and fluid components of the lesion. The characteristic feature on T2WI is a very bright, almost homogeneous signal, although sometimes a slightly heterogeneous appearance can be seen due to varying protein concentrations or debris within the cystic components.
Short Tau Inversion Recovery (STIR): The STIR sequence is useful for suppressing fat signal, which can be abundant in the parotid gland region. Warthin’s tumors typically appear hyperintense on STIR images. This sequence can help to differentiate the tumor from surrounding lymph nodes and fatty tissues, which will be suppressed and appear dark.
Diffusion-Weighted Imaging (DWI): DWI assesses the movement of water molecules within tissue. Warthin’s tumor usually shows diffusion restriction due to its high cellularity, resulting in high signal intensity on DWI and low apparent diffusion coefficient (ADC) values. However, the cystic components of the tumor might show variable signal intensity based on their content.
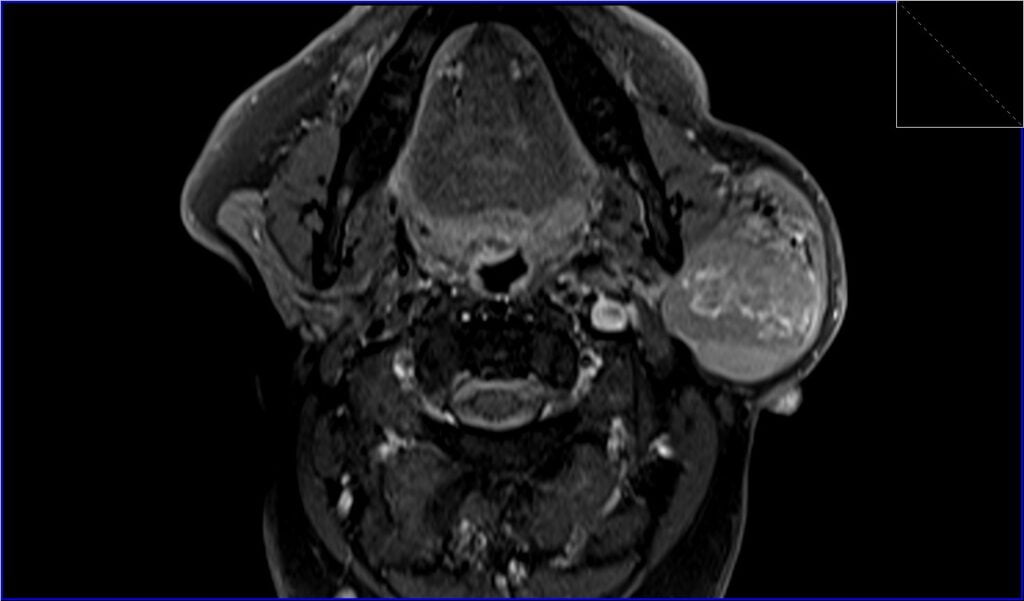
Post-Contrast T1 Appearance: After the administration of gadolinium-based contrast agents, Warthin’s tumors show strong enhancement, especially in the solid components, due to their rich blood supply. The enhancement can be heterogeneous because of the different components within the tumor. The cystic areas might show rim enhancement, while the solid nodular components can demonstrate more pronounced contrast uptake.
STIR coronal image shows Warthin's tumor

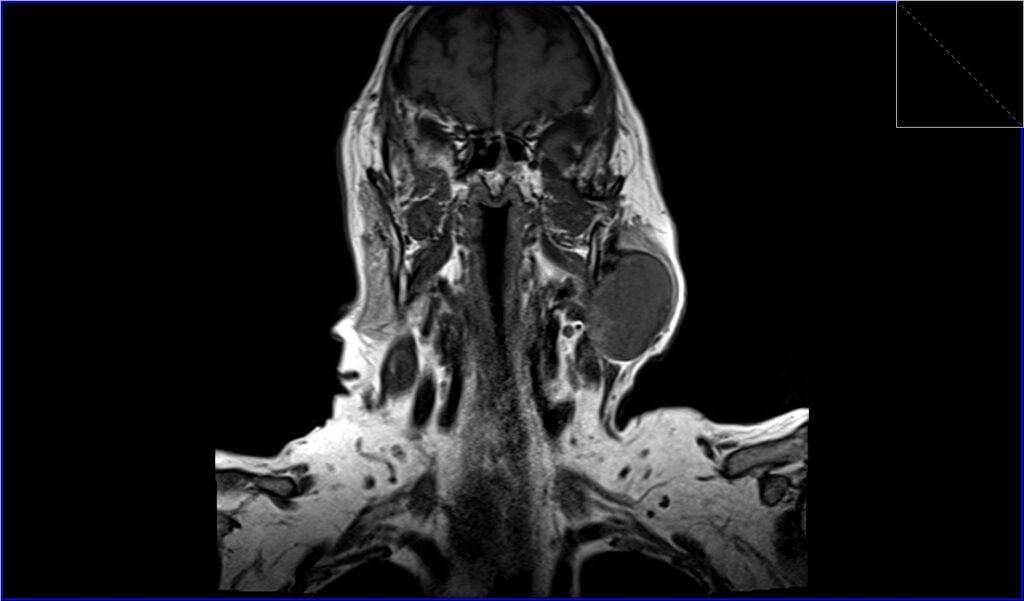
T1 coronal image shows Warthin's tumor
STIR axial image shows Warthin's tumor

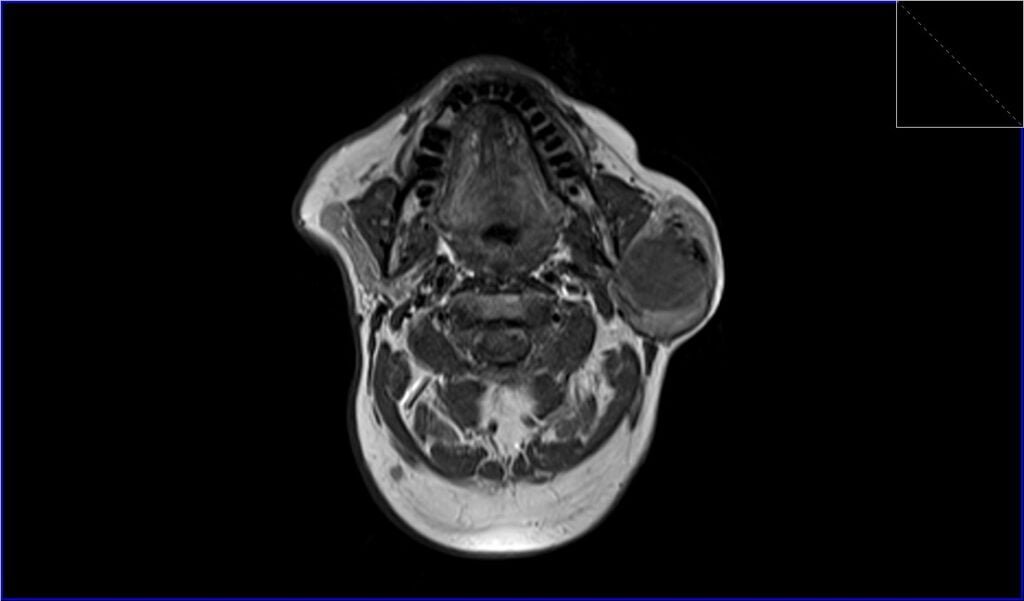
T1 axial image shows Warthin's tumor
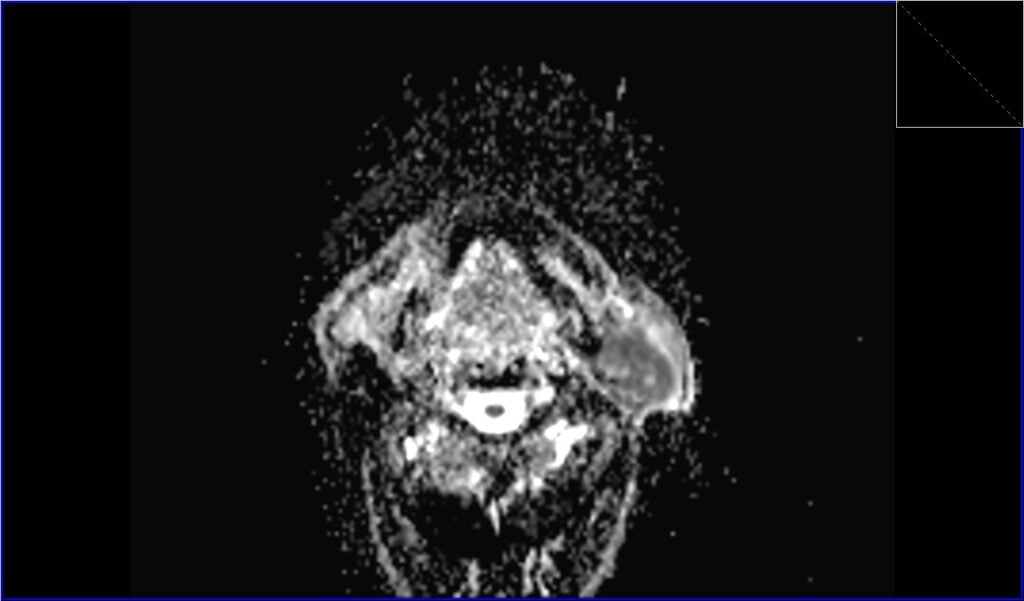
DWI axial b0 image shows Warthin's tumor

DWI axial b800 image shows Warthin's tumor

ADC axial image shows Warthin's tumor
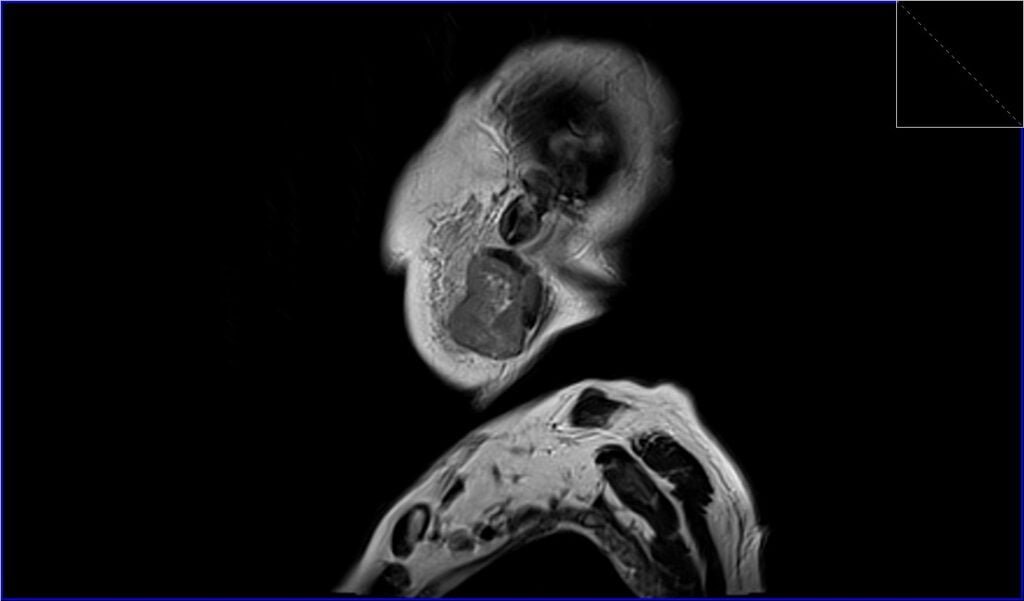
T2 sagittal image shows Warthin's tumor
T1 fat sat post contrast axial image shows Warthin's tumor
References
- Ikeda, M., Motoori, K., Hanazawa, T., Nagai, Y., Yamamoto, S., Ueda, T., Funatsu, H., & Ito, H. (2004). Warthin Tumor of the Parotid Gland: Diagnostic Value of MR Imaging with Histopathologic Correlation. AJNR Am J Neuroradiol, 25(7), 1256–1262. PMID: 15313720. PMCID: PMC7976549.
- Karaman CZ, Tanyeri A, Özgür R, Öztürk VS. Parotid gland tumors: comparison of conventional and diffusion-weighted MRI findings with histopathological results. Dentomaxillofac Radiol. 2021 May 1;50(4):20200391. doi: 10.1259/dmfr.20200391. PMID: 33237812; PMCID: PMC8077997.
- Kim, S. Y., Borner, U., Lee, J.-H., Wagner, F., & Vogel, D. W. T. (2022). Magnetic resonance imaging of parotid gland tumors: a pictorial essay. BMC Medical Imaging, 22, 191.
- Jia, C.-H., Wang, S.-Y., Li, Q., Qiu, J.-M., & Kuai, X.-P. (2021). Conventional, diffusion, and dynamic contrast-enhanced MRI findings for differentiating metaplastic Warthin’s tumor of the parotid gland. Science Progress, 104(2), 1–18. DOI: 10.1177/00368504211018583.
- Yao, H., Lin, H., Zhang, P., Zhang, T., & Feng, L. (2011). CT and MRI findings of parotid Warthin’s tumors. The Chinese-German Journal of Clinical Oncology, 10, 596–601. doi:10.1007/s10330-011-0866-5
