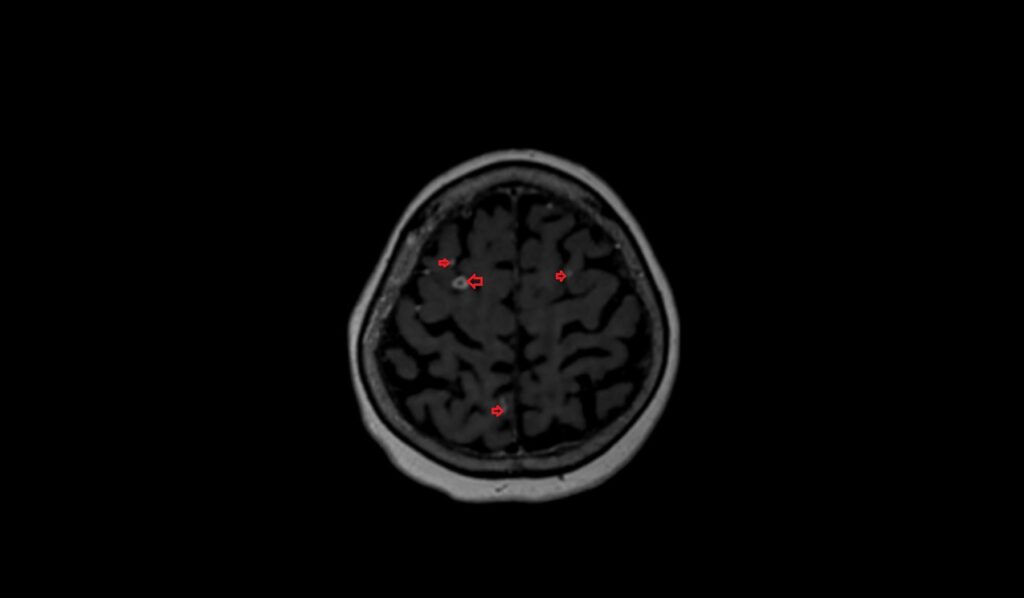
Tuberculoma MRI (Brain Tuberculoma)
Tuberculoma is a localized mass-like lesion or tumor-like granuloma that results from an infection caused by the bacterium Mycobacterium tuberculosis, which is the same organism that causes tuberculosis. Tuberculomas most commonly occur in the lungs, but they can also appear in the brain, liver, or other organs. These lesions are composed of immune cells that cluster together to form a granuloma around the tuberculosis bacteria as a way to isolate the infection.
Causes
Tuberculoma develops as a result of an immune response to tuberculosis infection. The formation of a tuberculoma is part of the body’s attempt to wall off and contain the bacteria. This can occur during an active TB infection or can be a part of a secondary or reactivated form of tuberculosis, especially in individuals with weakened immune systems.
Symptoms
Symptoms of tuberculoma depend on the location and size of the mass. Common symptoms include:
Neurological Tuberculoma (Brain):
- Headaches
- Seizures
- Focal neurological deficits (e.g., weakness in one part of the body)
- Changes in mental status or behavior
- Nausea and vomiting due to increased intracranial pressure
Pulmonary Tuberculoma (Lungs):
- Persistent cough
- Chest pain
- Hemoptysis (coughing up blood)
- Shortness of breath
- Fever and night sweats
Diagnosis
Diagnosing a tuberculoma involves a combination of imaging studies and microbiological tests:
- Imaging: Radiological techniques such as X-rays, computed tomography (CT) scans, and magnetic resonance imaging (MRI) are crucial. For brain tuberculomas, MRI is particularly useful as it provides detailed images of the brain.
- Laboratory Tests: Tests might include sputum smear microscopy, culture for Mycobacterium tuberculosis, and molecular tests like PCR to detect TB DNA.
- Biopsy: In some cases, a sample of tissue may be taken from the granuloma to be analyzed for the presence of tuberculosis bacteria.
Treatment
The treatment of tuberculoma involves a combination of anti-tuberculosis medications and, in some cases, surgical intervention:
Medications:
- First-Line Anti-TB Drugs: The standard treatment includes a regimen of isoniazid, rifampicin, pyrazinamide, and ethambutol. These drugs are taken for a minimum of 6-12 months.
- Adjunctive Corticosteroids: In cases of neurological tuberculoma, corticosteroids may be prescribed to reduce inflammation and cerebral edema.
Surgical Intervention:
- Surgery may be considered if the tuberculoma is causing significant pressure effects, is resistant to medical therapy, or if there is a need to obtain a biopsy for diagnosis.
MRI appearance of Brain Tuberculoma
Non-caseating Granuloma
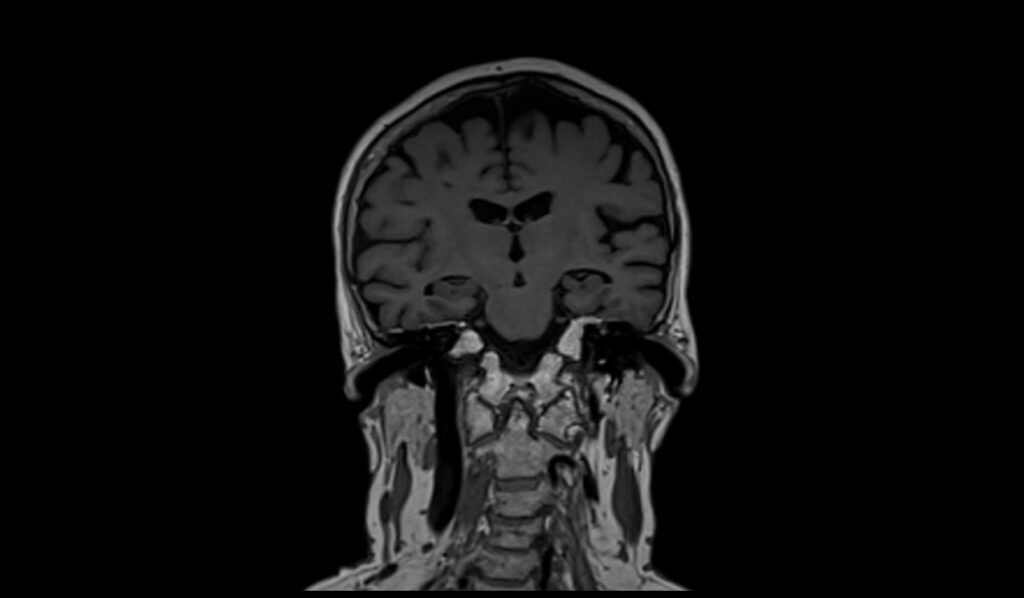
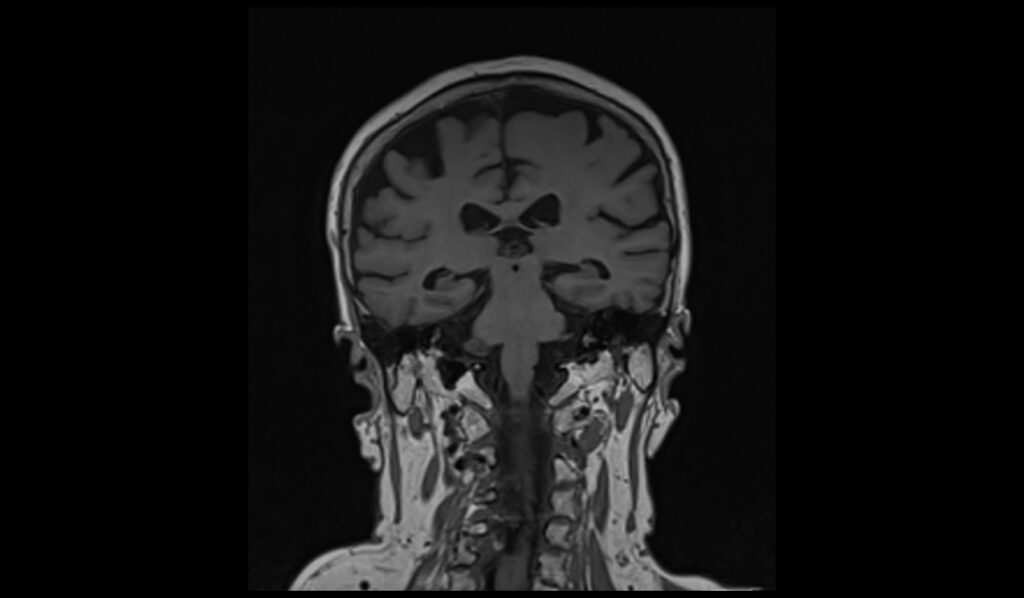
T1-weighted (T1):
- Isointense or hypointense compared to brain parenchyma.
- Poorly defined margins.
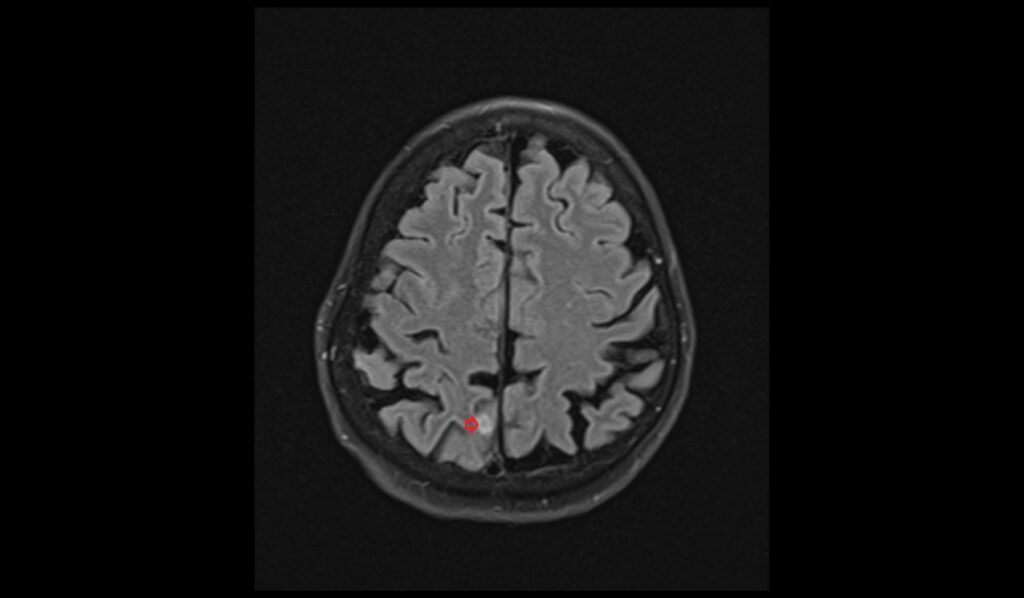
T2-weighted (T2):
- Hyperintense signal due to high water content.
- Surrounding edema may be present.
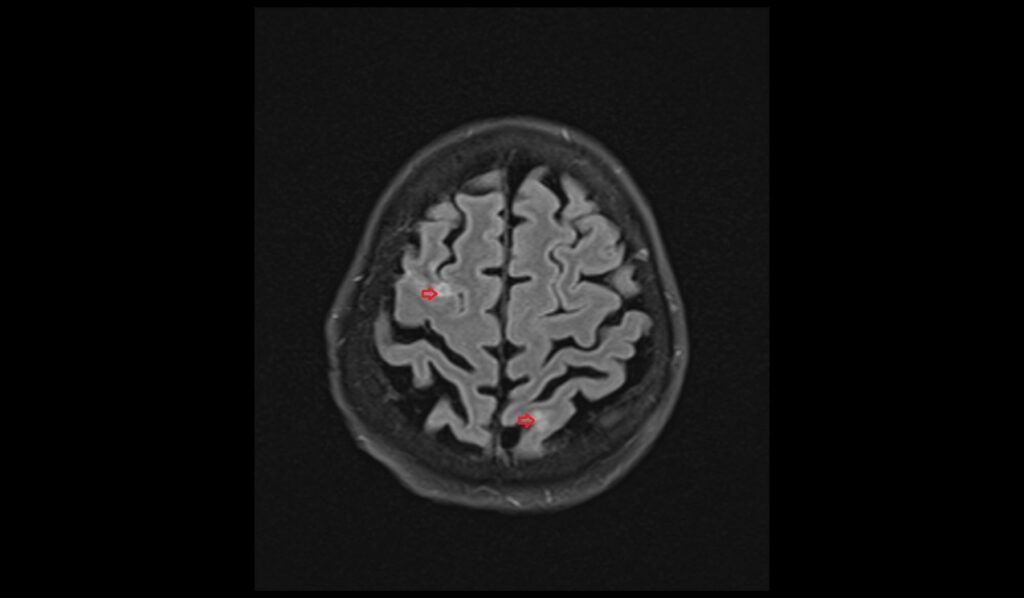
FLAIR (Fluid-attenuated inversion recovery):
- Hyperintense signal similar to T2.
- Helps in suppressing cerebrospinal fluid (CSF) for better lesion visibility.
DWI (Diffusion-weighted imaging):
- b0: Isointense or slightly hyperintense.
- b1000: Variable signal, usually hypointense to isointense.
- ADC (Apparent diffusion coefficient): Increased ADC values indicating restricted diffusion is less prominent.
T1 post-contrast:
- Homogeneous enhancement indicating non-caseating nature.
- Margins may become more defined after contrast administration.
Caseating Granuloma
T1-weighted (T1):
- Hypointense core with hyperintense rim.
- Central necrosis leads to core hypointensity.
T2-weighted (T2):
- Hyperintense rim with a hypointense core.
- Surrounding vasogenic edema is common.
FLAIR (Fluid-attenuated inversion recovery):
- Hyperintense rim with a hypointense core, aiding in differentiation from non-caseating types.
- Useful in identifying perilesional edema.
DWI (Diffusion-weighted imaging):
- b0: Hypointense or isointense core with a hyperintense rim.
- b1000: Hyperintense rim with a hypointense core.
- ADC (Apparent diffusion coefficient): Decreased ADC values in the core indicating restricted diffusion typical of caseating necrosis.
T1 post-contrast:
- Ring enhancement is characteristic due to the central necrotic area.
- Rim enhancement helps in distinguishing from other lesions.
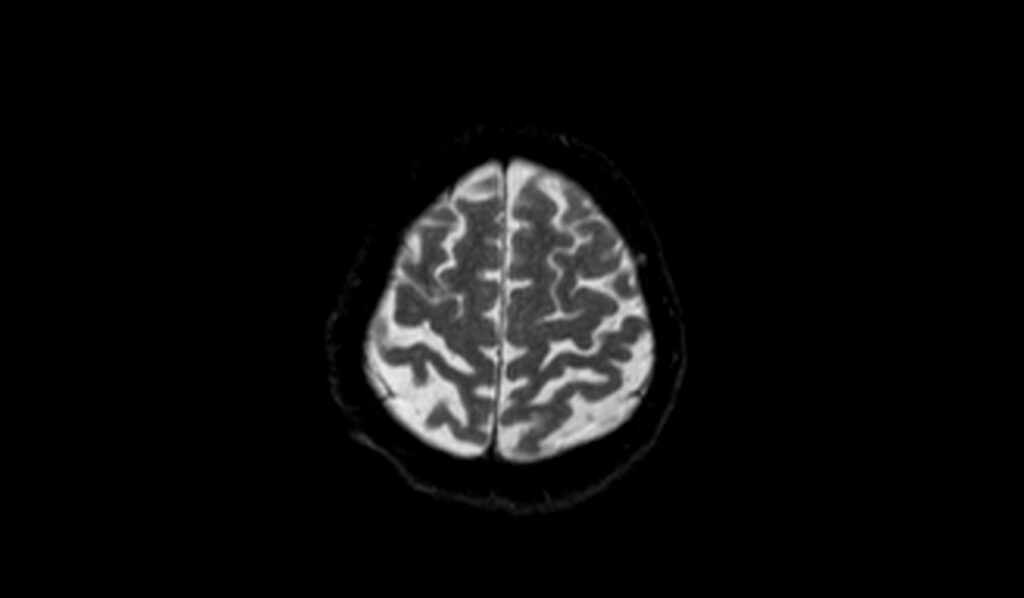
T2 axial images shows Brain Tuberculoma



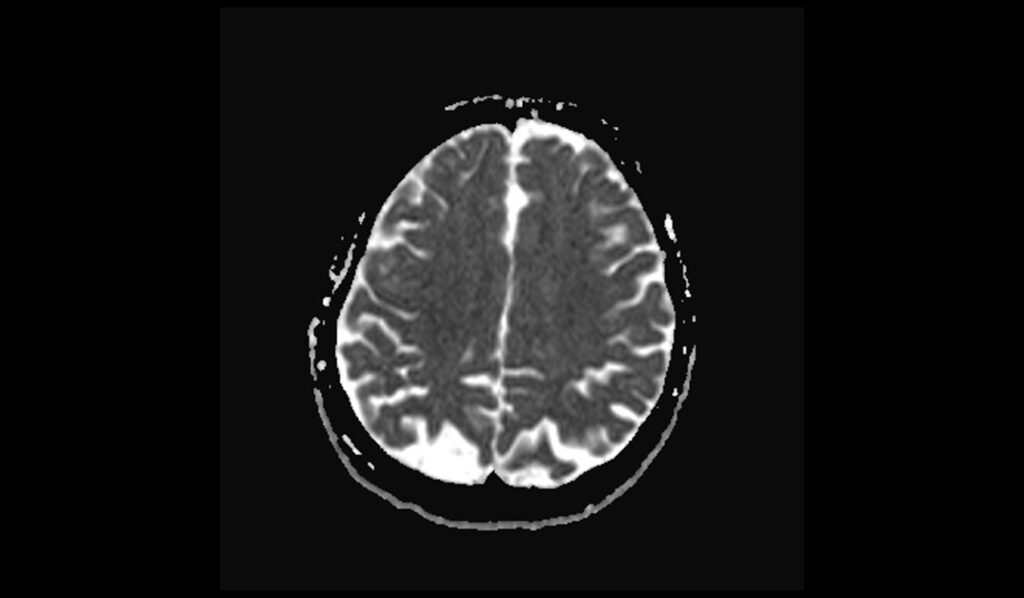
FLAIR axial images shows Brain Tuberculoma

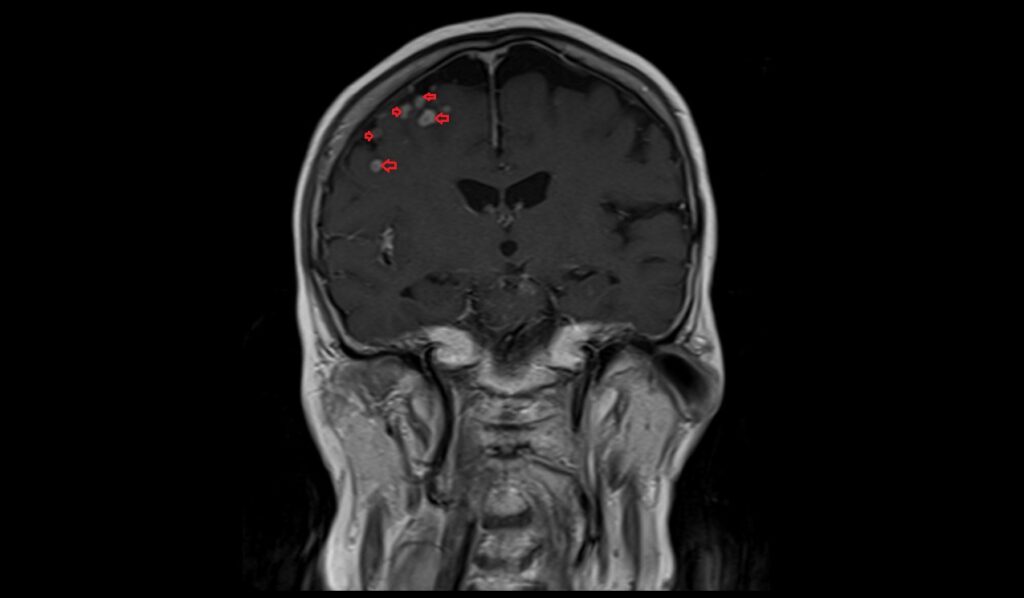
T1 coronal images shows Brain Tuberculoma
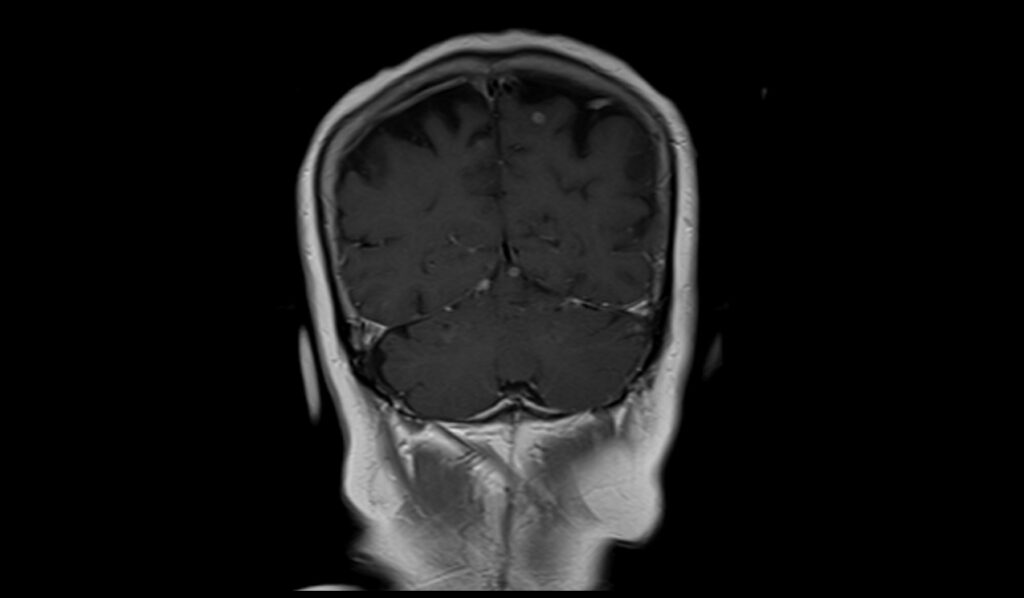
T2 sagittal image shows Brain Tuberculoma

DWI b0 image shows Brain Tuberculoma

DWI b1000 image shows Brain Tuberculoma


DWI ADC map image shows Brain Tuberculoma

T1 coronal post contrast images shows Brain Tuberculoma
T1 axial post contrast image shows Brain Tuberculoma
T1 sagittal post contrast image shows Brain Tuberculoma

References
- Parry, A.H., Wani, A.H., Shaheen, F.A., Wani, A.A., Feroz, I. and Ilyas, M., 2018. Evaluation of intracranial tuberculomas using diffusion-weighted imaging (DWI), magnetic resonance spectroscopy (MRS) and susceptibility weighted imaging (SWI). British Journal of Radiology, 91(1091), p.20180342.
- Ma, H., Liu, Y., Zhuang, C., Shen, Y. and Wu, R., 2018. Clinical features and MRI findings of intracranial tuberculomas. Radiology of Infectious Diseases, 5(4), pp.154-159.
- Ibrahim, I.G., Osman, A.A., Shikhow, M.G., Celik, C., Mutlu, E., Qalaf, M.S.H., Tahtabaşı, M. and mohameda, Y.G., 2022. Magnetic resonance imaging findings of intracranial tuberculoma patients in a tertiary hospital in Mogadishu, Somalia: A retrospective study. Annals of Medicine and Surgery (Lond), 78, p.103812.
- Koesbandono, R., Muljadi, R., Sutanto, R., Fransiska, S.R., Takaliuang, D. and Erico, A., 2024. Intracranial tuberculomas: review of MRI findings and clinical features. Clinical Radiology, 79(5), pp.354-362.
- Perez-Malagon, C.D., Barrera-Rodriguez, R., Lopez-Gonzalez, M.A. and Alva-Lopez, L.F., 2021. Diagnostic and neurological overview of brain tuberculomas: A review of literature. Cureus, 13(12), p.e20133.


