Syringomyelia MRI
Syringomyelia is a neurological condition where a cyst or cavity, called a syrinx, forms within the spinal cord. This cyst can expand and elongate over time, damaging the spinal cord and resulting in a range of symptoms.
Causes
The exact cause of syringomyelia is not always clear, but it often develops as a complication of:
- Chiari Malformation: A condition where brain tissue extends into the spinal canal. This is one of the most common associations with syringomyelia.
- Spinal Cord Injury: Trauma can lead to cyst formation.
- Meningitis: Inflammation of the membranes around the brain and spinal cord can result in a syrinx.
- Tumors: Spinal cord tumors can obstruct normal fluid flow, leading to syrinx formation.
Symptoms
Syringomyelia symptoms vary depending on the size and location of the syrinx. Common symptoms include:
- Pain: Often starts in the neck and back.
- Muscle Weakness and Wasting: Due to nerve damage in the spinal cord.
- Stiffness: In the back, shoulders, arms, or legs.
- Loss of Reflexes: Particularly in the extremities.
- Sensory Loss: Reduced ability to feel hot and cold, especially in the hands.
- Motor Difficulties: Coordination and balance issues.
- Bowel and Bladder Dysfunction: In more advanced cases.
MRI Appearance of Syringomyelia
T1-Weighted Images (T1WI):
- On T1-weighted MRI, a syrinx usually appears as a low signal intensity area (meaning it looks darker) within the spinal cord. This is because the fluid in the syrinx has a similar signal intensity to cerebrospinal fluid (CSF). The surrounding spinal cord tissue may appear normal or show signs of atrophy.
T2-Weighted Images (T2WI):
- Syringomyelia is more conspicuous on T2-weighted images. Here, the syrinx exhibits high signal intensity (brighter appearance), contrasting with the relatively lower signal of the surrounding spinal cord tissue. This contrast helps in clearly delineating the extent and location of the syrinx.
Short Tau Inversion Recovery (STIR):
- In the STIR sequence, the syrinx will also appear as high signal intensity, similar to T2-weighted images. STIR is particularly useful in suppressing fat signals and highlighting edema or inflammation, if present.
Post-Contrast T1 with Fat Saturation (T1 Fat Sat):
- After the administration of contrast material (gadolinium), there is usually no enhancement of a simple syrinx, as it lacks a blood supply. However, post-contrast images can be valuable in identifying associated conditions or complications, such as tumors or areas of inflammation. The fat saturation technique helps in suppressing signals from fatty tissues, making any contrast enhancement more conspicuous.
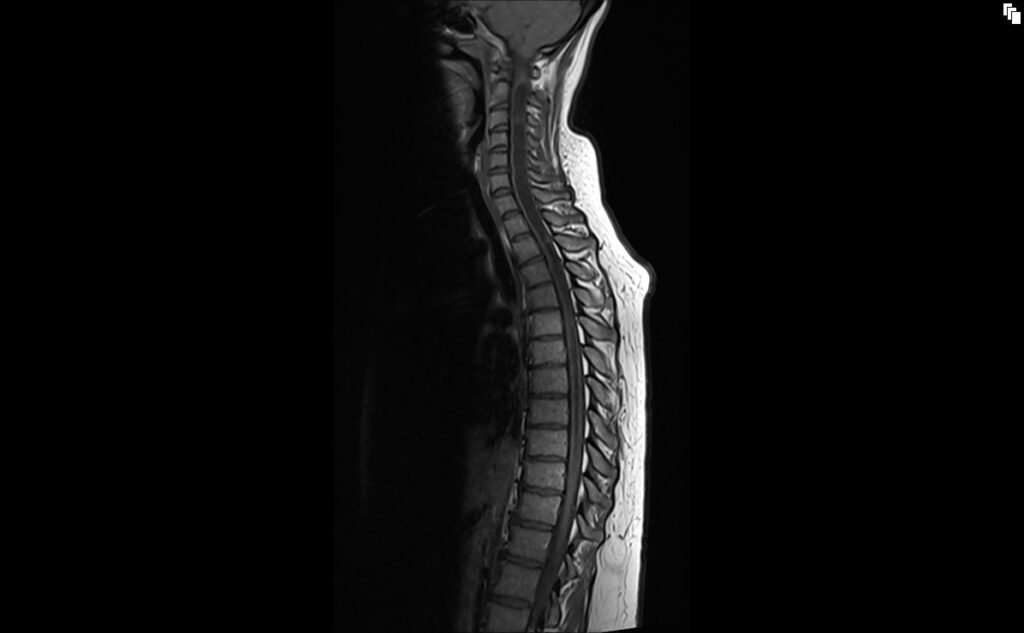
T2 sagittal image shows Syringomyelia

STIR sagittal image shows Syringomyelia

T1 TSE sagittal image shows Syringomyelia
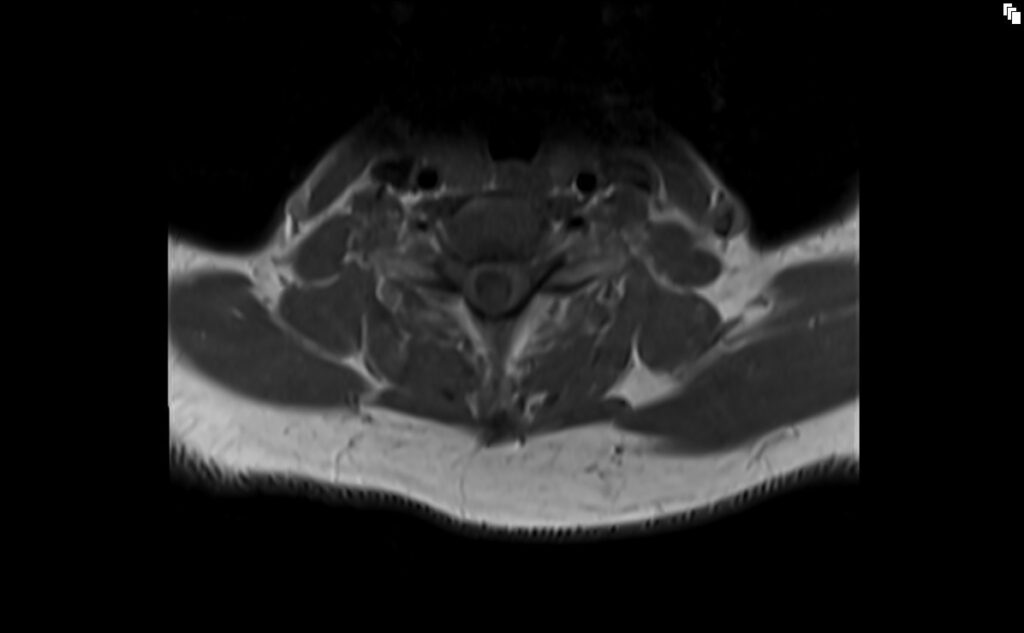
T2 TSE axial image shows Syringomyelia

T2 TSE axial image shows Syringomyelia
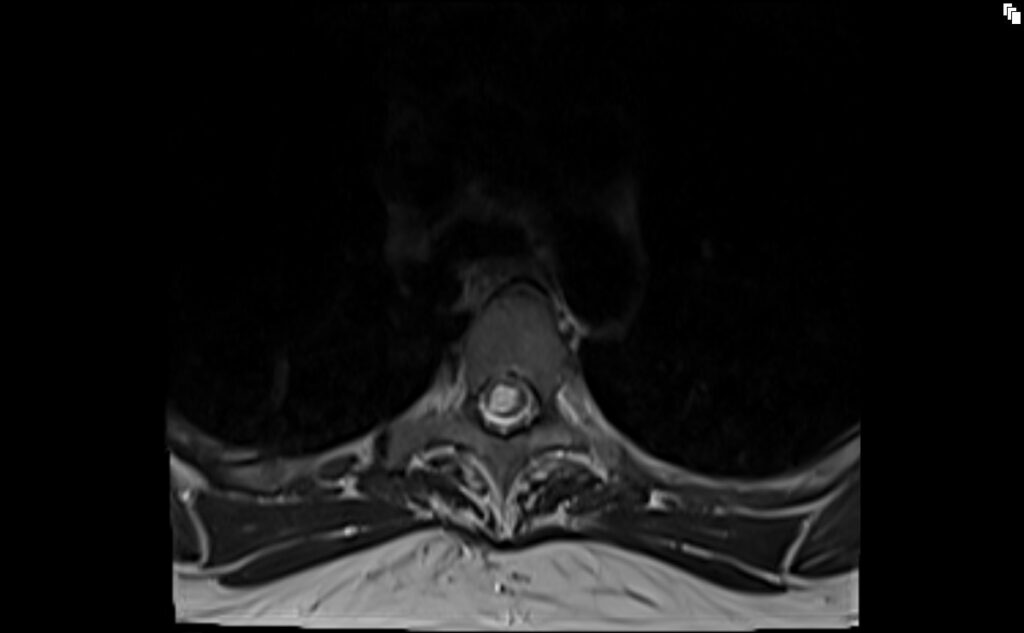
T1 TSE axial image shows Syringomyelia
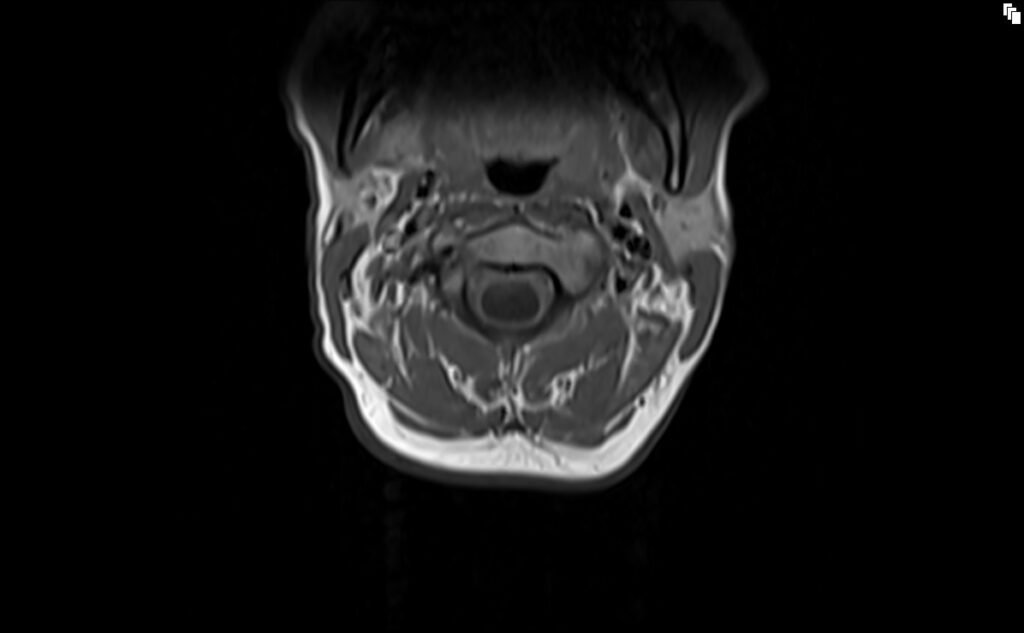
T1 TSE axial image shows Syringomyelia
References
- Timpone, V. M., & Patel, S. H. (2015). MRI of a Syrinx: Is Contrast Material Always Necessary? American Journal of Roentgenology, 204(5), https://doi.org/10.2214/AJR.14.13310.
- Fujii, K., Natori, Y., Nakagaki, H., & Fukui, M. (1991). Management of syringomyelia associated with Chiari malformation: Comparative study of syrinx size and symptoms by magnetic resonance imaging. Surgical Neurology, 36(4), 281-285.
- Kleindienst, A., Engelhorn, T., Roeckelein, V., & Buchfelder, M. (2020). Development of pre-syrinx state and syringomyelia following a minor injury: a case report. Journal of Medical Case Reports, 14, 223. doi:10.1186/s13256-020-02583-4
- Heiss JD, Snyder K, Peterson MM, Patronas NJ, Butman JA, Smith RK, DeVroom HL, Sansur CA, Eskioglu E, Kammerer WA, Oldfield EH. Pathophysiology of primary spinal syringomyelia. J Neurosurg Spine. 2012 Nov;17(5):367-380. Published online 2012 Sep 7.


