Sturge-Weber Syndrome MRI
Sturge-Weber Syndrome (SWS), also known as encephalotrigeminal angiomatosis, is a rare congenital neurological and skin disorder. It is characterized by abnormal blood vessels on the brain surface and skin, leading to a variety of symptoms.
Classification
SWS is classified based on the areas of the body affected:
Type I (Classic Sturge-Weber Syndrome): This type involves facial and leptomeningeal angiomas (abnormal blood vessel formations in the brain’s surface) and may include glaucoma.
Type II: This type involves a facial angioma without evidence of leptomeningeal involvement or neurological symptoms, but may include glaucoma.
Type III: This type involves only leptomeningeal angiomas with no facial involvement, but neurological symptoms are present.
Cause
Sturge-Weber syndrome is caused by a somatic mutation in the GNAQ gene. This mutation occurs after conception and is not inherited from the parents; instead, it arises spontaneously in one of the developing cells. The mutation affects the development of certain blood vessels, leading to the abnormalities seen in the syndrome.
Symptoms
Symptoms of Sturge-Weber syndrome can vary significantly but typically include:
- Port-wine stain: A reddish-purple birthmark typically appearing on one side of the face, often over the forehead and eyelid.
- Neurological symptoms: These can include seizures, which may begin in infancy and vary in severity. Additional issues may involve weakness on one side of the body, developmental delays, and migraines.
- Eye problems: Glaucoma is common, occurring in about 30% of those with a facial port-wine stain. It can lead to increased pressure in the eye that can cause damage to the optic nerve.
Diagnosis
Diagnosis of Sturge-Weber syndrome typically involves:
- Medical history and physical examination: Including detailed assessment of the skin and neurological symptoms.
- Imaging studies: MRI (magnetic resonance imaging) of the brain to detect leptomeningeal angiomas and look for evidence of brain involvement.
- Eye examination: To check for signs of glaucoma and other ocular issues.
Treatment
Treatment of Sturge-Weber syndrome is symptomatic and tailored to the individual needs of the patient:
- Management of seizures: Anticonvulsant medications are prescribed to control seizures.
- Treatment for glaucoma: Medications, laser treatments, or surgery may be required to manage glaucoma.
- Laser treatment for port-wine stain: Pulsed dye laser can be used to lighten the skin marking, although multiple treatments are often necessary.
- Physical therapy and educational support: These are recommended to address developmental delays and neurological issues.
- Regular monitoring: Continuous assessment by a team of specialists, including neurologists, dermatologists, and ophthalmologists, is crucial.
MRI appearance of Sturge-Weber syndrome
MRI T1 Appearance of Sturge-Weber Syndrome
In Sturge-Weber Syndrome, T1-weighted MRI images typically show cortical and subcortical atrophy in the affected hemisphere. Gyral calcifications, a hallmark of the syndrome, often appear hyperintense on T1-weighted images due to the presence of calcium. Additionally, prominent meningeal enhancement may be visible post-contrast, indicating abnormal blood vessels and leptomeningeal angiomas. These features contribute to the characteristic appearance of the syndrome on T1-weighted imaging.
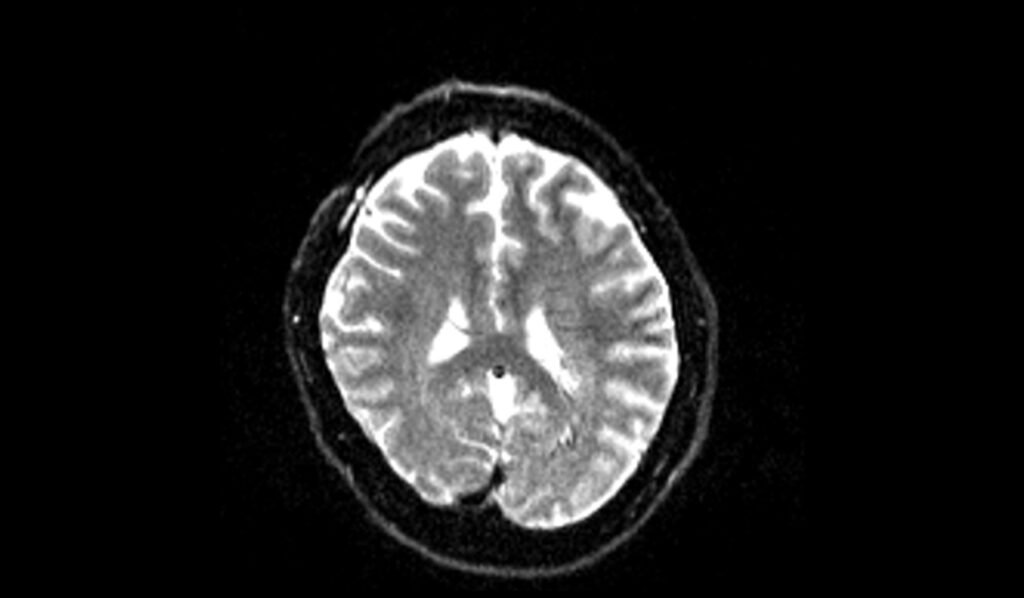
MRI T2 Appearance of Sturge-Weber Syndrome
T2-weighted MRI images of patients with Sturge-Weber Syndrome often reveal cortical and subcortical hyperintensities due to gliosis and venous congestion. The cortical calcifications, which appear hyperintense on T1, typically show as hypointense on T2-weighted images. These calcifications, coupled with the hyperintense signals from gliosis, help delineate the affected regions. Dilated medullary and leptomeningeal vessels can also appear as high-signal intensity areas, reflecting the vascular malformations characteristic of the syndrome.
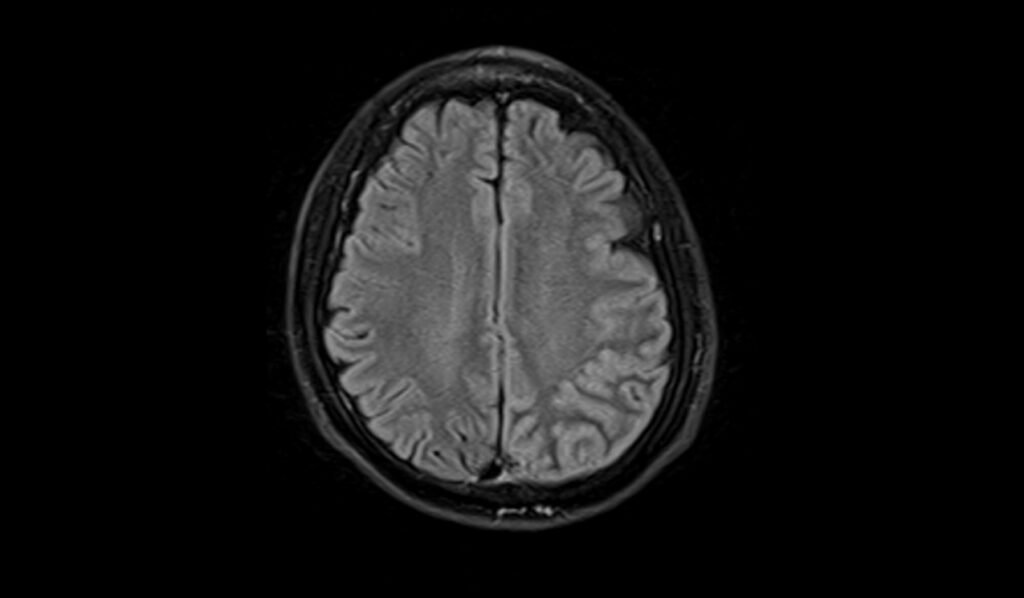
MRI FLAIR Appearance of Sturge-Weber Syndrome
FLAIR (Fluid-Attenuated Inversion Recovery) MRI sequences in Sturge-Weber Syndrome highlight the areas of cortical and subcortical hyperintensity, which correspond to gliosis and chronic ischemic changes. The leptomeningeal enhancement, indicative of abnormal vasculature, may also appear hyperintense on FLAIR images. FLAIR is particularly useful in identifying these lesions because it suppresses the cerebrospinal fluid (CSF) signal, making the abnormal parenchymal and meningeal signals more conspicuous.
MRI DWI b0, b1000 and ADC Appearance of Sturge-Weber Syndrome
Diffusion-weighted imaging (DWI) in Sturge-Weber Syndrome can show mixed signal intensity in the affected areas, especially if hemorrhage is present. At b0, diffusion images may appear normal or show mild hyperintensity due to gliosis and ischemia. At b1000, restricted diffusion may be visible in acute ischemic areas, appearing hyperintense. The apparent diffusion coefficient (ADC) maps typically show corresponding hypointensities in these areas. In the presence of hemorrhage, DWI might show heterogeneous signals due to the complex interplay of restricted and facilitated diffusion in the hemorrhagic and surrounding gliotic tissue.
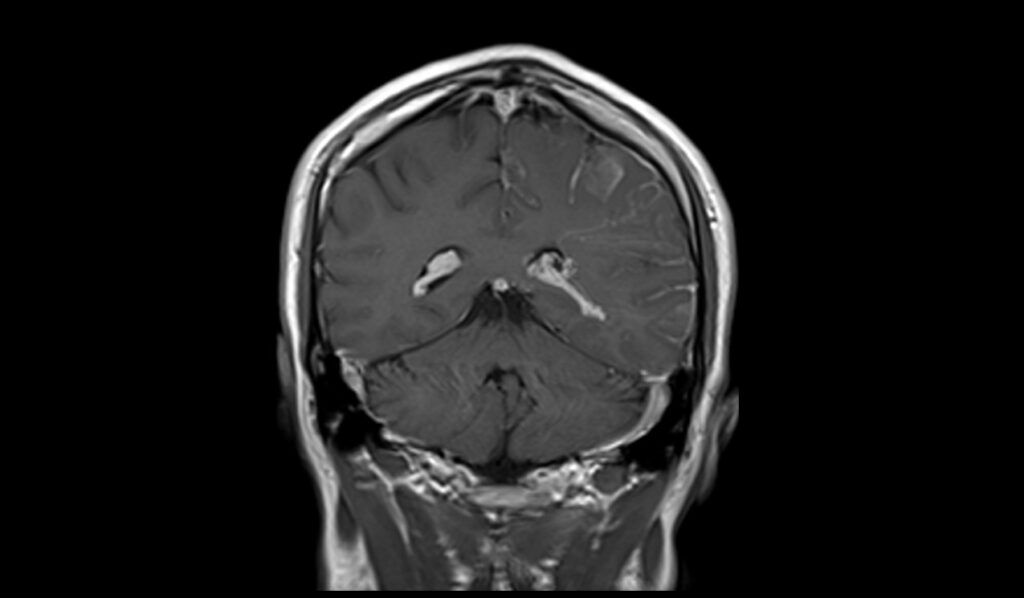
MRI T1 Post-Contrast Appearance of Sturge-Weber Syndrome
Post-contrast T1-weighted MRI images in Sturge-Weber Syndrome reveal prominent leptomeningeal enhancement, indicating the presence of abnormal blood vessels and angiomas. These enhancements are most pronounced in the regions of cortical atrophy and gyral calcifications. The abnormal vascular network enhances distinctly due to the contrast agent, providing a clear demarcation of the affected areas. This enhancement pattern is a key diagnostic feature, helping to differentiate Sturge-Weber Syndrome from other neurocutaneous disorders.
T2 axial image shows Sturge-Weber syndrome


FLAIR axial image shows Sturge-Weber syndrome

T1 axial images shows Sturge-Weber syndrome


T2 sagittal images shows Sturge-Weber syndrome

DWI b0 images shows Sturge-Weber syndrome
DWI b1000 images shows Sturge-Weber syndrome

DWI ADC images shows Sturge-Weber syndrome

T1 post contrast axial images shows Sturge-Weber syndrome




T1 post contrast coronal images shows Sturge-Weber syndrome


References
- Ragupathi, S., Reddy, A. K., Jayamohan, A. E., & Lakshmanan, P. M. (2014). Sturge-Weber syndrome: CT and MRI illustrations. BMJ Case Reports.
- Elster, A. D., & Chen, M. Y. M. (1990). MR Imaging of Sturge-Weber Syndrome: Role of Gadopentetate Dimeglumine and Gradient-Echo Techniques. American Journal of Neuroradiology, 11(4), 685-689.
- Pinto, A. L., Chen, L., Friedman, R., Grant, P. E., Poduri, A., Takeoka, M., Prabhu, S. P., & Sahin, M. (2016). Sturge-Weber Syndrome: Brain Magnetic Resonance Imaging and Neuropathology Findings. Pediatric Neurology, 58, 25-30. Elsevier.
