MRI Spinal schwannomas
Spinal schwannoma, also known as a spinal neurilemmoma, is a type of tumor that arises from the Schwann cells, which are cells that produce the myelin sheath surrounding nerves. This sheath is crucial for proper nerve function, as it helps to insulate the nerve and facilitate the transmission of electrical signals. Schwannomas are usually benign (non-cancerous) and slow-growing tumors.
Causes
The exact cause of spinal schwannomas is not fully understood. They can occur sporadically, without a clear reason, or they may be associated with genetic disorders such as neurofibromatosis type 2 (NF2). In NF2, there is a mutation in the gene that controls the production of a protein called merlin, which normally suppresses tumor growth.
Symptoms
The symptoms of a spinal schwannoma vary depending on the size and location of the tumor and may include:
- Pain: Often the first symptom. It can be localized back pain or radiating pain, depending on the nerve affected.
- Muscle Weakness or Numbness: Compression of the spinal cord or nerve roots can lead to sensory or motor deficits.
- Difficulty with Coordination: Compression of the spinal cord can affect coordination, particularly in the legs.
- Bowel or Bladder Dysfunction: Severe spinal cord compression may affect control of bladder or bowel functions.
Many spinal schwannomas, however, are asymptomatic and are found incidentally during imaging for other reasons.
Diagnosis
Diagnosing a spinal schwannoma typically involves a combination of:
- Medical History and Physical Examination: To assess symptoms and possible neurological deficits.
- Imaging Studies: Magnetic resonance imaging (MRI) is the primary tool for visualizing the spinal cord and identifying tumors. A computed tomography (CT) scan may also be used.
- Biopsy: In some cases, a biopsy may be performed to confirm the diagnosis, although this may not always be necessary if imaging is conclusive.
Treatment
Treatment for spinal schwannomas depends on the size, location, symptoms, and the patient’s overall health:
- Observation: Small, asymptomatic tumors may just be monitored with regular MRI scans.
- Surgery: The main treatment for symptomatic schwannomas is surgical removal. The goal is to remove the tumor without damaging surrounding nerves. Techniques vary depending on the tumor’s location and size, and may include less invasive options.
- Radiation Therapy: Stereotactic radiosurgery, such as Gamma Knife or CyberKnife, may be an option for tumors that are difficult to remove surgically or for patients who cannot undergo surgery. Conventional radiation therapy may also be used, particularly if the tumor cannot be completely removed or if it recurs after surgery.
- Chemotherapy: Rarely used for benign schwannomas, but may be considered if the tumor is malignant or cannot be fully addressed with surgery or radiation.
MRI Appearance of Spinal schwannomas
T1-Weighted Images
- Pre-contrast: Spinal schwannomas typically appear isointense or slightly hypointense (darker) compared to the spinal cord on T1-weighted images.
- Post-contrast (with gadolinium): These tumors usually enhance homogeneously with intravenous contrast, but they can sometimes show heterogeneous enhancement if cystic or necrotic areas are present.
- T1 with fat saturation (fat sat): After contrast administration, fat saturation is used to suppress the signal from fat, making the enhanced tumor more conspicuous against the suppressed background.
T2-Weighted Images
- Schwannomas are usually hyperintense (brighter) on T2-weighted images, but they may have areas of hypointensity if there are dense collagenous parts or areas of calcification.
Short Tau Inversion Recovery (STIR) images
- On STIR images, which suppress the fat signal, schwannomas will typically be hyperintense, aiding in the detection of the lesion, particularly if it is small or in a complex area with lots of surrounding fat.
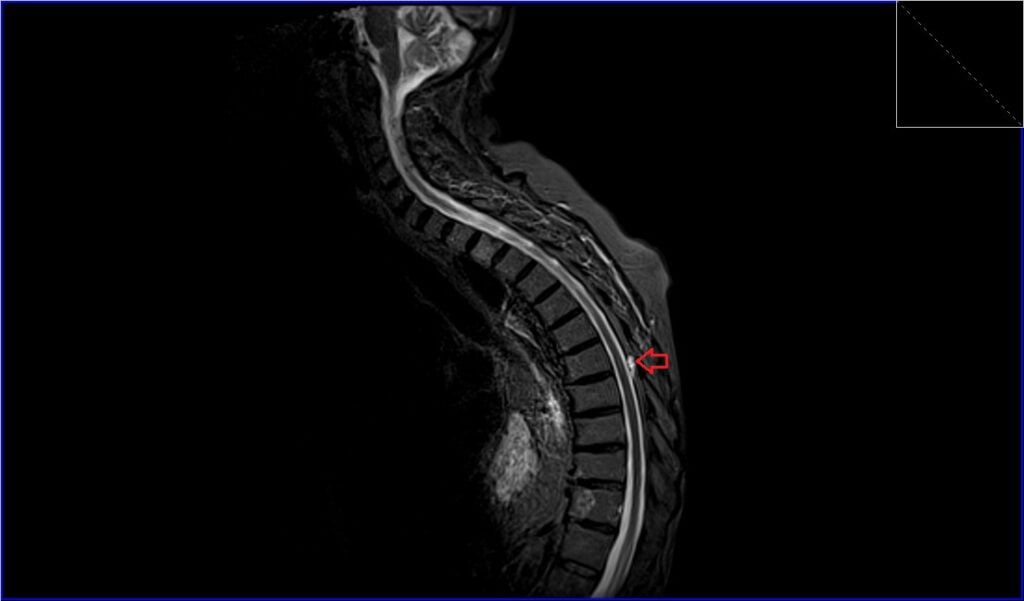
STIR sagittal image shows Spinal Schwannoma
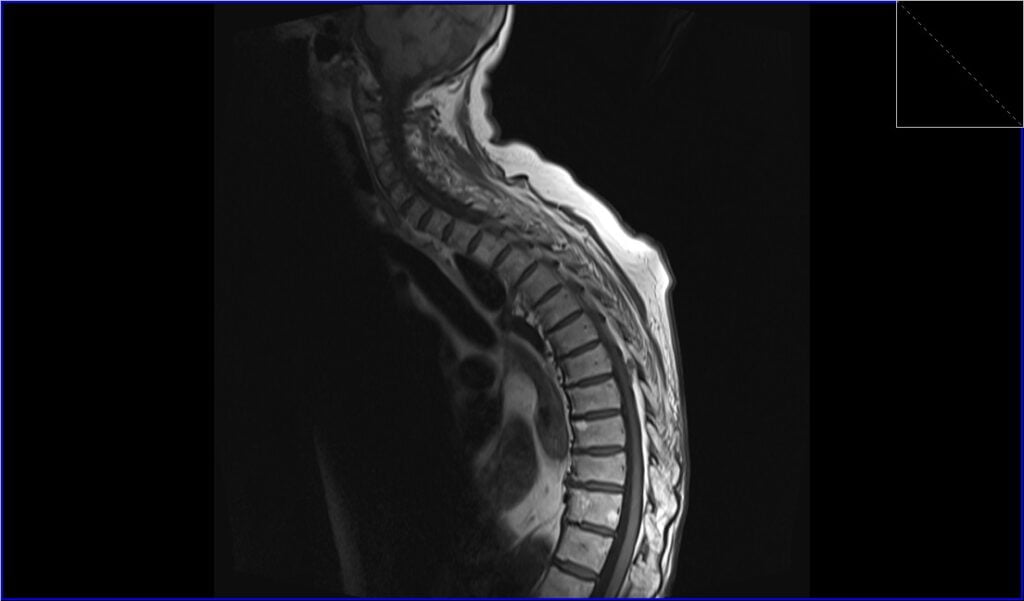
T1 TSE sagittal image shows Spinal Schwannoma
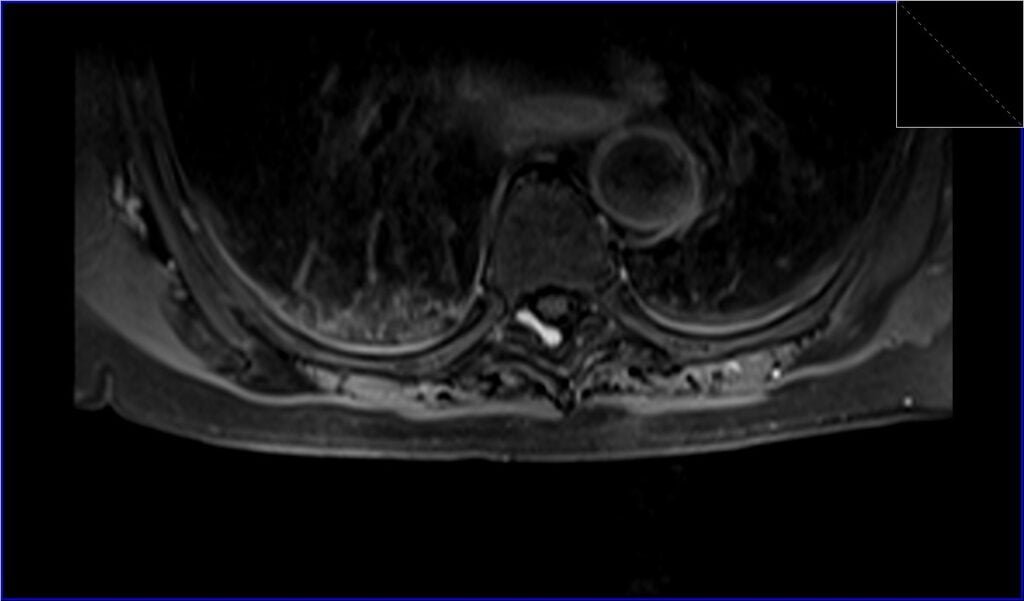
T2 TSE axial image shows Spinal Schwannoma

T1 TSE axial image shows Spinal Schwannoma

Post-contrast T1 sagittal image shows Spinal Schwannoma

Post-contrast T1 fat saturation axial image shows Spinal Schwannoma
References
- Friedman, D. P., Tartaglino, L. M., & Flanders, A. E. (1992). Intradural schwannomas of the spine: MR findings with emphasis on contrast-enhancement characteristics. AJR Am J Roentgenol, 158(6), 1347-1350. doi: 10.2214/ajr.158.6.1590138. PMID: 1590138.
- Kobayashi, K., Imagama, S., Ando, K., Hida, T., Ito, K., Tsushima, M., Ishikawa, Y., Matsumoto, A., Morozumi, M., Tanaka, S., & Ishiguro, N. (2017). Contrast MRI Findings for Spinal Schwannoma as Predictors of Tumor Proliferation and Motor Status. Spine (Phila Pa 1976), 42(3), E150-E155. doi: 10.1097/BRS.0000000000001732.
- Riffaud, L., Morandi, X., Massengo, S., Carsin-Nicol, B., Heresbach, N., & Guegan, Y. (2000). MRI of intramedullary spinal schwannomas: case report and review of the literature. Neuroradiology, 42(4), 275-279. doi: 10.1007/s002340050885. PMID: 10872172.
- Ito, S., Ando, K., Kobayashi, K., Nakashima, H., Oda, M., Machino, M., Kanbara, S., Inoue, T., Yamaguchi, H., Koshimizu, H., Mori, K., Ishiguro, N., & Imagama, S. (2021). Automated Detection of Spinal Schwannomas Utilizing Deep Learning Based on Object Detection From Magnetic Resonance Imaging. Spine (Phila Pa 1976), 46(2), 95-100. doi: 10.1097/BRS.0000000000003749.
- Lee JH, Kim HS, Yoon YC, Cha MJ, Lee SH, Kim ES. Differentiating between spinal schwannomas and meningiomas using MRI: A focus on cystic change. PLoS One. 2020;15(5):e0233623. Published online 2020 May 29. doi: 10.1371/journal.pone.0233623. PMID: 32469953. PMC ID: PMC7259580.


