MRI Spinal Seroma
A seroma is a collection of fluid that builds up under the surface of the skin, often appearing at a surgical site where tissue has been removed. In the context of the spine, a seroma can occur after spinal surgery, such as a laminectomy, discectomy, spinal fusion, or any procedure that involves significant tissue disruption. The fluid in a seroma is typically a serous fluid, which is a clear or pale yellow, protein-rich fluid that is a component of blood.
Symptoms of Seroma in the Spine:
Swelling: The most common symptom of a seroma is a noticeable swelling or lump at or near the surgical site. This can vary in size and may increase over time if the seroma is not resolved.
Pain or Discomfort: While seromas are not always painful, they can cause discomfort, especially if they press against nerves or surrounding tissues.
Redness or Warmth: Although these symptoms are more characteristic of an infection, they can sometimes occur with a seroma. If the area is also tender to the touch, this could be a sign of infection and should be evaluated by a physician.
Fluid Leakage: In some cases, the seroma may leak through the surgical incision or the skin.
Treatment of Seroma in the Spine:
Observation: Small seromas often resolve on their own as the body reabsorbs the fluid. Doctors may take a wait-and-see approach, monitoring the seroma for changes.
Aspiration: Larger or symptomatic seromas may require aspiration, where a needle is used to draw out the accumulated fluid. This procedure is typically done under sterile conditions to reduce the risk of infection.
Drainage: In cases where the seroma continues to recur or is quite large, a surgical drain might be temporarily placed to continuously remove fluid from the site.
Antibiotics: While seromas are not infections, if there is an infection or a high risk of one, antibiotics may be prescribed.
Surgical Intervention: On rare occasions, particularly if the seroma does not resolve or there are complications, additional surgery may be req
MRI Appearance of Seroma
- T1-Weighted Images: On T1-weighted MRI sequences, seromas typically appear as well-defined structures with low to intermediate signal intensity, which means they are darker than fat but can be brighter than muscle. This is because the serous fluid within a seroma has a protein content that is different from that of other tissues, such as cysts which are often very low in protein and appear darker on T1.
- T2-Weighted Images: In T2-weighted images, seromas usually exhibit high signal intensity, causing them to appear bright. This is attributed to the high water content of the serous fluid.
- STIR (Short Tau Inversion Recovery): In STIR images, seromas also present with high signal intensity, consequently appearing bright. STIR is a fluid-sensitive sequence with fat suppression that aids in distinguishing fluid collections from fatty tissues. Because fat signal is suppressed, any fluid collection, such as a seroma, becomes more prominent with increased contrast. This sequence is particularly valuable in cases where a seroma is adjacent to fatty tissue, as it facilitates differentiation between the two.
The presence of blood within a seroma can alter its appearance on MRI:
- On T1-weighted images, fresh blood within a seroma can appear bright due to the methemoglobin stage of hemoglobin breakdown, which is more common in subacute hematomas. Over time, as the blood products within the seroma change, the intensity may vary.
- On T2-weighted images, the signal intensity of a seroma containing blood will depend on the age of the hematoma. Acute blood may appear dark due to the presence of deoxyhemoglobin
T2 TSE sagittal image shows seroma
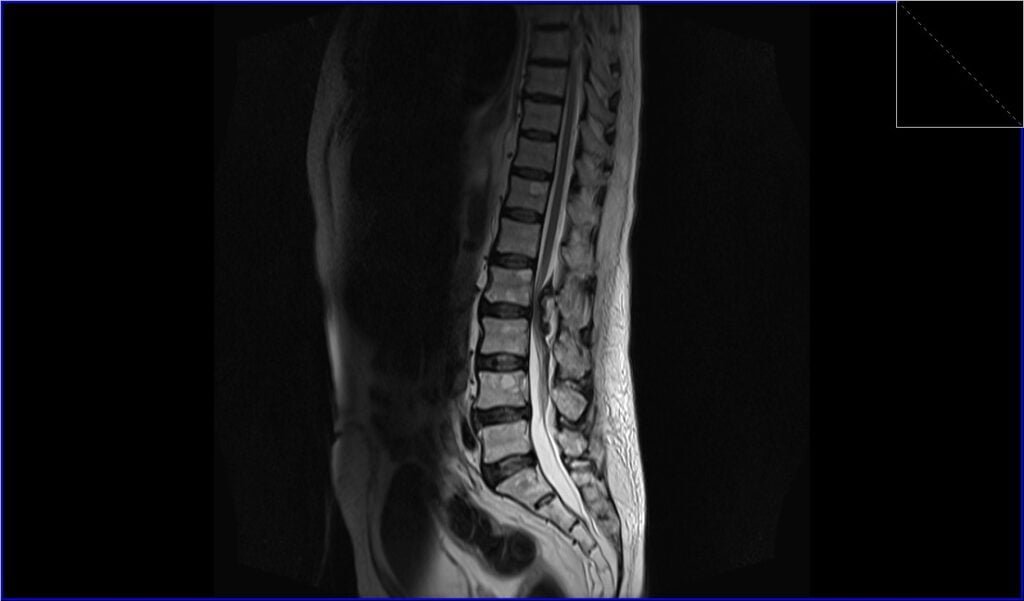
STIR sagittal image shows seroma

T1 TSE sagittal image shows seroma

T2 TSE axial image shows seroma

T1 TSE axial image shows seroma

References
- Malhotra, A., Kalra, V. B., Wu, X., Grant, R., Bronen, R. A., & Abbed, K. M. (2015). Imaging of lumbar spinal surgery complications. Insights Imaging, 6(6), 579–590. doi: 10.1007/s13244-015-0435-8. PMID: 26432098. PMC ID: PMC4656239.
- Davies, A. M., Hall, A. D., Strouhal, P. D., Evans, N., & Grimer, R. J. (2004). The MR imaging appearances and natural history of seromas following excision of soft tissue tumors. European Radiology, 14(7), 1196-1202. doi: 10.1007/s00330-004-2255-y. Epub 2004 Mar 9. PMID: 15007612.
- Jeon, S. H., Shin, K. H., Park, S.-Y., Kim, J.-I., Park, J. M., Kim, J. H., Chie, E. K., & Wu, H.-G. (2017). Seroma change during magnetic resonance imaging-guided partial breast irradiation and its clinical implications. Radiation Oncology, 12, 103. doi:10.1186/s13014-017-0843-2
- Poon-Chue, A., Menendez, L., Gerstner, M. M., Colletti, P., & Terk, M. (1999). MRI evaluation of post-operative seromas in extremity soft tissue sarcomas. Skeletal Radiology, 28(3), 279–282.
- Jeon, S.H., Shin, K.H., Park, S.Y., Kim, J.H., Chie, E.K., & Wu, H.G. (2017). Seroma Change during Magnetic Resonance Imaging-Guided Partial Breast Irradiation and Its Clinical Implications. Poster viewing, Volume 99, Issue 2, Supplement, E674, October 01, 2017. International Journal of Radiation Oncology, Biology, Physics, 99(2), e674.
- Baroudi, R., & Ferreira, C. A. A. (1998). Seroma: How to Avoid It and How to Treat It. Aesthetic Surgery Journal, 18(6), 439–441. https://doi.org/10.1016/S1090-820X(98)70073-1


