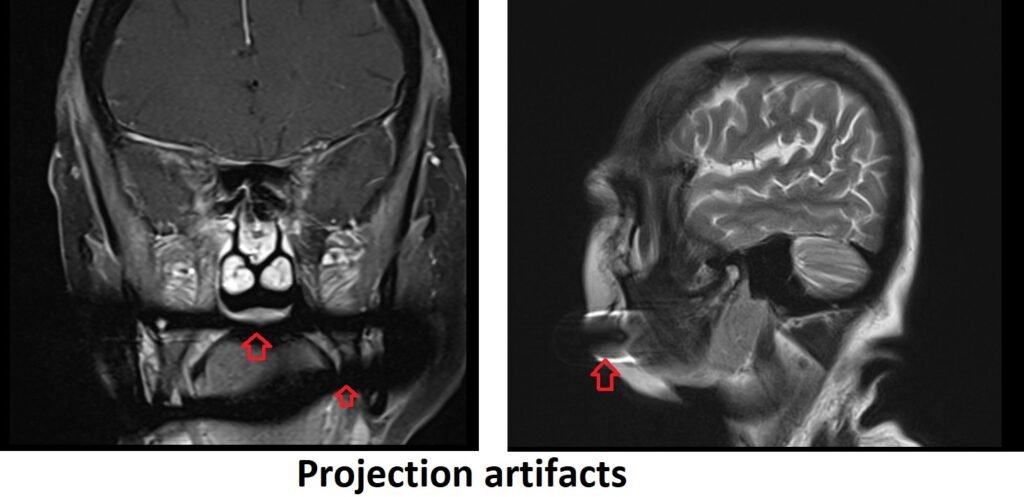
Projection Artifact MRI
Projection artifacts in MRI refer to imaging artifacts that occur due to the presence of objects or structures outside the imaging plane that cast a signal onto the image. These artifacts can appear as bright or dark streaks, shadows, or ghosting effects in the image. They can obscure or distort the true anatomical information and affect the diagnostic quality of the image.
Projection artifacts can arise from several sources, including:
Metallic objects: Metallic implants, such as orthopedic implants, surgical clips, or dental fillings, can cause significant signal distortions and susceptibility artifacts. These artifacts can extend beyond the implant itself, creating streaking or shading artifacts in the image.
Patient-related objects: External objects like jewelry, clothing accessories, or patient positioning devices can also lead to projection artifacts if they are within the imaging field of view and interact with the magnetic field.
RF coil-related artifacts: Poorly positioned or improperly tuned radiofrequency (RF) coils can cause shading or streaking artifacts in the images. These artifacts can occur when the coil sensitivity is not uniform or when the coil is too close to a high-signal-intensity structure.
Minimizing projection artifacts in MRI involves several strategies:
Patient screening: Thoroughly screen patients for any metallic objects, implants, or external accessories that could potentially cause artifacts. Obtain detailed patient histories to identify any contraindications or potential sources of artifacts.
RF coil optimization: Carefully position and optimize the RF coils to achieve uniform sensitivity and minimize artifacts related to coil interaction. Adjust coil positioning or use alternative coil configurations if necessary.
Sequence selection: Choose MRI sequences that are less susceptible to projection artifacts, such as spin-echo sequences. Avoid using sequences highly sensitive to susceptibility effects, such as gradient-echo or echo-planar imaging (EPI), when artifacts are anticipated.
References:
- Weinreb JC, et al. Artifacts in MR imaging: recognition and avoidance. Radiographics. 2010;30(3):893-901. (https://pubs.rsna.org/doi/full/10.1148/rg.303095174)
- Bydder GM, et al. Artefacts in imaging: explanations and solutions. Insights Imaging. 2011;2(4):373-386. (https://link.springer.com/article/10.1007/s13244-011-0102-z)
- Lewin JS, et al. Clinical MRI artifacts. AJR Am J Roentgenol. 2007;189(6):W38-45. (https://www.ajronline.org/doi/full/10.2214/AJR.07.2294)


