Pelvic osteomyelitis MRI
Pelvic osteomyelitis refers to an infection of the bone in the pelvic area. This type of osteomyelitis can be quite serious due to the pelvic bones’ critical role in structural support and their proximity to various vital organs.
Causes
Pelvic osteomyelitis is typically caused by bacteria, although it can occasionally be due to fungal or other types of infections. The most common bacteria involved are Staphylococcus aureus. The infection can reach the pelvic bone through various routes:
- Hematogenous spread, where bacteria spread through the bloodstream from another infected site.
- Direct infection, due to trauma, surgery, or an open wound.
- Spread from nearby infections, such as in the urinary tract or intra-abdominal infections.
Symptoms
The symptoms of pelvic osteomyelitis can vary but typically include:
- Pain in the pelvic area, hip, or back
- Fever and chills
- Swelling, warmth, and redness over the pelvis
- General malaise or feeling unwell
- Restricted movement due to pain
Diagnosis
- Clinical Evaluation: Thorough history and physical examination.
- Blood Tests: Elevated white blood cell count, increased inflammatory markers such as ESR (erythrocyte sedimentation rate) and CRP (C-reactive protein).
- Blood Cultures: To identify the causative organism.
- Imaging:
- X-rays: Initial imaging, though early stages may not show changes.
- MRI: More sensitive in detecting early changes and soft tissue involvement.
- CT Scan: Useful for assessing bone destruction and guiding biopsies.
- Biopsy: Bone biopsy to confirm the diagnosis and identify the causative organism.
Treatment
Treatment for pelvic osteomyelitis usually involves:
- Antibiotics: Prolonged courses of antibiotics that may initially be administered intravenously and later switched to oral forms. The choice of antibiotics depends on the suspected or confirmed bacteria.
- Surgery: In severe cases, surgery might be required to remove infected bone tissue, drain abscesses, or stabilize the bone structure.
MRI Appearance of pelvic osteomyelitis
T1 Appearance of Spinal Metastases
On T1-weighted MRI sequences, spinal metastases typically appear as areas of low signal intensity compared to the normal high signal intensity of the fatty bone marrow. This signal decrease is due to the replacement of fatty marrow by tumor cells, which contain more water and less fat. The metastatic lesions often appear as hypointense (dark) spots within the vertebral bodies, and the extent of these lesions can vary from focal areas to diffuse involvement. T1 imaging is particularly useful for detecting changes in the bone marrow composition and for delineating the anatomical details of the spine.
T2 Appearance of Spinal Metastases
In T2-weighted MRI sequences, spinal metastases usually exhibit high signal intensity relative to the normal bone marrow. This hyperintense (bright) signal is attributed to the increased water content within the metastatic lesions, resulting from the presence of tumor cells, edema, and potential inflammatory response. T2 imaging is effective in highlighting the lesions against the background of normal spinal structures and is instrumental in identifying the extent of metastatic disease, including any involvement of the spinal canal, paraspinal tissues, and intervertebral discs.
STIR Appearance of Spinal Metastases
Short Tau Inversion Recovery (STIR) sequences in MRI are highly sensitive for detecting spinal metastases due to their ability to suppress the signal from fat, making the lesions stand out more clearly. On STIR images, spinal metastases typically appear as areas of high signal intensity against a dark background of suppressed fatty bone marrow. This sequence is particularly useful in identifying small lesions, detecting marrow edema, and evaluating the extent of metastatic involvement. STIR is an essential tool for the comprehensive assessment of metastatic disease in the spine, providing high contrast between normal and pathological tissues.
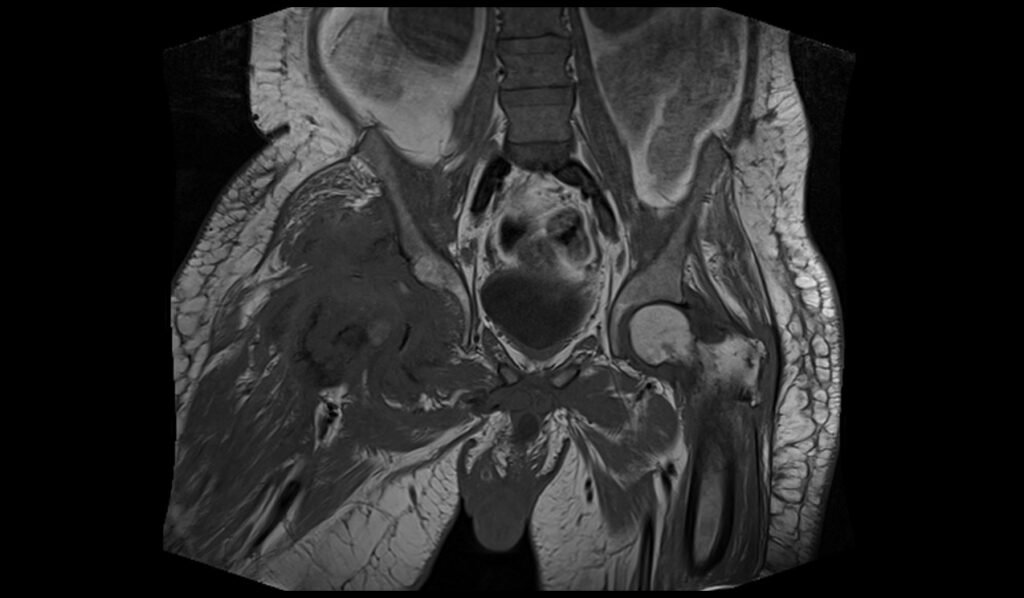
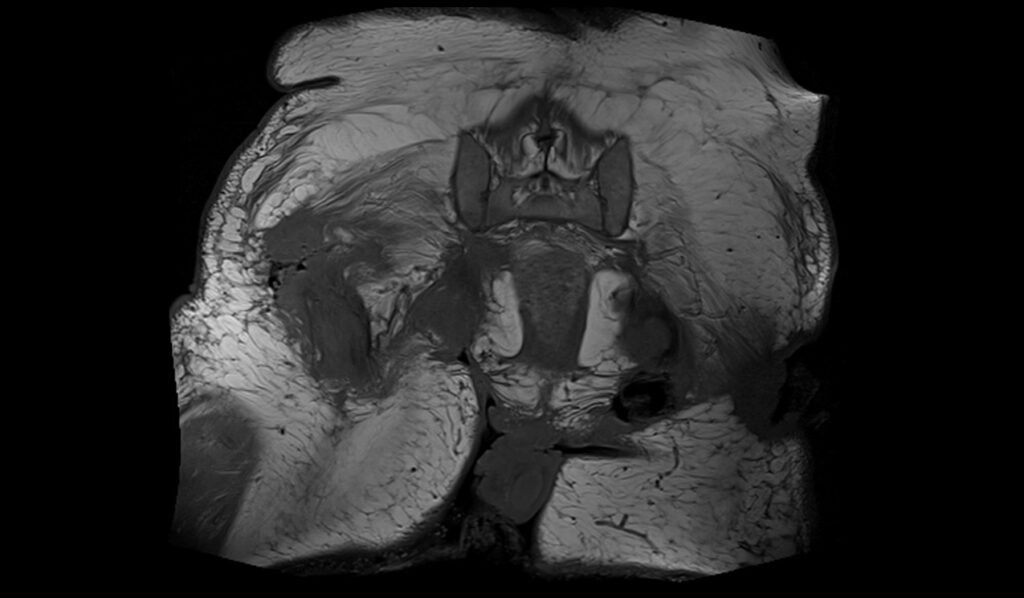
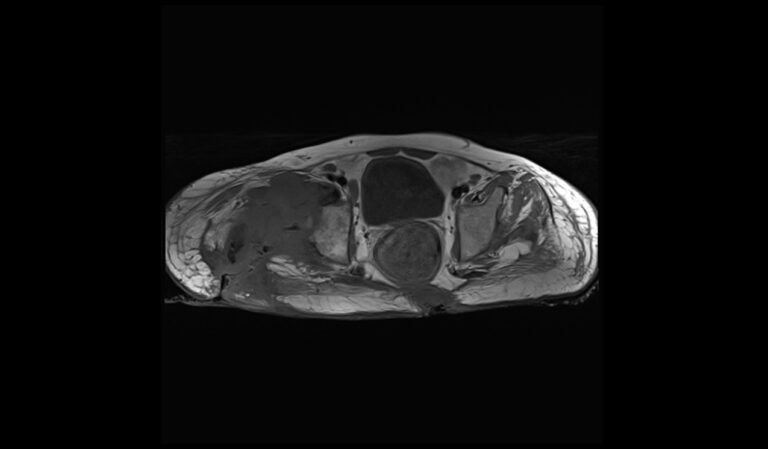
STIR coronal image of pelvis shows pelvic osteomyelitis




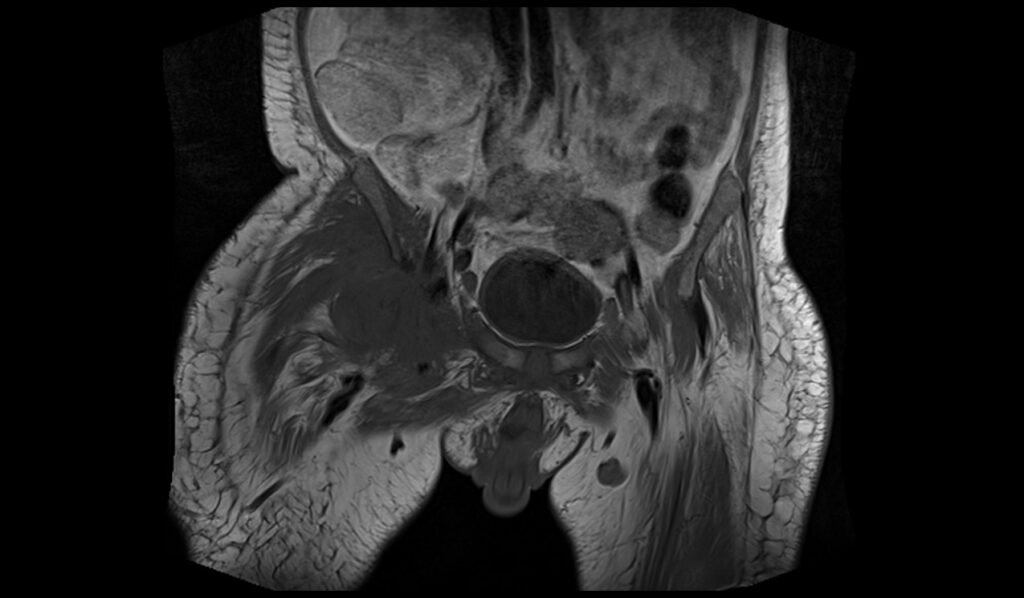
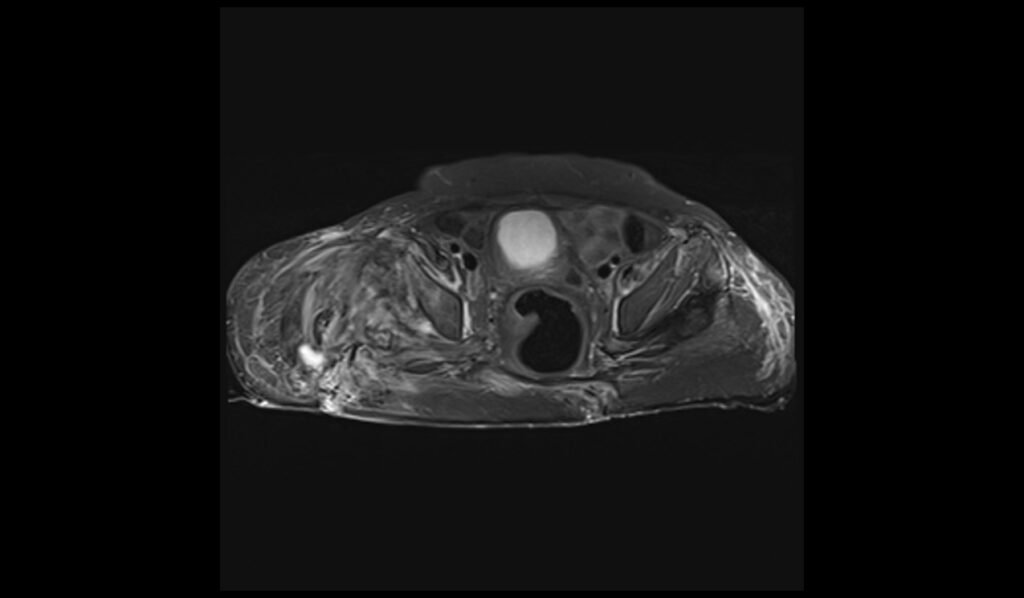
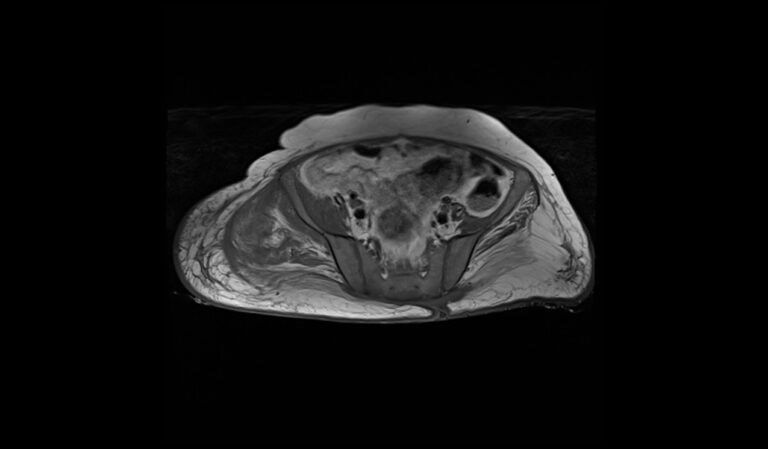
T1 TSE coronal image of pelvis shows pelvic osteomyelitis

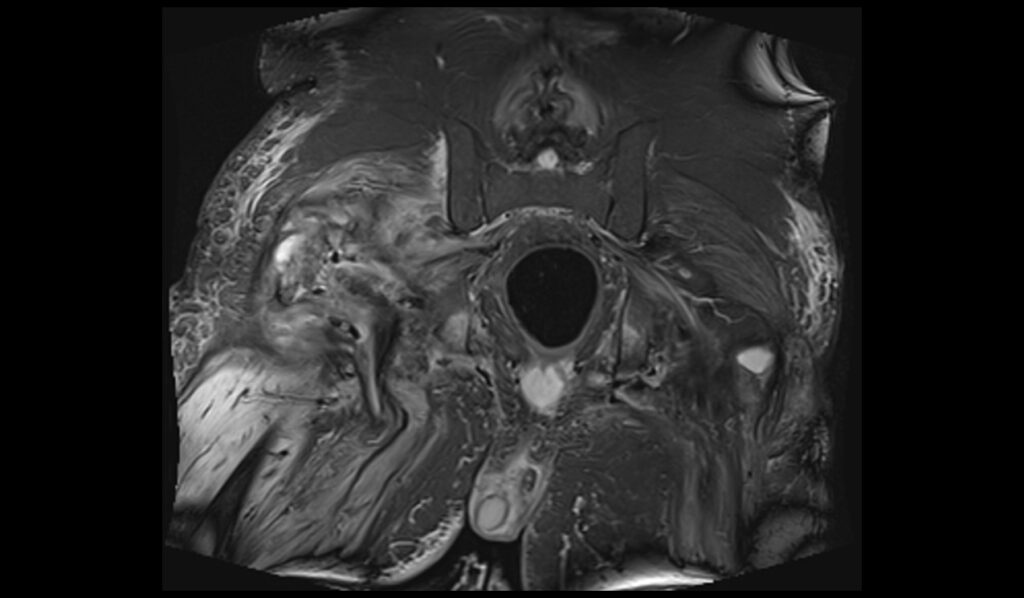
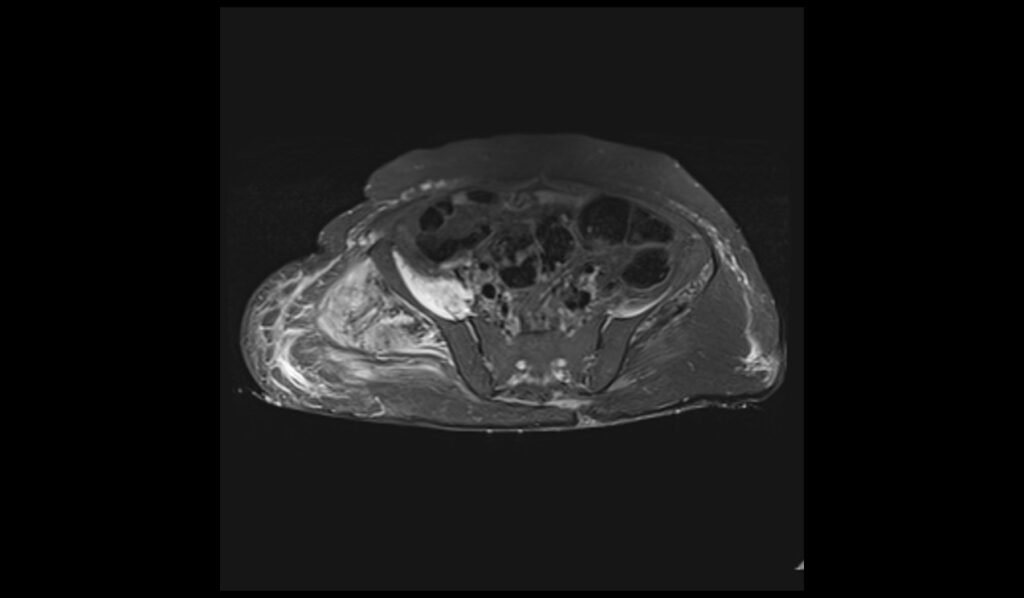
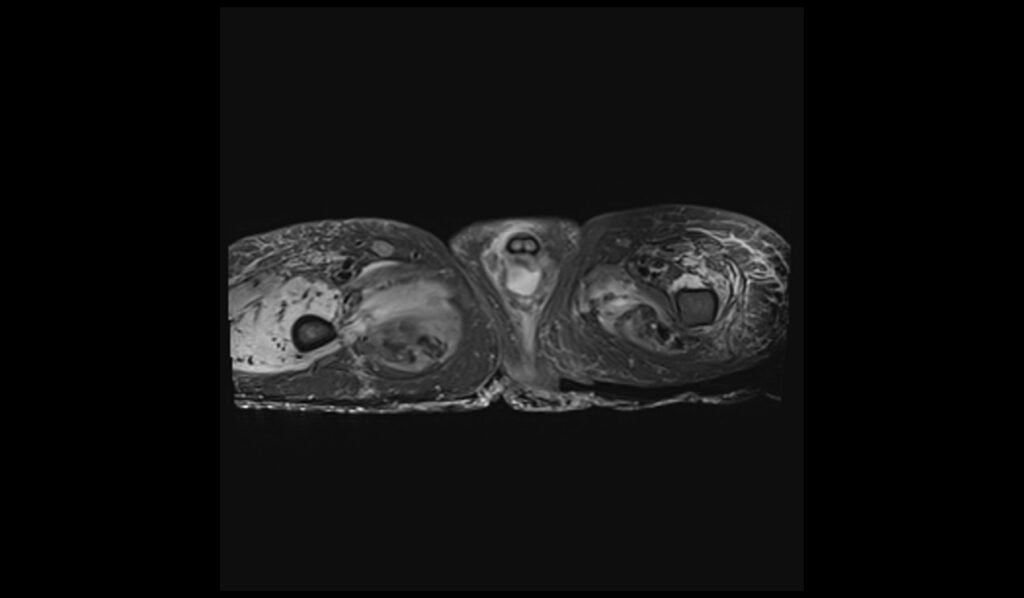
STIR axial image of pelvis shows pelvic osteomyelitis
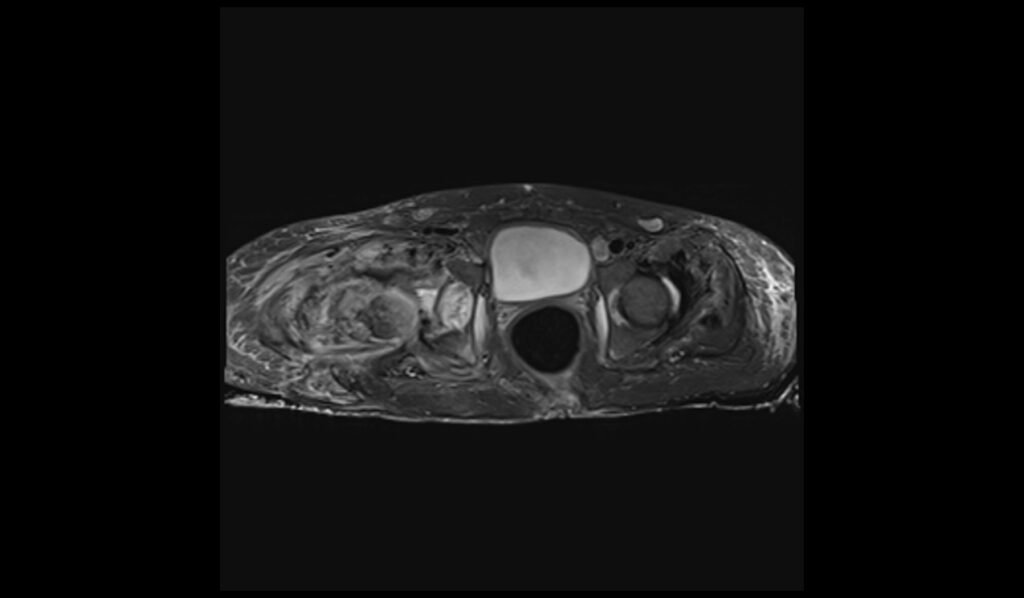

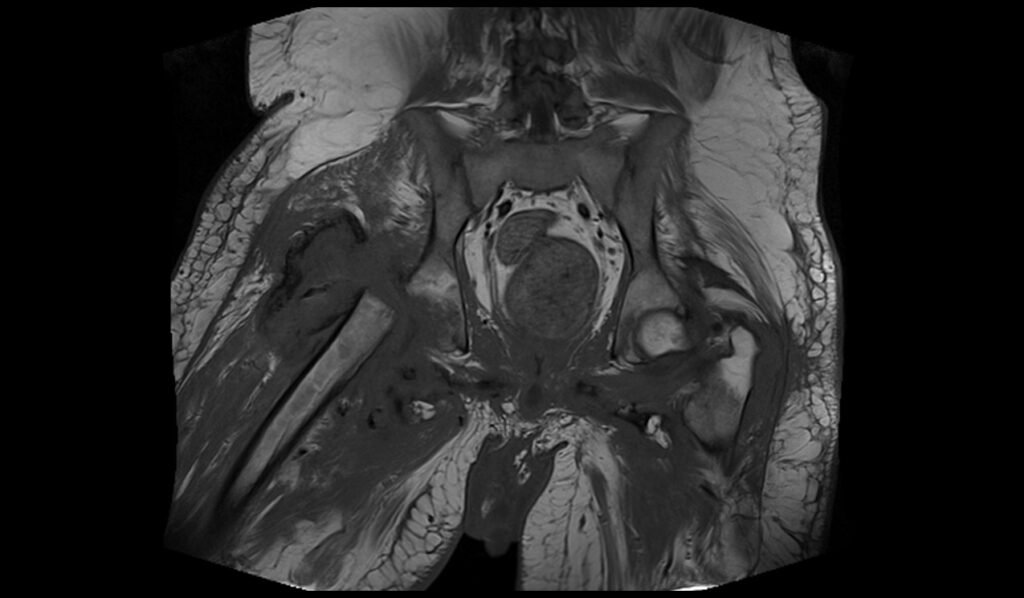
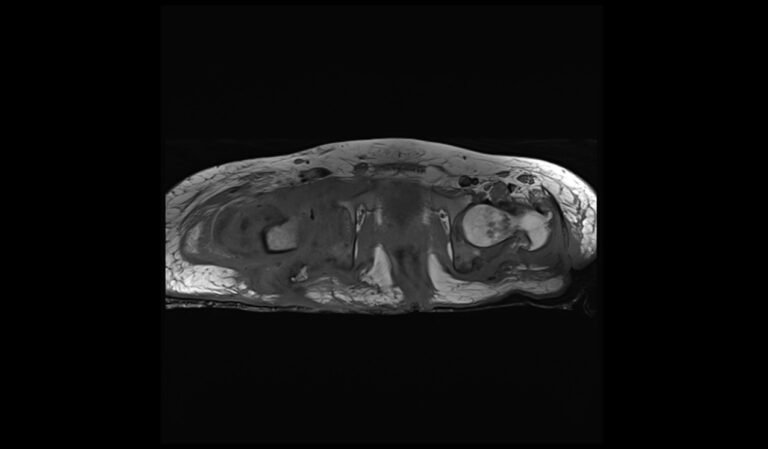
T1 TSE axial image of lumbar spine shows spinal metastases
References
- Deore, S., & Bansal, M. (2018). Pelvic osteomyelitis in a child – A diagnostic dilemma. Journal of Orthopaedic Case Reports, 8(4), 86-88.
- McPhee, E., Eskander, J. P., Eskander, M. S., Mahan, S. T., & Mortimer, E. (2007). Imaging in pelvic osteomyelitis: Support for early magnetic resonance imaging. Journal of Pediatric Orthopaedics, 27(8), 903-909.
- Connolly, S. A., Connolly, L. P., Drubach, L. A., Zurakowski, D., & Jaramillo, D. (2007). MRI for detection of abscess in acute osteomyelitis of the pelvis in children. American Journal of Roentgenology, 189(4). https://doi.org/10.2214/AJR.07.2416
- Tolley, M., Morris, A., & Williams, N. (2017). Pelvic osteomyelitis: Three unusual cases with predominantly abdominal symptoms. Journal of Paediatrics and Child Health. https://doi.org/10.1111/jpc.13533


