MRI Patellar Dislocation
A patellar dislocation occurs when the kneecap (patella) slips out of its normal position, usually to the side of the knee. This can result in pain, swelling, and difficulty moving the knee.
Causes
- Trauma: Direct impact to the knee, such as during a fall or collision.
- Sudden Twisting Movements: Rapid changes in direction or twisting motions, common in sports, can dislocate the patella.
- Weak or Imbalanced Muscles: Imbalance in the muscles around the knee, particularly the quadriceps, can increase the risk.
- Structural Abnormalities: Conditions such as a shallow trochlear groove (the groove in which the patella sits) or a high-riding patella (patella alta).
- Previous Dislocation: A history of patellar dislocation can weaken the structures around the knee, making recurrence more likely.
Symptoms
- Pain: Sudden, intense pain at the front of the knee.
- Swelling: Rapid swelling around the knee.
- Visible Deformity: The kneecap may be visibly out of place.
- Inability to Straighten the Knee: Difficulty in extending the knee fully.
- Feeling of Instability: The knee may feel unstable or give way.
- Tenderness: Tenderness along the edges of the patella and around the knee.
Diagnosis:
- Physical Examination: Checking for signs of dislocation, swelling, and tenderness.
- Imaging:
- X-rays: To assess the position of the patella and check for associated fractures.
- MRI: Provides detailed images of soft tissues, including ligaments and cartilage, to identify any additional injuries or predisposing factors.
Treatment:
- Reduction: The initial step is to manually guide the patella back into place, usually performed by a medical professional.
- Immobilization: Using a brace or cast to keep the knee stable and allow healing.
- Physical Therapy: Strengthening the muscles around the knee, improving flexibility, and restoring range of motion.
- Surgery: In cases of recurrent dislocation or when conservative treatments fail, surgical options may be considered. Procedures can include:
- Lateral Release: Cutting tight structures on the outer knee to allow the patella to move more freely.
- Medial Patellofemoral Ligament Reconstruction: Rebuilding the ligament that helps keep the patella in place.
- Osteotomy: Realigning the bones to improve patella tracking
MRI Appearance of Patellar Dislocation
T1 weighted Sequence
- Dislocation: The patella appears out of its normal position, often laterally displaced.
- Bone Contusions: There may be visible bone marrow edema in the lateral femoral condyle and the medial patella as areas of low signal intensity.
- Medial Retinaculum and Medial Patellofemoral Ligament (MPFL): Potential tears or injuries might appear as irregularities or discontinuities in these structures.
Proton Density (PD) Fat Saturation (Fat Sat) Sequence
- Dislocation: The patella’s abnormal position will be clearly seen, usually with lateral displacement.
- Bone Marrow Edema: Enhanced visualization of bone marrow edema in the lateral femoral condyle and medial patella as high signal intensity areas due to the fat suppression technique.
- Soft Tissue Structures: Injuries to the MPFL and medial retinaculum appear more conspicuous, showing as high signal intensity due to the increased fluid content from acute injury.
- Joint Effusion: Increased fluid within the joint space will be seen as high signal intensity.
Short Tau Inversion Recovery (STIR) Sequence
- Dislocation: The patella remains visibly out of place.
- Bone Marrow Edema: Enhanced detection of bone marrow edema in the affected bones due to the high sensitivity of STIR to fluid, showing as very high signal intensity areas.
- Soft Tissue Edema: The presence of edema in the surrounding soft tissues, including the medial retinaculum and MPFL, will appear as areas of high signal intensity.
- Joint Effusion: Like in PD Fat Sat, joint effusion will be prominently seen as high signal intensity.
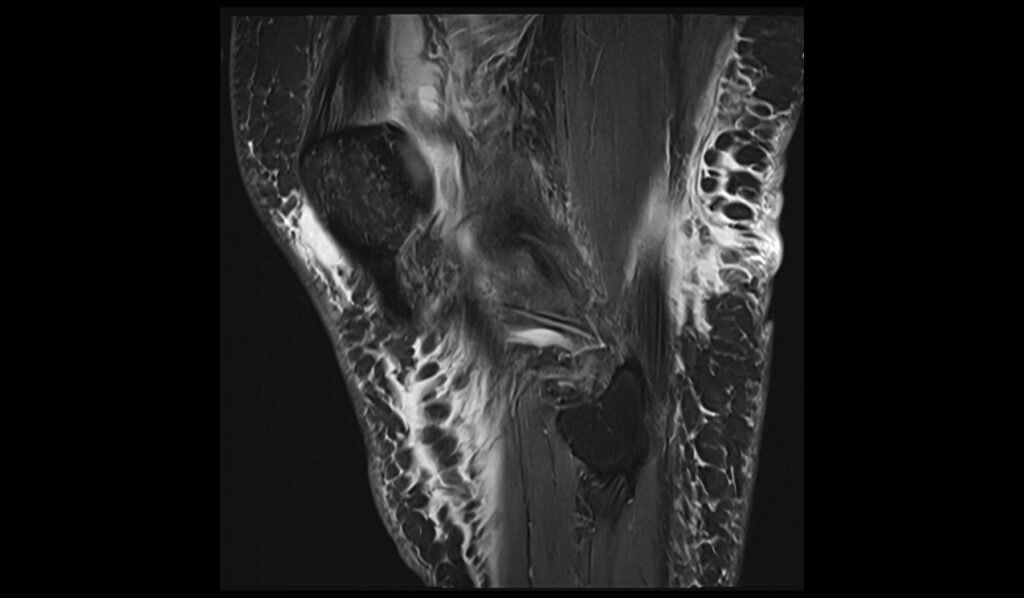
T1 TSE sagittal image shows Patellar Dislocation



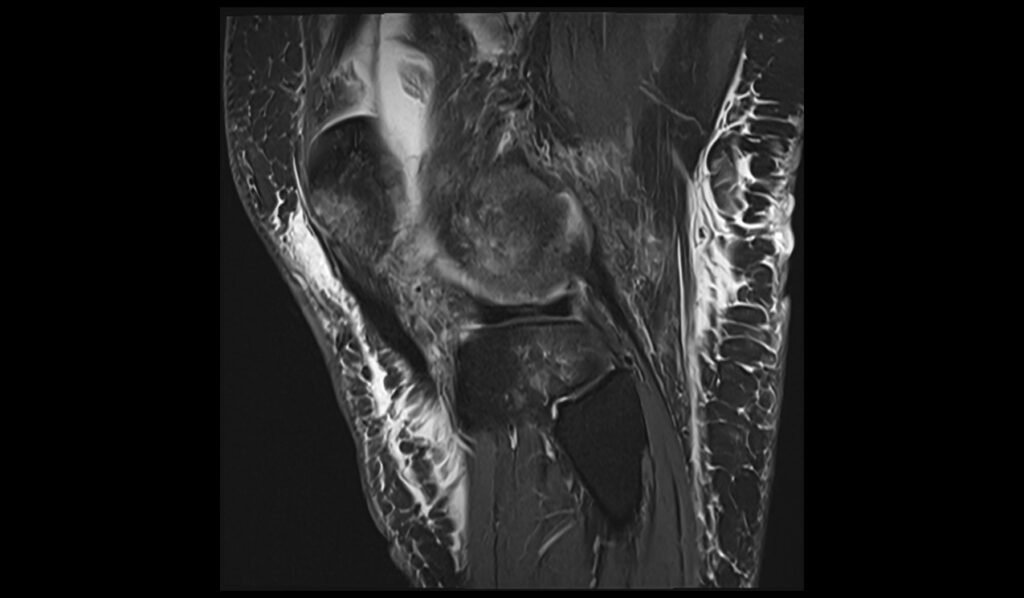
STIR sagittal image shows Patellar Dislocation

PD fat saturated coronal shows Patellar Dislocation


PD fat saturated axial image shows Patellar Dislocation

References
- Mohan K, Ellanti P, Lincoln M, McCarthy T. Magnetic Resonance Imaging Features of Traumatic Patellofemoral Dislocation. Cureus. 2018 Dec 14;10(12):e3730. doi: 10.7759/cureus.3730. PMID: 30800540; PMCID: PMC6384034.
- Diederichs, G., Issever, A. S., & Scheffler, S. (2010). MR imaging of patellar instability: Injury patterns and assessment of risk factors. RadioGraphics, 30(4). https://doi.org/10.1148/rg.304095755
- Tsai, C.-H., Hsu, C.-J., Hung, C.-H., & Hsu, H.-C. (2012). Primary traumatic patellar dislocation. Journal of Orthopaedic Surgery and Research, 7, Article 21. https://doi.org/10.1186/1749-799X-7-21


