Pachygyria MRI
Pachygyria is a neurological condition characterized by abnormal development of the brain, where the brain’s surface has unusually thick convolutions (gyri) and shallow grooves (sulci). This developmental anomaly leads to a smooth and simplified brain structure, which can impact various neurological functions.
Causes
Pachygyria is primarily caused by disruptions in brain development during the early stages of fetal growth. Several factors can contribute to this condition, including:
- Genetic Mutations: Mutations in specific genes that regulate neuronal migration and cortical development.
- Prenatal Infections: Infections during pregnancy, such as cytomegalovirus (CMV) or toxoplasmosis, can interfere with normal brain development.
- Toxic Exposures: Exposure to certain toxins, drugs, or alcohol during pregnancy.
- Blood Flow Issues: Problems with blood supply to the fetal brain during critical periods of development.
Symptoms
The symptoms of pachygyria can vary widely in severity, depending on the extent and location of the abnormal brain development. Common symptoms include:
- Developmental Delays: Delays in reaching developmental milestones such as sitting, walking, or talking.
- Intellectual Disability: Ranging from mild to severe cognitive impairment.
- Seizures: Frequent and often difficult-to-control seizures.
- Motor Dysfunction: Weakness, spasticity, or poor coordination of muscles.
- Speech and Language Difficulties: Problems with speech articulation and language comprehension.
- Behavioral Issues: Hyperactivity, aggression, or other behavioral problems.
Diagnosis
Diagnosing pachygyria involves a combination of clinical evaluation and neuroimaging techniques. The diagnostic process typically includes:
- Clinical Assessment: Evaluating developmental history, physical and neurological examinations.
- Magnetic Resonance Imaging (MRI): MRI scans are crucial for visualizing the brain’s structure and identifying the characteristic thickened gyri and shallow sulci.
- Genetic Testing: Testing for known genetic mutations associated with pachygyria.
- Electroencephalogram (EEG): Used to assess brain activity, especially if seizures are present.
Treatment
There is no cure for pachygyria, and treatment focuses on managing symptoms and improving quality of life. Treatment strategies include:
- Seizure Management: Antiepileptic medications to control seizures. In some cases, surgical interventions might be considered.
- Therapies:
- Physical Therapy: To improve motor skills and muscle strength.
- Occupational Therapy: To enhance daily living skills and independence.
- Speech Therapy: To address speech and language difficulties.
- Educational Support: Special education programs tailored to the child’s cognitive and developmental needs.
- Behavioral Therapy: To manage behavioral issues and support social skills development.
MRI appearance of Pachygyria
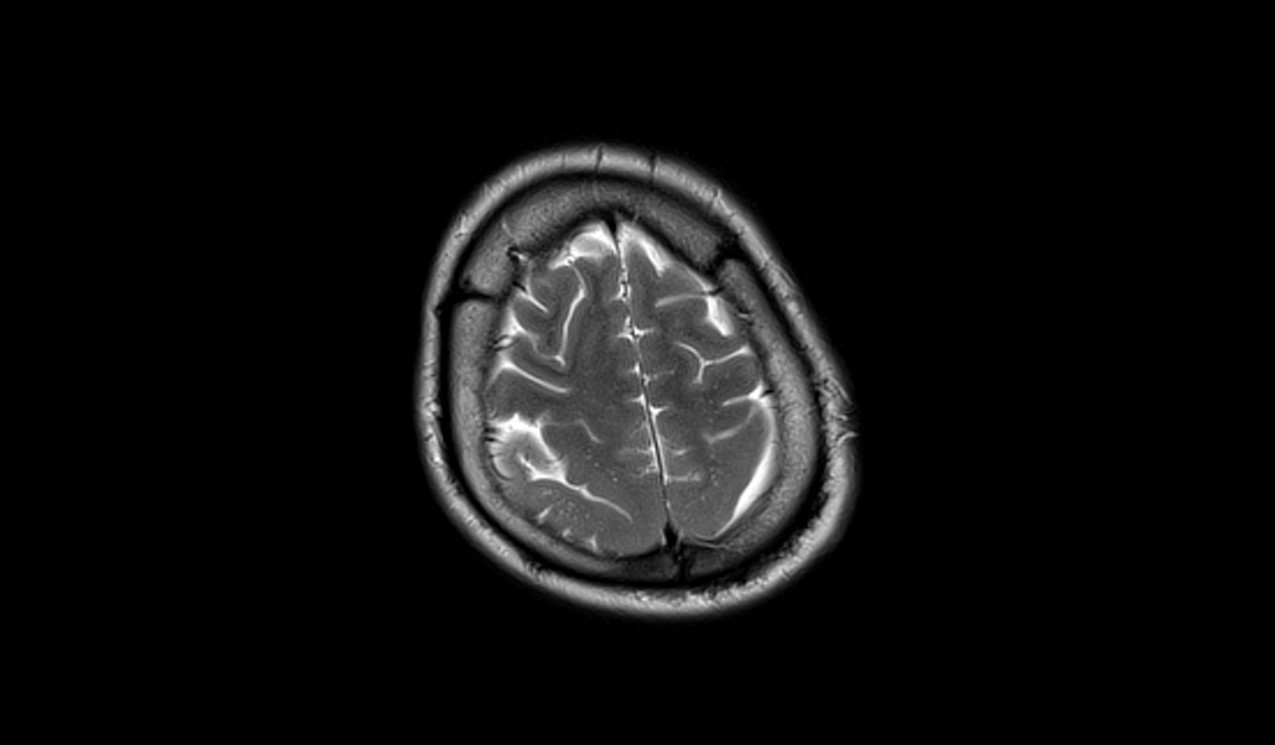
MRI T1 Appearance of Pachygyria
On T1-weighted MRI, pachygyria appears as areas with abnormal cortical thickening and a smooth cortical surface, with broad, flattened gyri. The grey matter may appear slightly hyperintense compared to normal white matter. The differentiation between grey and white matter might be less distinct than usual due to the disrupted cortical development. T1-weighted images are particularly useful for providing detailed anatomical views, allowing the identification of the extent and distribution of the pachygyria.
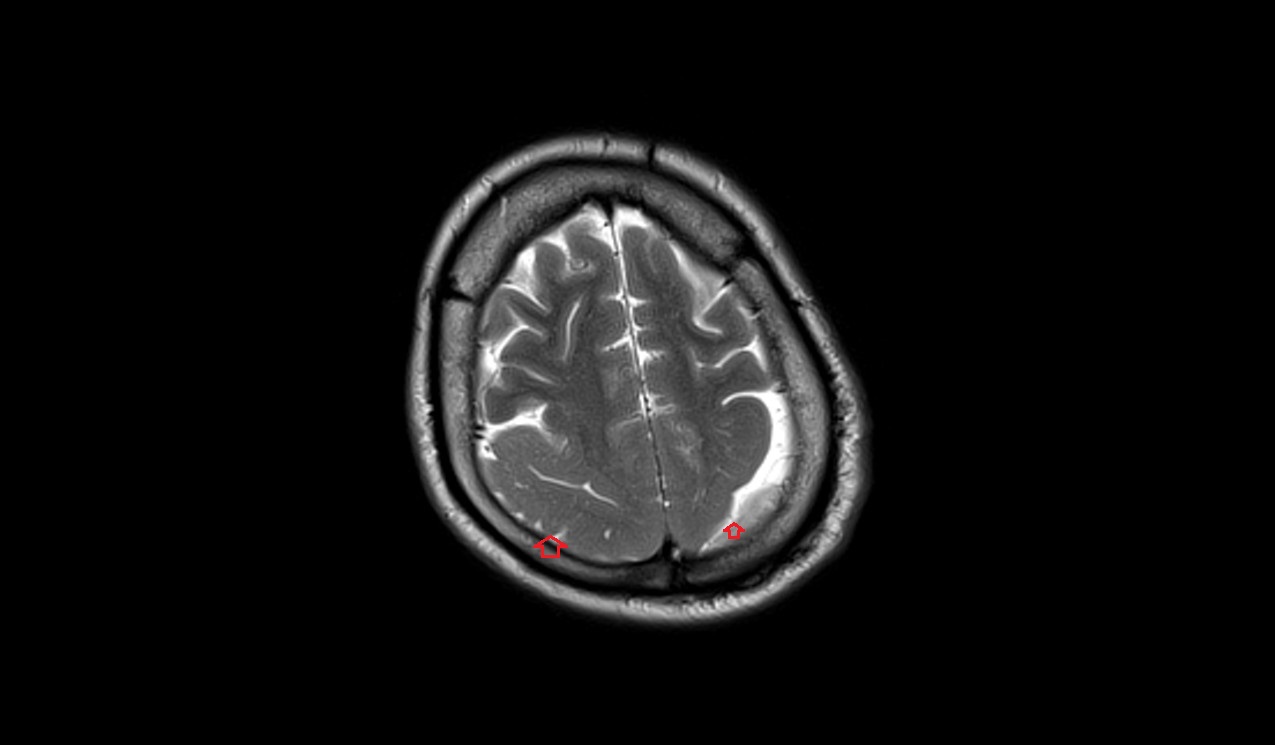
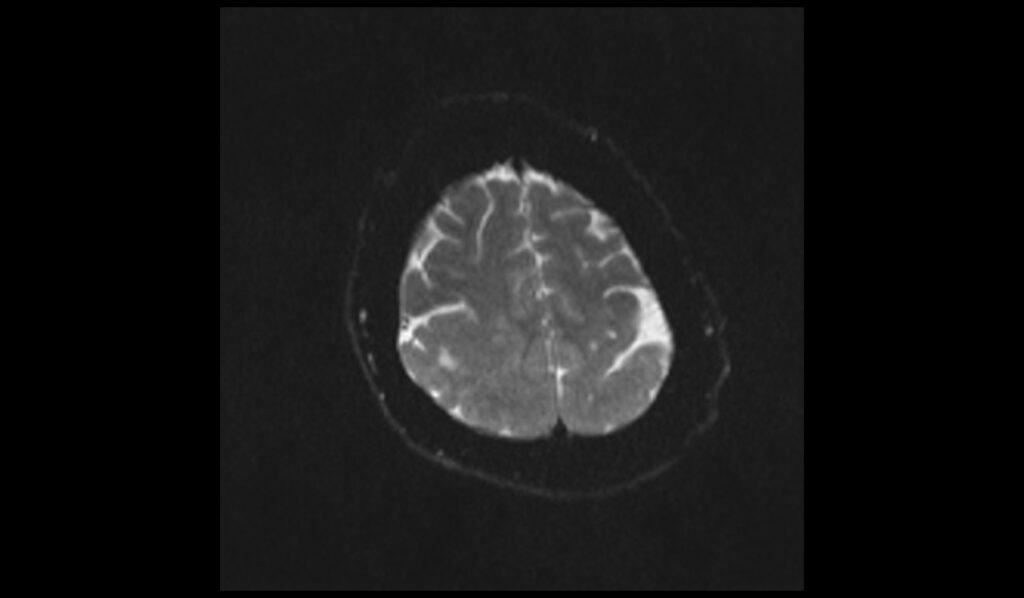
MRI T2 Appearance of Pachygyria
T2-weighted MRI images of pachygyria reveal thickened cortical regions with broad and smooth gyri, often more clearly showing the extent of the abnormal cortical architecture. These regions typically appear hyperintense compared to the normal cortex. The T2 images help highlight the altered white matter signal intensity adjacent to the malformed cortex, which can assist in assessing the severity and distribution of the pachygyria.
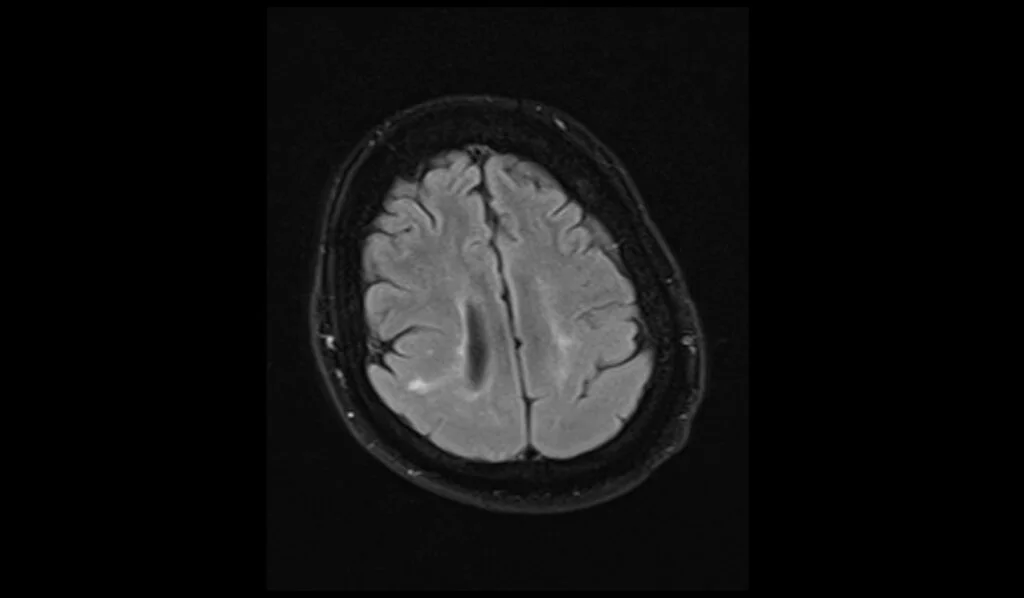
MRI FLAIR Appearance of Pachygyria
FLAIR (Fluid-Attenuated Inversion Recovery) MRI sequences provide enhanced contrast between lesions and cerebrospinal fluid (CSF), making them particularly useful for visualizing pachygyria. In FLAIR images, the thickened and smooth cortical regions characteristic of pachygyria appear hyperintense, with the abnormal cortical pattern standing out clearly against the suppressed CSF background. This sequence is useful for identifying associated white matter changes and other abnormalities often seen with cortical malformations.
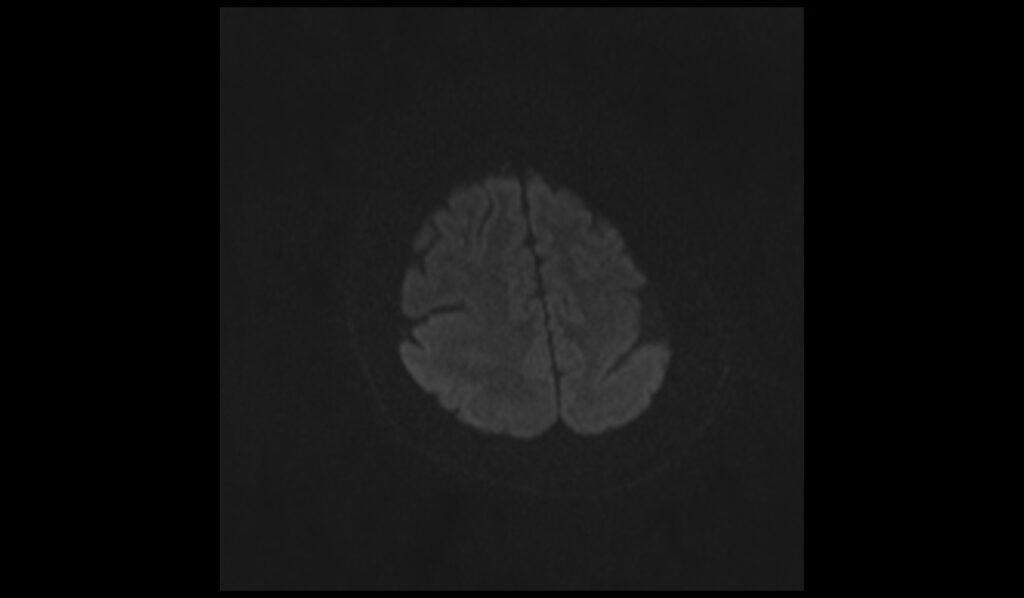
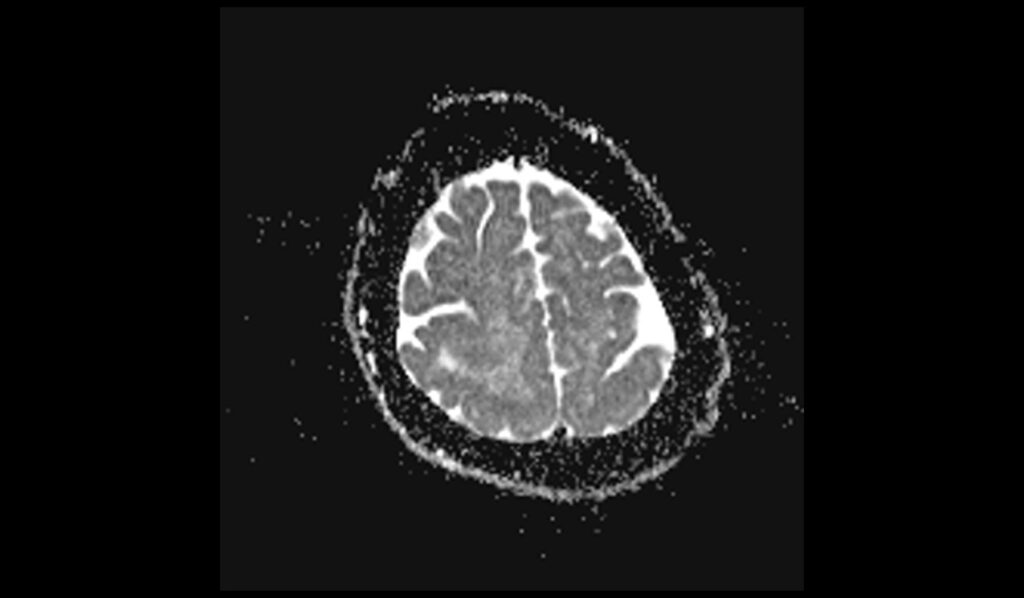
DWI (Diffusion-Weighted Imaging) and ADC (Apparent Diffusion Coefficient)
On DWI with b0 and b1000 sequences, areas of pachygyria typically do not show diffusion restriction unless there is an associated pathology like an acute ischemic event. The ADC maps reflect these findings, usually showing no significant abnormalities in diffusion, but there can be subtle changes depending on the underlying cellular and structural abnormalities in the malformed cortex.
T2 axial image shows Pachygyria

FLAIR axial image shows Pachygyria

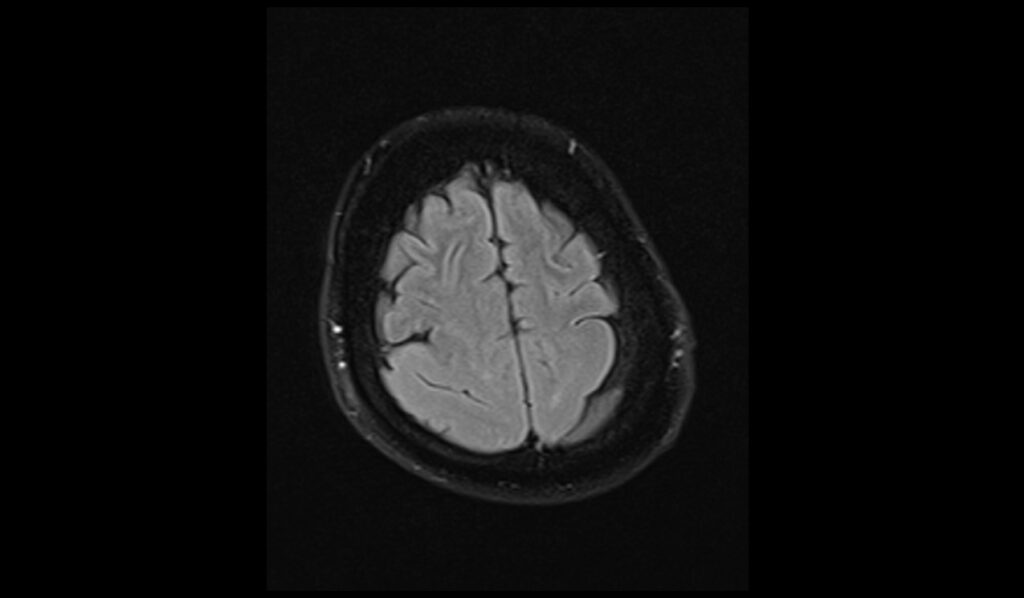
DWI b0 images shows Pachygyria
DWI b1000 images shows Pachygyria
DWI ADC images shows Pachygyria
References
- Byrd, S. E., Osborn, R. E., & Radkowski, M. A. (1991). The MR evaluation of pachygyria and associated syndromes. European Journal of Radiology, 12(1), 53-59.
- El Houssni, J., El Haddad, S., Chat, L., & Nazik, A. (2022). Pachygyria with cerebellar hypoplasia and tigroid pattern of the white matter secondary to neuronal migration disorders. Edorium Journal of Radiology, Article ID: 101343Z01EJ2022.


