Neurocysticercosis MRI
Neurocysticercosis is a serious, potentially life-threatening condition that occurs when the larval form of the pork tapeworm, Taenia solium, infects the brain. It is the most common parasitic infection of the central nervous system and a major cause of adult-onset seizures in developing countries.
Cause
Neurocysticercosis is caused by the ingestion of eggs from Taenia solium. These eggs are generally spread through food, water, or surfaces contaminated with feces from a person who has an intestinal tapeworm. Once ingested, the eggs hatch in the intestines, and the larvae can enter the bloodstream and migrate to the brain and other tissues, where they form cysts.
Symptoms
The symptoms of neurocysticercosis vary depending on the location and number of cysts in the brain. Common symptoms include:
- Seizures, which are the most frequent sign and often the first symptom noticed.
- Headaches, often caused by increased pressure within the brain.
- Confusion or difficulty with attention and memory.
- Balance problems or difficulty walking.
- Vision changes, depending on the cyst’s location.
Diagnosis
Diagnosis of neurocysticercosis involves a combination of imaging techniques and serological tests:
- Imaging tests: MRI (Magnetic Resonance Imaging) or CT (Computed Tomography) scans are used to visualize cysts in the brain.
- Blood tests: Serological tests can detect antibodies or antigens related to Taenia solium.
- Cerebrospinal fluid (CSF) analysis: This may show inflammatory changes typical of infection.
Treatment
Treatment for neurocysticercosis includes:
- Antiparasitic medication: Drugs like albendazole or praziquantel are used to kill the cysts, although their use must be carefully managed to avoid causing inflammation as the cysts die.
- Steroids: These are often given to reduce inflammation caused by the dying cysts.
- Antiepileptic drugs: Used to control seizures associated with the infection.
- Surgical intervention: In cases where cysts cause obstructive hydrocephalus.
MRI appearance of Neurocysticercosis
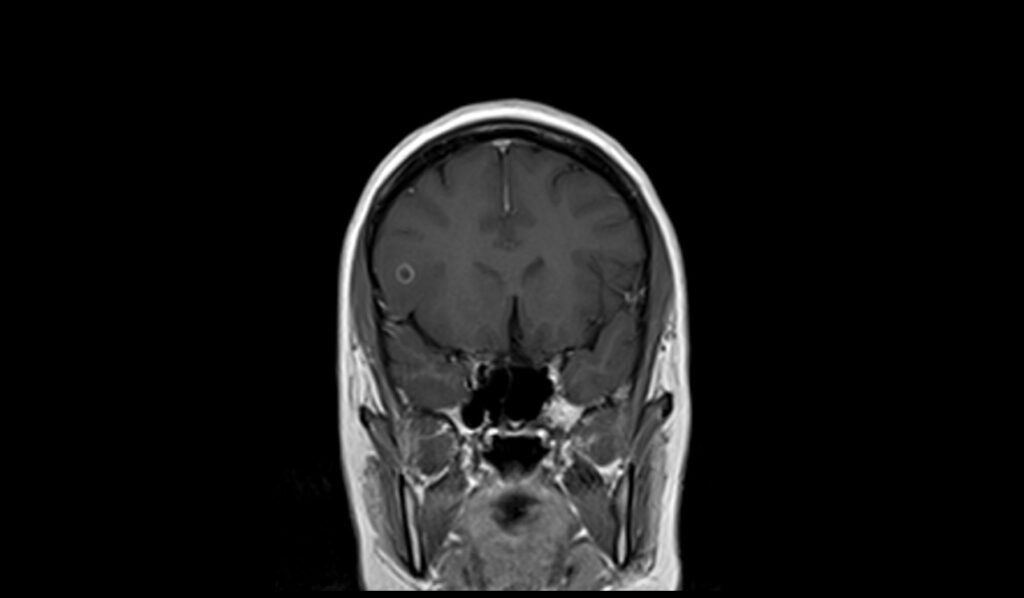
MRI T1 Appearance of Neurocysticercosis
On T1-weighted MRI, neurocysticercosis lesions generally appear as hypointense (dark) cystic areas. The cysts often have a well-defined border with minimal surrounding edema in the viable cyst stage. In the degenerative stages, the cyst fluid may become isointense or hyperintense relative to cerebrospinal fluid (CSF). A characteristic scolex (the head of the tapeworm) may sometimes be visible within the cyst, appearing as a small, hyperintense nodule, which can be a key diagnostic feature. Calcified lesions, representing the end stage of the disease, appear as hypointense foci due to their dense nature.
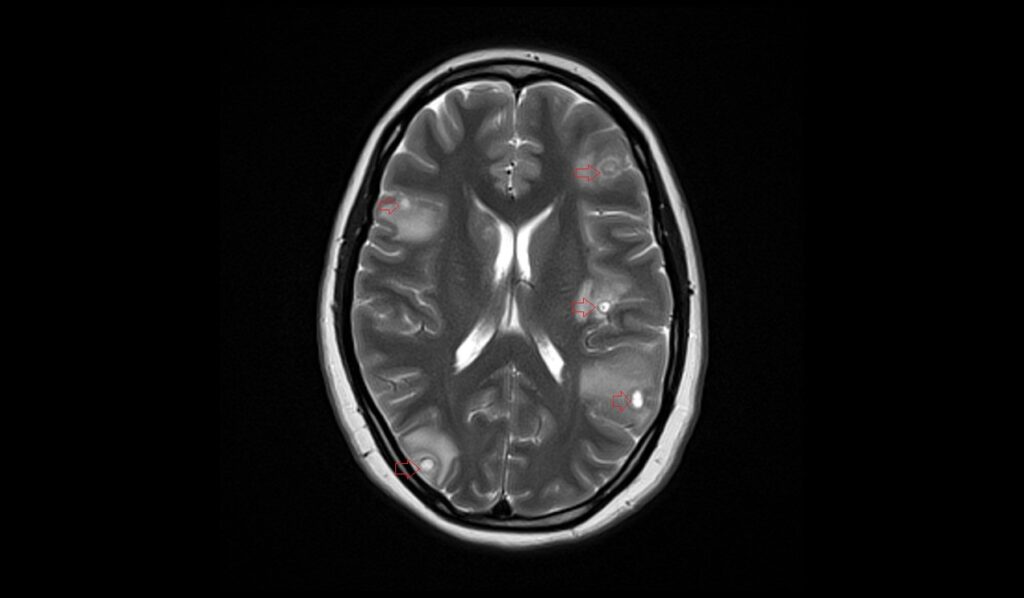
MRI T2 Appearance of Neurocysticercosis
On T2-weighted MRI, neurocysticercosis typically presents as hyperintense (bright) cystic lesions relative to brain parenchyma, with a well-defined border. The surrounding brain tissue may show varying degrees of hyperintense signal if there is associated edema or gliosis. The cyst fluid is often similar in intensity to CSF. The scolex, if present, may appear as a hypointense nodule within the cyst. In the chronic stage, calcified granulomas appear as hypointense foci, which are more easily detected on T2-weighted sequences compared to T1.
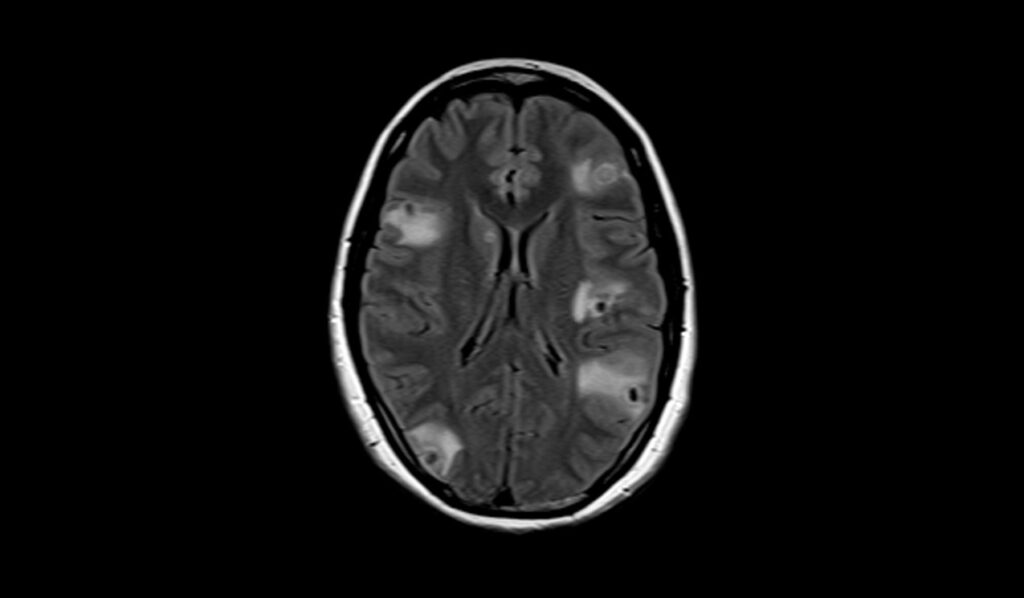
MRI FLAIR Appearance of Neurocysticercosis
On FLAIR (Fluid-Attenuated Inversion Recovery) MRI sequences, neurocysticercosis exhibits unique characteristics where the central fluid part of the cyst is suppressed and appears dark. This suppression helps differentiate the cystic fluid from the surrounding brain tissue and edema, which remain hyperintense. The cyst wall may still be visible as a hyperintense rim, and the scolex, if present, may also appear slightly hyperintense against the suppressed fluid background.
MRI DWI b0, b1000 and ADC Appearance of Neurocysticercosis
On Diffusion-Weighted Imaging (DWI) with b0 and b1000 values, neurocysticercosis cysts usually show no significant restriction of diffusion, appearing hypointense on DWI and hyperintense on the Apparent Diffusion Coefficient (ADC) maps. This lack of diffusion restriction helps differentiate viable cysts from other types of brain lesions that might restrict diffusion, such as abscesses or some tumors. In the vesicular stage, the cyst content resembles CSF, showing facilitated diffusion. However, in the granular nodular stage, some restricted diffusion might be observed due to the inflammatory response and cellular debris within the cyst.
MRI T1 Post-Contrast Appearance of Neurocysticercosis
On T1-weighted post-contrast imaging, neurocysticercosis may exhibit various enhancement patterns depending on the stage of the disease. Viable cysts in the vesicular stage typically do not enhance, except for the scolex, which might show ring enhancement. In the colloidal vesicular stage, cyst walls may enhance due to the breakdown of the blood-brain barrier and surrounding inflammation. Granular nodular cysts often show ring or nodular enhancement, indicating an active inflammatory process. Calcified cysts in the nodular calcified stage generally do not enhance with contrast. The post-contrast T1 sequence is crucial for assessing the integrity of the blood-brain barrier and the degree of inflammatory response.
T2 axial images shows Neurocysticercosis of brain


FLAIR axial images shows Neurocysticercosis of brain


T1 coronal images shows Neurocysticercosis of brain



T2 sagittal image shows Neurocysticercosis of brain


DWI b0 image shows Neurocysticercosis of brain

DWI b1000 image shows Neurocysticercosis of brain

DWI ADC map image shows Neurocysticercosis of brain

T1 coronal post contrast images shows Neurocysticercosis of brain


T1 axial post contrast image shows Neurocysticercosis of brain



References
- Dewi, D. K., Surjadi, K., & Fitrah, A. (2023). Radiology findings in neurocysticercosis: A case report. Radiology Case Reports, 18(9), 2960–2965.
- Kimura-Hayama, E. T., Higuera, J. A., Corona-Cedillo, R., Chávez-Macías, L., Perochena, A., Quiroz-Rojas, L. Y., Rodríguez-Carbajal, J., & Criales, J. L. (2010). Neurocysticercosis: Radiologic-pathologic correlation. RadioGraphics, 30(6).
- Singhi, P. (2011). Neurocysticercosis. Therapeutic Advances in Neurological Disorders, 4(2), 67-81. https://doi.org/10.1177/1756285610395654
- Zhao, J.-L., Lerner, A., Shu, Z., Gao, X.-J., & Zee, C.-S. (2015). Imaging spectrum of neurocysticercosis. Radiology of Infectious Diseases, 1(2), 94-102. https://doi.org/10.1016/j.jrid.2014.12.001
- Venkat, B., Aggarwal, N., Makhaik, S., & Sood, R. (2016). A comprehensive review of imaging findings in human cysticercosis. Japanese Journal of Radiology, 34, 241–257.


