MRI fistula associated mucinous adenocarcinoma
Fistula-associated mucinous adenocarcinoma represents a rare but serious form of cancer emerging in the presence of a long-standing, chronic fistula. Fistulas are abnormal passages that develop between two organs or between an organ and the external body surface. Often seen in areas like the anorectal region, these fistulas are particularly prevalent in patients with inflammatory bowel diseases, such as Crohn’s disease.
The persistent irritation and inflammation triggered by the fistula create an environment conducive to the transformation of normal cells into malignant ones. The hallmark of mucinous adenocarcinoma is the production of mucus by cancerous cells. This cancer type is known for its aggressive nature and the complexity it presents in treatment, largely due to the intricate and challenging environment fostered by the existing fistula. The management of such cancer demands a comprehensive approach, often involving a combination of surgical intervention, chemotherapy, and radiation therapy, tailored to the specific case and the cancer’s stage and location.
Causes:
The development of a fistula-associated mucinous adenocarcinoma is often linked to chronic inflammation. The specific causes can vary but may include:
- Chronic Inflammatory Conditions: Long-standing inflammatory conditions, such as Crohn’s disease or ulcerative colitis, can lead to fistula formation and may increase the risk of developing this type of cancer.
- Infection: Chronic or recurring infections in an area may contribute to fistula formation and subsequent malignant transformation.
- Surgical Complications: In some cases, fistulas may form as a complication of surgery, and if they persist for a long time, they might lead to the development of a mucinous adenocarcinoma.
Symptoms:
The symptoms of fistula-associated mucinous adenocarcinoma can vary depending on the location and size of the tumor, but may include:
- Abnormal Discharge: This might be observed at the fistula site.
- Pain or Discomfort: In the area where the fistula and tumor are located.
- Changes in Bowel Habits or Urinary Symptoms: If the fistula and tumor involve the intestines or bladder.
- Bleeding: Unusual bleeding from the fistula.
- Infection Symptoms: Such as fever, if the area becomes infected.
- General Cancer Symptoms: Like unexplained weight loss, fatigue, and loss of appetite.
Diagnosis:
Accurate diagnosis often involves a combination of imaging studies (like CT scans or MRI), endoscopic evaluations, and biopsy to confirm the type of cancer and determine its extent.
Treatment:
Treatment depends on several factors, including the cancer’s stage, location, and the patient’s overall health:
- Surgical Resection: The primary treatment is usually surgical removal of the tumor and surrounding tissue, including the fistula tract.
- Radiation Therapy: This may be used pre- or post-surgery to shrink the tumor or kill any remaining cancer cells.
- Chemotherapy: Can be administered in conjunction with surgery and radiation, especially in advanced cases or when the tumor is not completely resectable.
MRI Appearance of Mucinous Adenocarcinoma
T1-Weighted MRI:
- On T1-weighted images, mucinous adenocarcinomas typically appear as lesions with low to intermediate signal intensity. The mucin component of the tumor often shows up as more hyperintense compared to the surrounding muscle or fat.
T2-Weighted MRI:
- In T2-weighted images, these tumors generally have high signal intensity due to the high water content in mucin. This contrast can help in delineating the tumor from the surrounding tissues.
Short Tau Inversion Recovery (STIR) or T2 Fat Saturation:
- Both STIR and T2 fat sat techniques are used to suppress fat signal, making it easier to see edema, inflammation, or tumors. In these sequences, the mucinous adenocarcinoma associated with a fistula may demonstrate high signal intensity, similar to T2WI, but with better contrast against the suppressed fat signal.
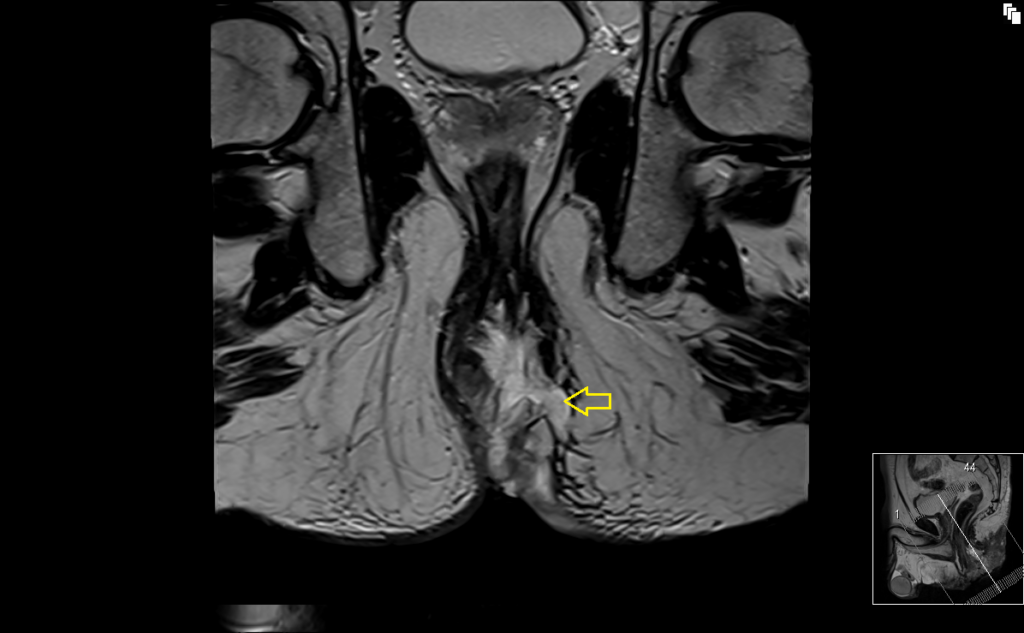
T2 TSE sagittal image shows fistula associated mucinous adenocarcinoma

T2 coronal oblique image shows fistula associated mucinous adenocarcinoma
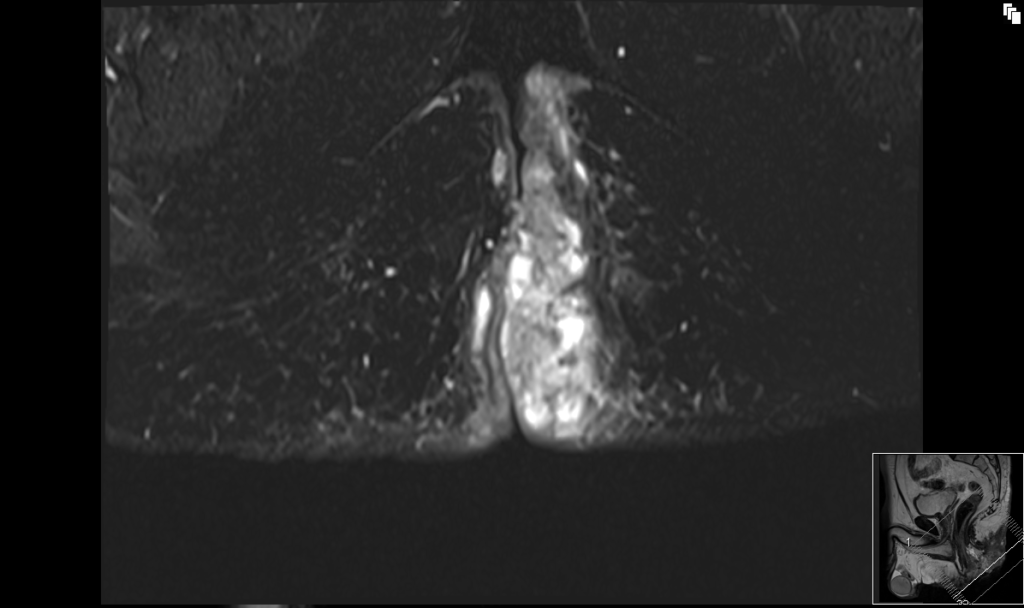
T2 axial oblique image shows fistula associated mucinous adenocarcinoma

T2 fat saturated axial oblique image shows fistula associated mucinous adenocarcinoma
References
- Hama, Y., Makita, K., Yamana, T., & Dodanuki, K. (2006, August). Mucinous Adenocarcinoma Arising from Fistula in Ano: MRI Findings. American Journal of Roentgenology, 187(2). https://doi.org/10.2214/AJR.05.0011
- Tahir, M., Rahman, J., Zubair, T., & Basit, A. (2020). An Association of Mucinous Adenocarcinoma With Chronic Peri-Anal Fistula: A Brief Review of Pathophysiology of Rare Tumor. Cureus, 12(6), e8882. https://doi.org/10.7759/cureus.8882
- Zhu X, Zhu TS, Ye DD, Liu SW. Magnetic resonance imaging findings of carcinoma arising from anal fistula: A retrospective study in a single institution. World J Clin Cases. 2020 Nov 6;8(21):5159-5171. doi: 10.12998/wjcc.v8.i21.5159. Published online Nov 6, 2020. PMID: 33269252.
- Koizumi, M., Matsuda, A., Yamada, T., Morimoto, K., Kubota, I., Kubota, Y., Tamura, S., Tominaga, K., Sakatani, T., & Yoshida, H. (2023). A case report of anal fistula-associated mucinous adenocarcinoma developing 3 years after treatment of perianal abscess. Surgical Case Reports, 9(159), 11 September 2023.


