MRI Spinal Metastases
Spinal metastases are cancerous tumors that have spread to the spine from another part of the body. This spread of cancer cells is known as metastasis. The spine is a common site for metastases because the vertebral column’s venous system, known as Batson’s plexus, provides an easy pathway for cancer cells to travel from other parts of the body.
Causes
The primary cause of spinal metastases is the presence of a primary cancer elsewhere in the body that has the capability to spread. Common cancers that may lead to spinal metastases include:
- Breast cancer
- Prostate cancer
- Lung cancer
- Kidney cancer
- Thyroid cancer
Symptoms
Symptoms of spinal metastases can vary depending on the location and size of the tumors, but typically include:
- Pain in the back or neck, which may be worse at night or upon waking
- Numbness or weakness, often in the limbs, depending on where the spine is affected
- Difficulty walking or loss of function of the limbs due to nerve compression
- Loss of bladder or bowel control in severe cases
- Paralysis: Severe cases can lead to loss of motor function.
- Pathological fractures: Weakened bones can lead to fractures even with minimal trauma.
Diagnosis
Diagnosis involves a combination of clinical evaluation and imaging studies:
- Medical history and physical examination: Assessment of symptoms and neurological function.
- Imaging studies:
- X-rays: Initial evaluation but may not detect early metastases.
- MRI (Magnetic Resonance Imaging): The preferred method for detailed images of spinal cord and surrounding tissues.
- CT (Computed Tomography) scans: Useful for assessing bone involvement.
- Bone scans: Detects areas of increased bone activity.
- Biopsy: To confirm the type of cancer, if the primary source is unknown.
Treatment
Treatment aims to relieve symptoms, preserve neurological function, and stabilize the spine. It often involves a multidisciplinary approach:
- Radiation therapy: Commonly used to shrink tumors and relieve pain.
- Surgery: May be necessary to remove the tumor, stabilize the spine, or decompress the spinal cord.
- Medications:
- Pain relievers: To manage pain.
- Steroids: To reduce inflammation and swelling around the spinal cord.
- Bisphosphonates: To strengthen bones and reduce fracture risk.
- Chemotherapy: Systemic treatment to target cancer cells throughout the body.
- Targeted therapy and immunotherapy: Depending on the type of primary cancer and its specific characteristics.
MRI Appearance of Spinal Metastases
T1 Appearance of Spinal Metastases
On T1-weighted MRI sequences, spinal metastases typically appear as areas of low signal intensity compared to the normal high signal intensity of the fatty bone marrow. This signal decrease is due to the replacement of fatty marrow by tumor cells, which contain more water and less fat. The metastatic lesions often appear as hypointense (dark) spots within the vertebral bodies, and the extent of these lesions can vary from focal areas to diffuse involvement. T1 imaging is particularly useful for detecting changes in the bone marrow composition and for delineating the anatomical details of the spine.
T2 Appearance of Spinal Metastases
In T2-weighted MRI sequences, spinal metastases usually exhibit high signal intensity relative to the normal bone marrow. This hyperintense (bright) signal is attributed to the increased water content within the metastatic lesions, resulting from the presence of tumor cells, edema, and potential inflammatory response. T2 imaging is effective in highlighting the lesions against the background of normal spinal structures and is instrumental in identifying the extent of metastatic disease, including any involvement of the spinal canal, paraspinal tissues, and intervertebral discs.
STIR Appearance of Spinal Metastases
Short Tau Inversion Recovery (STIR) sequences in MRI are highly sensitive for detecting spinal metastases due to their ability to suppress the signal from fat, making the lesions stand out more clearly. On STIR images, spinal metastases typically appear as areas of high signal intensity against a dark background of suppressed fatty bone marrow. This sequence is particularly useful in identifying small lesions, detecting marrow edema, and evaluating the extent of metastatic involvement. STIR is an essential tool for the comprehensive assessment of metastatic disease in the spine, providing high contrast between normal and pathological tissues.
T2 sagittal image of lumbar spine shows spinal metastases

STIR sagittal image of lumbar spine shows spinal metastases

T1 TSE sagittal image of lumbar spine shows CSF Leak

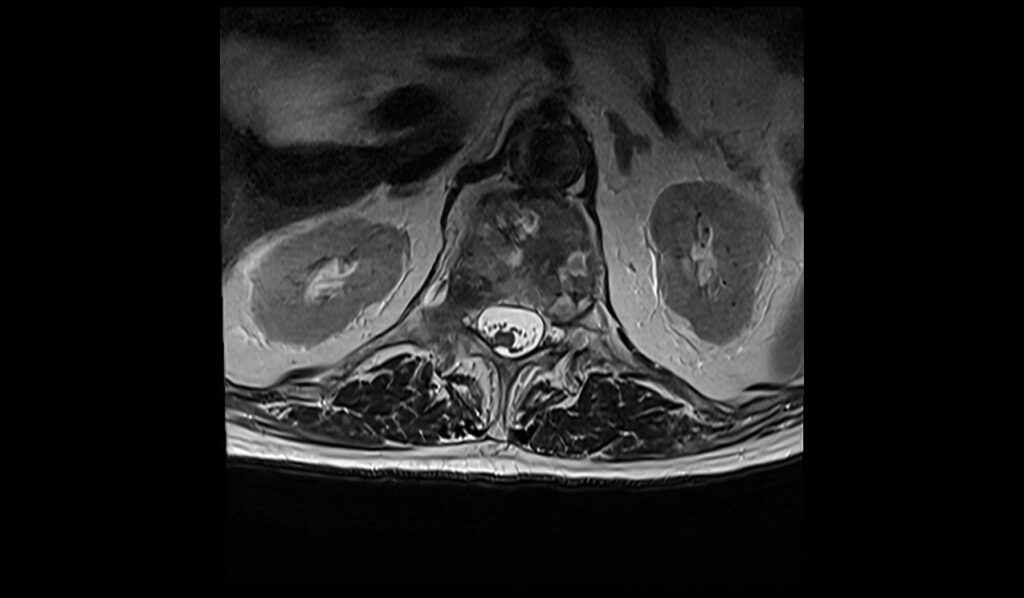
T2 TSE axial image of lumbar spine shows spinal metastases

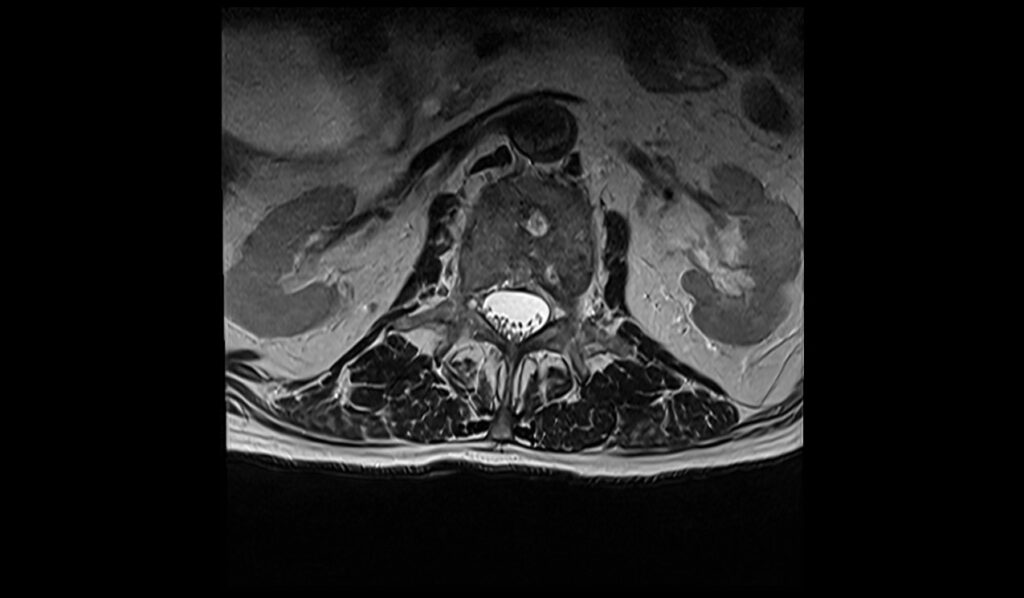
T1 TSE axial image of lumbar spine shows spinal metastases



References
- Jasmin, J. O., & Schiff, D. (2014). Metastatic disease and the nervous system. In M. J. Aminoff, F. Boller, & D. S. Swaab (Eds.), Aminoff’s Neurology and General Medicine (5th ed., pp. 539-562). Academic Press. https://doi.org/10.1016/B978-0-12-407710-2.00026-6
- Mossa-Basha, M., Gerszten, P. C., Myrehaug, S., Mayr, N. A., Yuh, W. T. C., Maralani, P. J., Sahgal, A., & Lo, S. S. (2019). Spinal metastasis: Diagnosis, management and follow-up. British Journal of Radiology, 92(1103), 20190211. https://doi.org/10.1259/bjr.20190211
- Shah, L. M., & Salzman, K. L. (2011). Imaging of spinal metastatic disease. International Journal of Surgical Oncology, 2011, Article 769753. https://doi.org/10.1155/2011/769753
- Park, S., & Musculoskeletal Imaging Laboratory, Ajou University Medical Center. (2021). Differentiation of vertebral metastases from focal hematopoietic marrow depositions on MRI: Added value of proton density fat fraction. AJR American Journal of Roentgenology, 216(3), 734–741.


