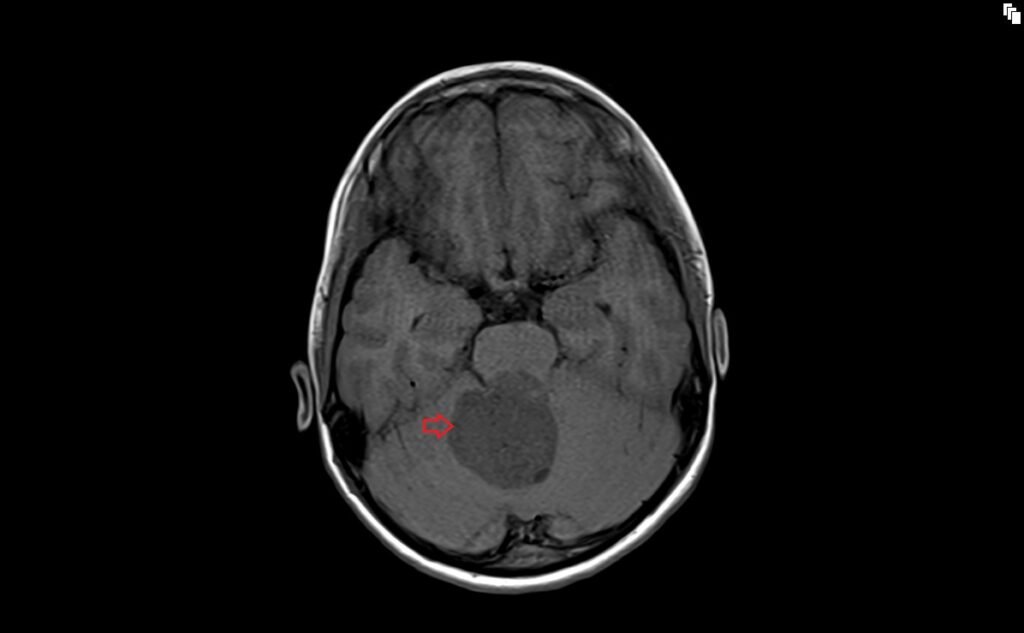
MRI Medulloblastoma
Medulloblastoma is a type of brain tumor primarily affecting children, though it can also occur in adults. It is considered the most common malignant brain tumor in children. Medulloblastomas originate in the cerebellum or posterior fossa region of the brain, an area responsible for coordinating movement.
Causes
The exact cause of medulloblastoma is not fully understood. However, it is believed to involve genetic mutations, some of which may be inherited, although this is rare. Other cases seem to arise sporadically without a known cause.
Symptoms
Symptoms of medulloblastoma are generally related to increased intracranial pressure or disruption of cerebellar functions and can include:
- Headaches, often worse in the morning.
- Nausea and Vomiting, particularly in the morning.
- Problems with Coordination and Balance.
- Gait Disturbances: Difficulty in walking or a tendency to fall.
- Behavioral or Cognitive Changes: Changes in personality or school performance.
- Eye Problems: Double vision or other vision abnormalities.
- Increased Head Size in infants (due to open skull sutures).
Diagnosis
Diagnosis involves a combination of:
- Neurological Exam: To check vision, hearing, balance, coordination, strength, and reflexes.
- Imaging : MRI (most common), CT scans to visualize the tumor.
- Lumbar Puncture (Spinal Tap): To check for cancer cells in the cerebrospinal fluid.
- Biopsy: To confirm the diagnosis and classify the tumor subtype.
Treatment
Treatment for medulloblastoma is multi-modal and may include:
- Surgery: To remove as much of the tumor as safely possible.
- Radiation Therapy: Postoperative radiation is a standard treatment, especially for children over the age of 3. For younger children, strategies to delay or reduce radiation are considered due to long-term effects on the developing brain.
- Chemotherapy: Often used in conjunction with radiation therapy to increase treatment effectiveness.
MRI appearance of Medulloblastoma
T1-Weighted MRI: Medulloblastomas often appear as hypointense or isointense (darker or similar in intensity) to the surrounding brain tissue on T1-weighted images.
T2-Weighted MRI: On T2-weighted images, these tumors usually present as hyperintense (brighter) compared to the surrounding brain tissue.
FLAIR (Fluid-Attenuated Inversion Recovery): In FLAIR sequences, medulloblastomas generally show a hyperintense signal, similar to T2-weighted images, but with better suppression of signals from cerebrospinal fluid, which can help in delineating the tumor more clearly.
DWI (Diffusion-Weighted Imaging): Medulloblastomas typically appear hyperintense on DWI. This sequence is helpful in assessing the cellular density of the tumor, as high cellularity often restricts the diffusion of water molecules, leading to a brighter appearance on these images.
Post-Contrast T1: After the administration of contrast material (usually gadolinium), medulloblastomas often show strong and homogeneous enhancement on T1-weighted images. This enhancement can help to differentiate the tumor from surrounding structures and can also be useful in evaluating the effectiveness of treatment.
T2 axial image shows Medulloblastoma

FLAIR coronal image shows Medulloblastoma

T1 axial image shows Medulloblastoma
T2 sagittal image shows Medulloblastoma

T1 post contrast axial image shows Medulloblastoma

T1 post contrast coronal image shows Medulloblastoma

T1 post contrast sagittal image shows Medulloblastoma

References
- Zhang, M., Wong, S. W., Wright, J. N., Wagner, M. W., Toescu, S., Han, M., Tam, L. T., Zhou, Q., Ahmadian, S. S., Shpanskaya, K., Lummus, S., Lai, H., Eghbal, A., Radmanesh, A., Nemelka, J., et al. (2022). MRI Radiogenomics of Pediatric Medulloblastoma: A Multicenter Study. Radiology, 304(2), Article ID 212137. https://doi.org/10.1148/radiol.212137
Colafati, G. S., Voicu, I. P., Carducci, C., Miele, E., Carai, A., Di Loreto, S., Marrazzo, A., Cacchione, A., Cecinati, V., Tornesello, A., & Mastronuzzi, A. (2018). MRI features as a helpful tool to predict the molecular subgroups of medulloblastoma: state of the art. Ther Adv Neurol Disord, 11, 1756286418775375.
Yeom, K. W., Mobley, B. C., Lober, R. M., Andre, J. B., Partap, S., Vogel, H., & Barnes, P. D. (2013). Distinctive MRI Features of Pediatric Medulloblastoma Subtypes. Pediatric Imaging, Original Research, AJR, 200, 895–903. doi:10.2214/AJR.12.8873
- Al-Sharydah, A.M., Al-Abdulwahhab, A.H., Al-Suhibani, S.S., Al-Issawi, W.M., Al-Zahrani, F., Katbi, F.A., Al-Thuneyyan, M.A., Jallul, T., & Alabbas, F.M. (2021). Posterior fossa extra-axial variations of medulloblastoma: a pictorial review as a primer for radiologists. Insights into Imaging, 12(43), 1-2.


