Liver hemangioma
A liver hemangioma, medically referred to as hepatic hemangioma, is a prevalent non-cancerous vascular lesion or tumor that typically develops within the liver. These lesions are frequently encountered in medical practice and are usually discovered incidentally during various medical imaging studies, such as ultrasound, computed tomography (CT) scans, or magnetic resonance imaging (MRI) scans. Importantly, these imaging procedures are often conducted for entirely unrelated medical reasons.
One distinctive feature of liver hemangiomas is their tendency to remain asymptomatic, which means they do not typically cause noticeable symptoms or health problems in individuals who have them. As a result, many people may go about their lives without any awareness of the presence of these benign liver masses.
- Appearance: Liver hemangiomas are composed of a cluster of blood vessels. They can vary in size, ranging from small, less than an inch in diameter, to quite large, several inches across. These lesions are typically well-defined and appear as dark, round or oval masses within the liver tissue.
- Blood Vessel Origin: Liver hemangiomas originate from the liver’s blood vessels, particularly the hepatic artery. They consist of a tangle of blood vessels with thin walls and are filled with blood. These vessels are often dilated and may not function normally.
- Symptoms (if Present): While most liver hemangiomas are asymptomatic, some individuals with larger hemangiomas may experience discomfort or pain in the upper right abdomen. In extremely rare cases, particularly if the hemangioma ruptures or causes complications, more severe symptoms such as bleeding or liver dysfunction can occur.
- Diagnosis: Diagnosis of liver hemangioma is typically made through imaging studies, as the lesions have characteristic features on imaging. These features include a well-defined outline and a pattern known as “flash-filling,” where the contrast material rapidly fills the lesion during imaging tests.
- Natural History: Liver hemangiomas are generally stable lesions and tend not to grow significantly over time. They do not carry a risk of becoming cancerous (malignant) and are not associated with a higher risk of liver cancer.
- Treatment: In most cases, liver hemangiomas do not require treatment, especially if they are small, asymptomatic, and stable. However, if a hemangioma is causing symptoms, growing rapidly, or causing complications, treatment options such as surgical removal or minimally invasive procedures may be considered.
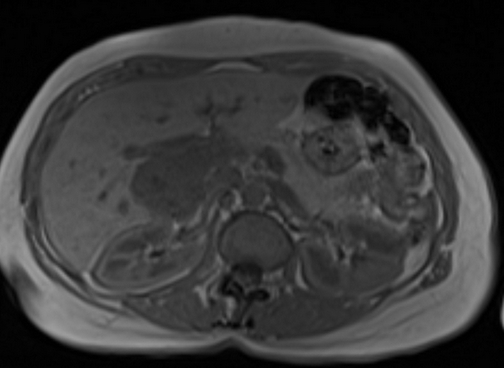
MRI appearance
The MRI appearance of liver hemangiomas can vary depending on several factors, including their size and vascular characteristics. Here is a general description of how liver hemangiomas appears on different MRI sequences:
T1-Weighted Imaging (T1WI): Liver hemangiomas typically appear hypointense (darker) on T1-weighted MRI scans. They are darker than the surrounding liver tissue due to their vascular composition.
T2-Weighted Imaging (T2WI): On T2-weighted MRI scans, liver hemangiomas often appear hyperintense (brighter) compared to the surrounding liver tissue. The increased signal intensity is due to the blood-filled vascular spaces within the lesion.
In-Phase and Out-of-Phase Imaging: In-phase and out-of-phase imaging are used to assess the presence of fat within lesions. Liver hemangiomas do not contain fat, so they typically appear similar in both in-phase and out-of-phase images, showing no significant signal drop on out-of-phase images.
Diffusion-Weighted Imaging (DWI): Liver hemangiomas can demonstrate variable signal intensity on DWI. The signal characteristics may vary depending on factors such as lesion vascularity and size. Typically, they exhibit mild to moderate restriction of water diffusion.
T1-Weighted Post-Contrast Imaging (T1-CE or T1WI with contrast): After the administration of a contrast agent (such as gadolinium), liver hemangiomas often show characteristic enhancement patterns. In the arterial phase, they usually demonstrate peripheral and centripetal enhancement, which means the outer rim of the lesion enhances first and then the contrast progresses toward the center. This appearance is often referred to as a “progressive fill-in” pattern. In the portal venous and delayed phases, the entire lesion becomes hyperintense.

T2 fat saturated Axial

T2 Axial TE 90

T2 Axial TE 180
T1 IN PHASE
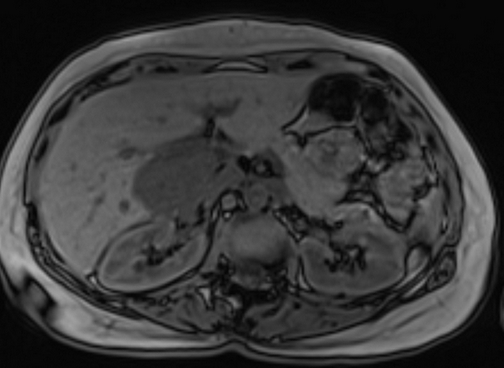
T1 out of phase

T1 pre contrast

T1 post contrast arterial phase

T1 post contrast venous phase

T1 post contrast 5 minutes

T1 post contrast 20 minutes
References
Bartolotta, T. V., Taibbi, A., Midiri, M., Lagalla, R., & De Maria, M. (2015). Contrast-enhanced magnetic resonance imaging of the liver: Hepatic lesions. World Journal of Hepatology, 7(21), 2374-2391.
Mortele, K. J., Ros, P. R., Cystic focal liver lesions in the adult: Differential CT and MR imaging features. Radiographics, 21(4), 895-910.
Hussain, S. M., Terkivatan, T., Zondervan, P. E., Lanjouw, E., De Rave, S., & Ijzermans, J. N. (2004). Focal nodular hyperplasia: findings at state-of-the-art MR imaging, US, CT, and pathologic analysis. Radiographics, 24(1), 3-17.
Paltiel, H. J., Burrows, P. E., Kozakewich, H. P., Zurakowski, D., Mulliken, J. B., & Boiselle, P. M. (2004). Soft-tissue vascular anomalies in children: a comparative study of imaging modalities. Pediatric Radiology, 34(4), 262-271.
Tanaka, S., & Hirohashi, K. (2014). Diagnostic imaging: Contrast-enhanced computed tomography and magnetic resonance imaging in hepatocellular carcinoma. World Journal of Gastroenterology, 20(24), 15972-15987.
