Fahr Syndrome (Bilateral Striatopallidodentate Calcinosis) MRI
Fahr syndrome, also known as bilateral striatopallidodentate calcinosis, is a rare, inherited neurological disorder characterized by abnormal calcium deposits in certain areas of the brain. These areas include the basal ganglia, thalamus, dentate nucleus, and cerebral cortex. The condition typically manifests in adults, although it can occur at any age.
Causes
The exact cause of Fahr’s syndrome is not fully understood. In many cases, it appears to be sporadic, but there can also be familial patterns suggesting a genetic component. The condition is often associated with metabolic disorders, particularly those involving disturbances in calcium metabolism. Disorders such as hypoparathyroidism (which leads to low levels of parathyroid hormone and calcium in the body) are frequently linked to the syndrome.
Symptoms
The symptoms of Fahr syndrome can vary widely among individuals and may include:
- Movement disorders: tremors, chorea (involuntary, rapid, and irregular movements), dystonia (muscle contractions causing abnormal postures), and parkinsonism (rigidity, bradykinesia, and tremors).
- Cognitive impairment: dementia, memory loss, confusion, and difficulties with thinking and reasoning.
- Psychiatric symptoms: mood swings, depression, anxiety, psychosis, and personality changes.
- Seizures
- Speech difficulties
- Headaches
- Balance and coordination problems
Diagnosis
Diagnosis of Fahr syndrome involves a combination of clinical evaluation, imaging studies, and laboratory tests. The key diagnostic steps include:
- Clinical Evaluation: Assessment of symptoms and medical history, including any family history of similar symptoms.
- Imaging Studies:
- CT Scan: The most common imaging modality for detecting brain calcifications characteristic of Fahr syndrome.
- MRI: Can be used to assess the extent of calcifications and any associated brain abnormalities.
- Laboratory Tests:
- Blood tests to evaluate calcium and phosphate metabolism, parathyroid hormone levels, and other relevant metabolic parameters.
- Genetic testing may be conducted if a hereditary form of the syndrome is suspected.
Treatment
There is no cure for Fahr syndrome, and treatment is primarily symptomatic and supportive. Management strategies may include:
Medication:
- Antiepileptic drugs: For managing seizures.
- Antipsychotic and antidepressant medications: For psychiatric symptoms.
- Medications for movement disorders: Such as levodopa for parkinsonism and muscle relaxants for dystonia.
Management of Underlying Conditions:
If Fahr syndrome is secondary to an underlying condition (e.g., hypoparathyroidism), treatment of that condition may help manage symptoms.
Supportive Therapies:
- Physical therapy: To improve mobility and coordination.
- Speech therapy: To address speech and swallowing difficulties.
- Occupational therapy: To assist with daily living activities.
Regular Monitoring:
Ongoing follow-up with a neurologist and other specialists to monitor disease progression and adjust treatments as necessary.
MRI appearance of Fahr Syndrome
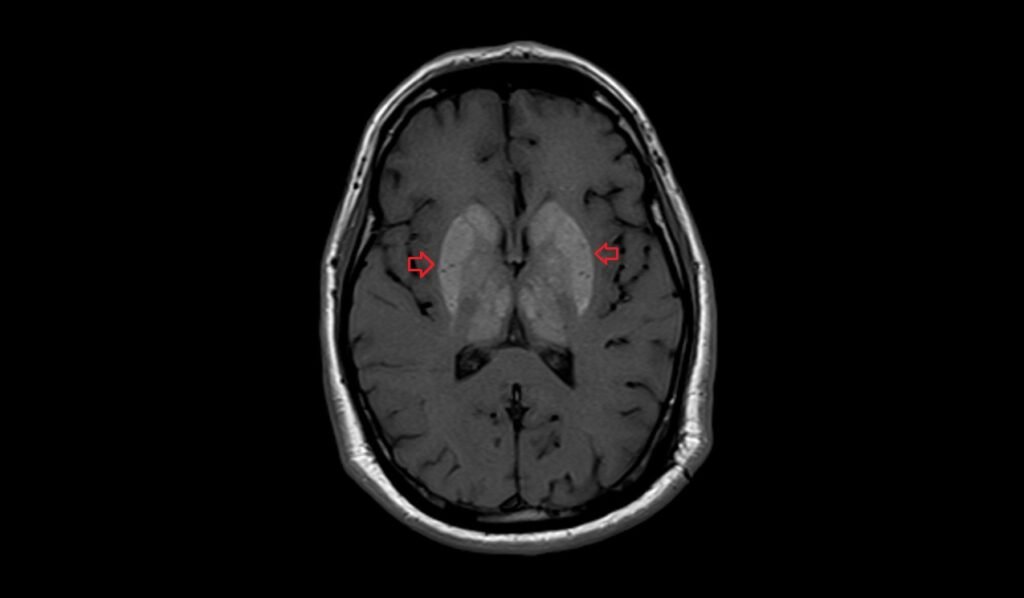
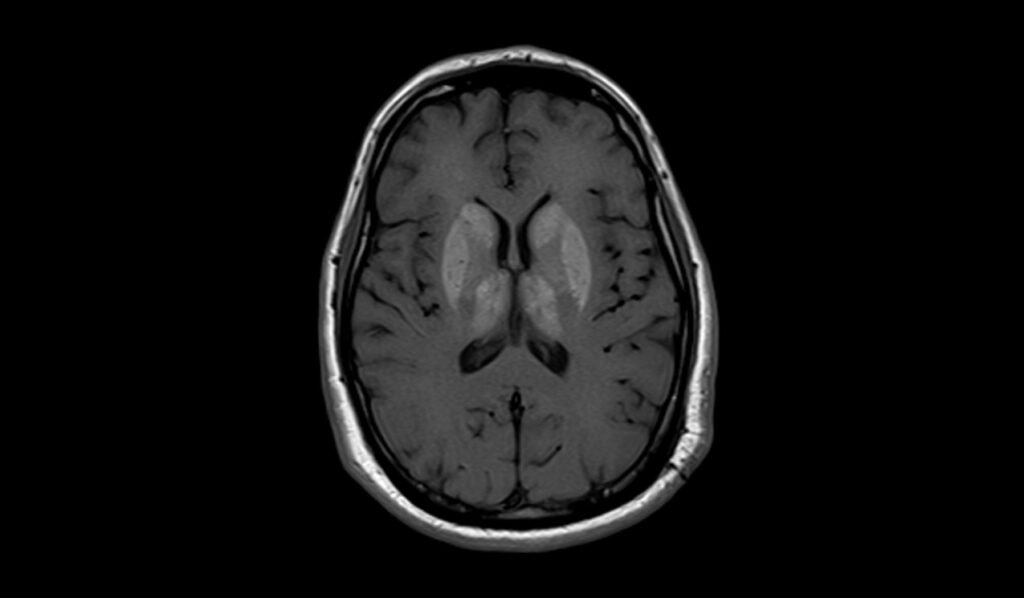
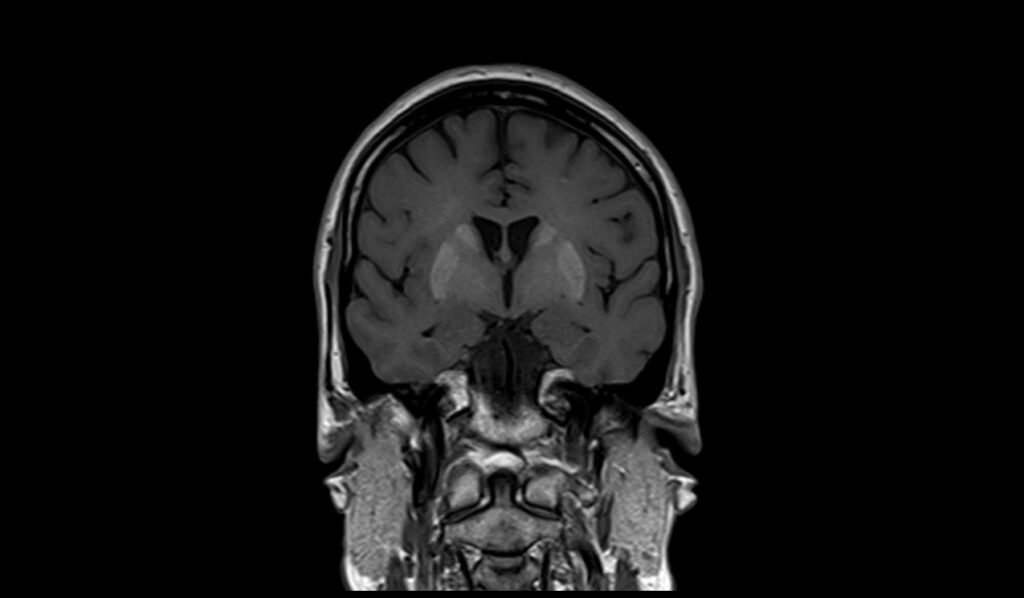
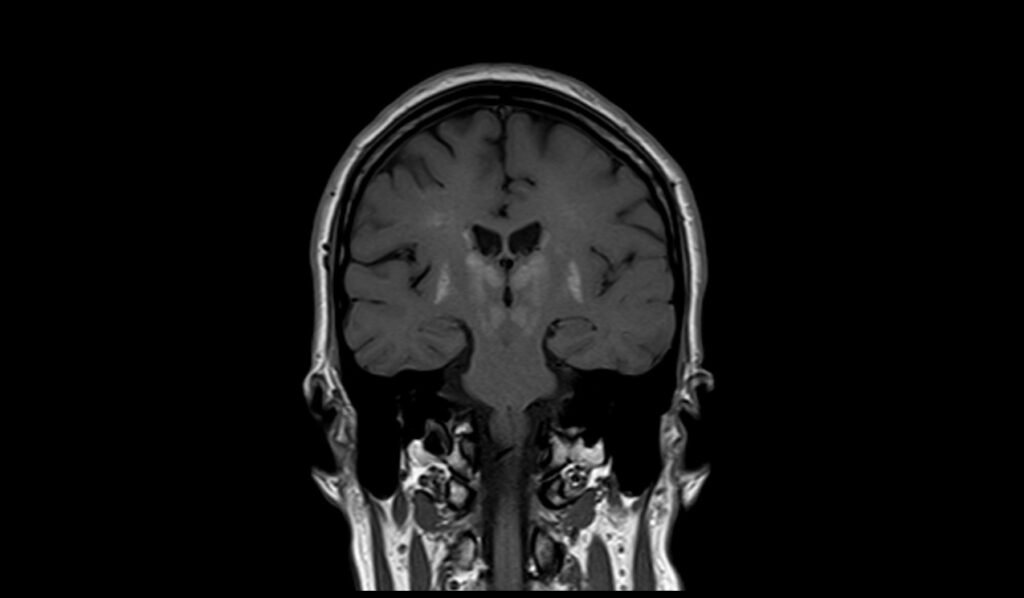
MRI T1 Appearance of Fahr Syndrome
In Fahr syndrome, T1-weighted MRI images typically show hyperintense (bright) signals in areas of abnormal calcification within the brain. These calcifications are commonly located in the basal ganglia, thalamus, dentate nucleus, and subcortical white matter. The hyperintensity on T1-weighted images is due to the presence of calcium, which has a high signal intensity on this sequence. These findings are characteristic of Fahr syndrome and help in differentiating it from other neurodegenerative and metabolic disorders.
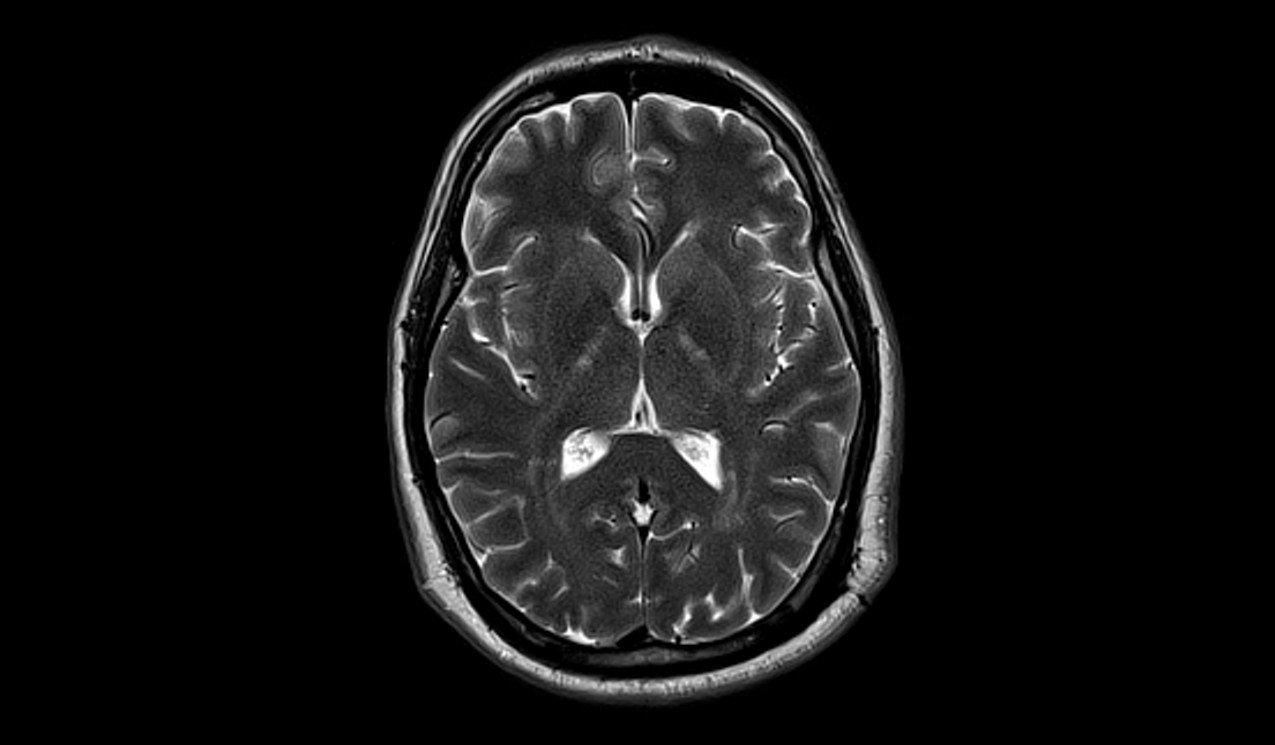
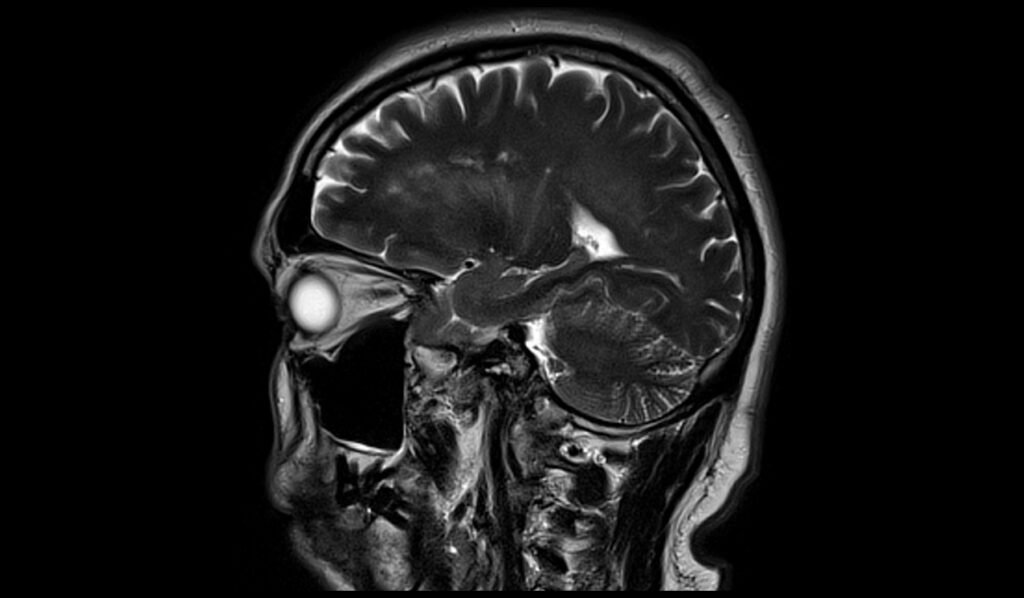
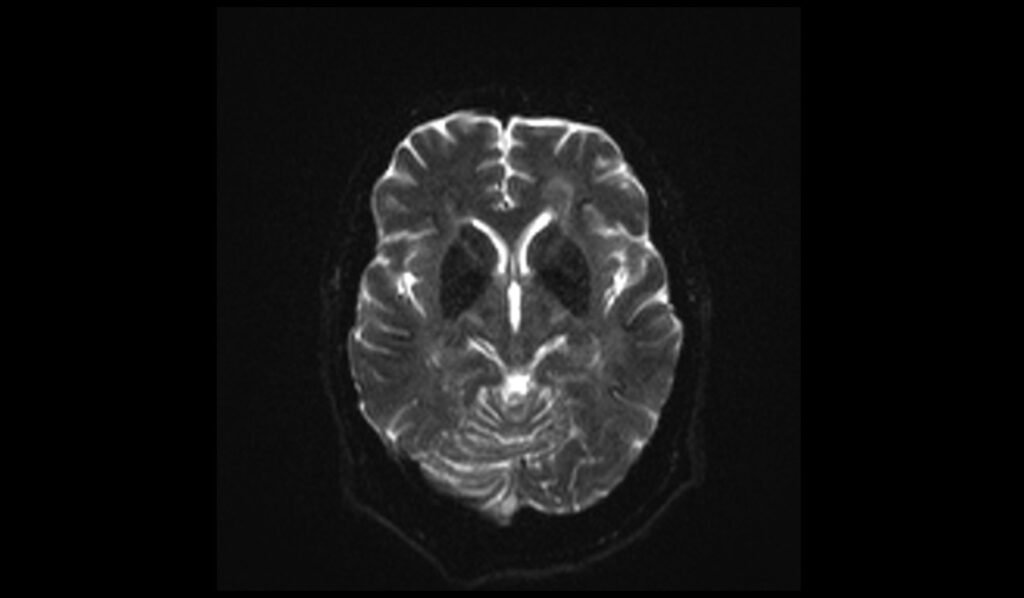
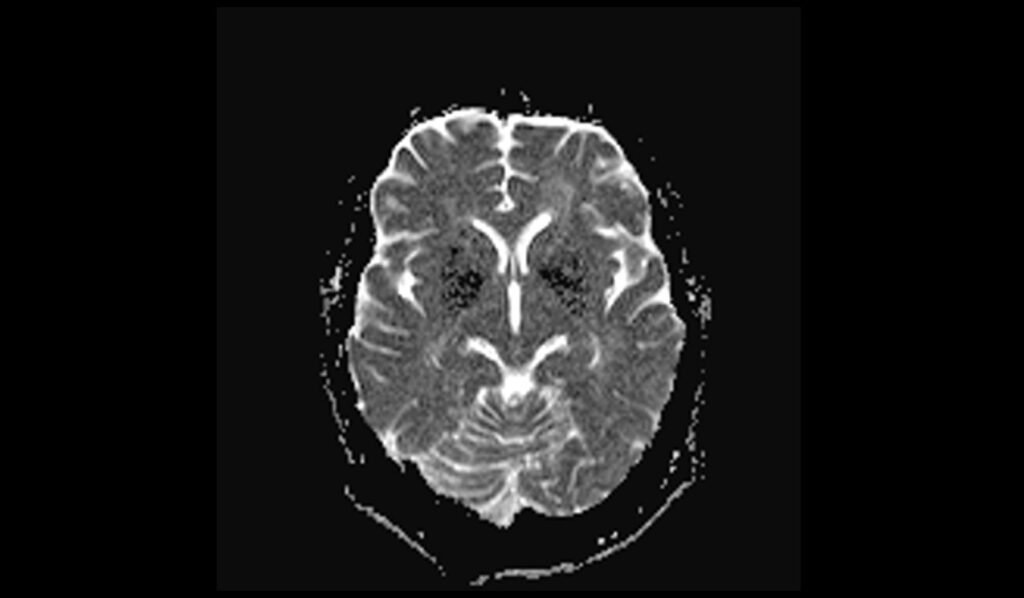
MRI T2 Appearance of Fahr Syndrome
On T2-weighted MRI images, Fahr syndrome appears as hypo- to isointense (dark to intermediate) signals in the same regions where calcifications are present, such as the basal ganglia, thalamus, dentate nucleus, and subcortical white matter. The hypo- to isointensity on T2-weighted images is indicative of the dense, calcified deposits, which do not allow for a high signal return on this sequence. This characteristic appearance aids in the diagnosis and evaluation of the extent of calcification in Fahr syndrome.
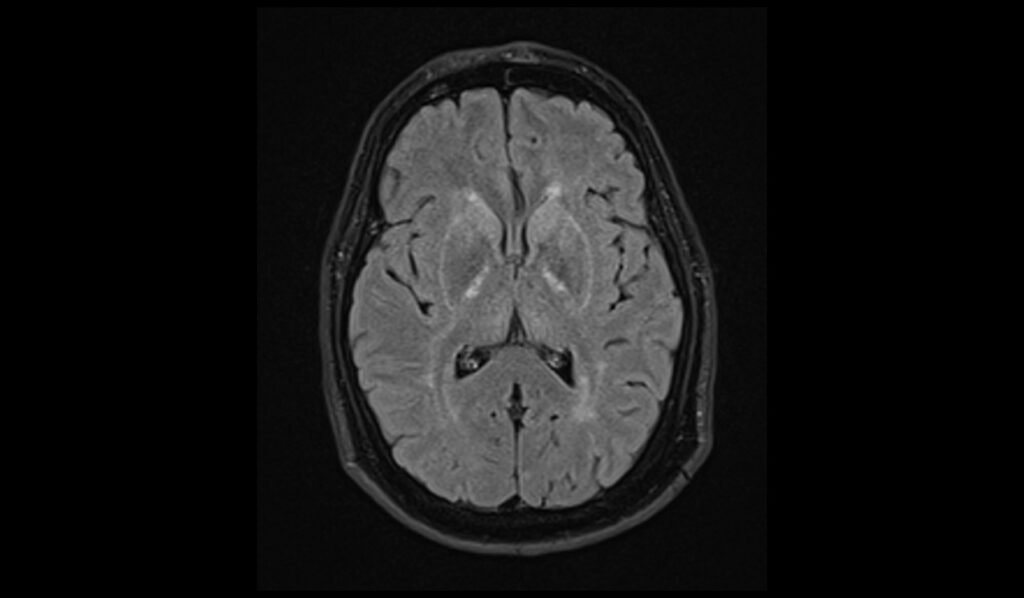
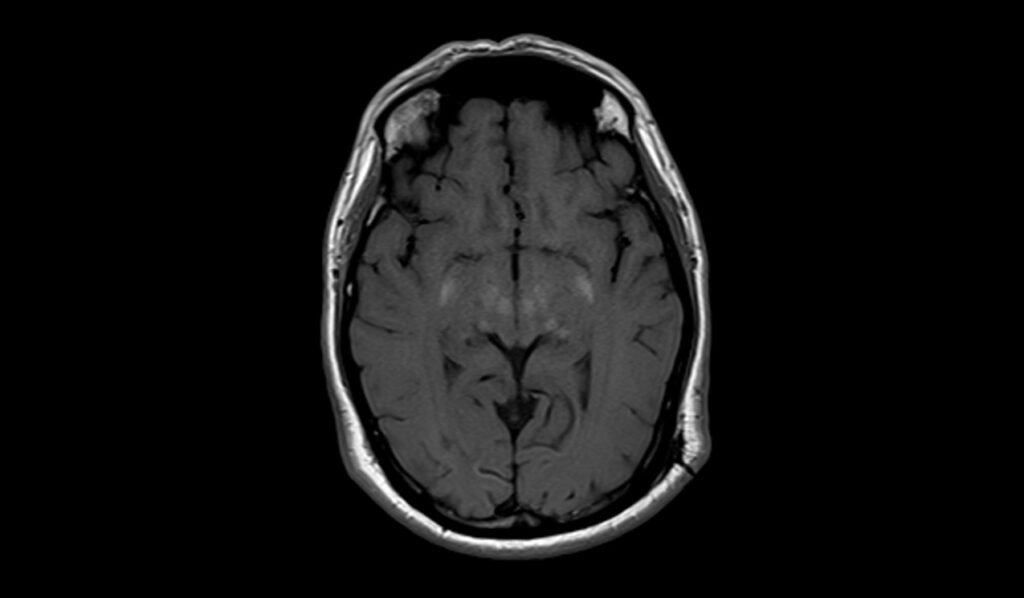
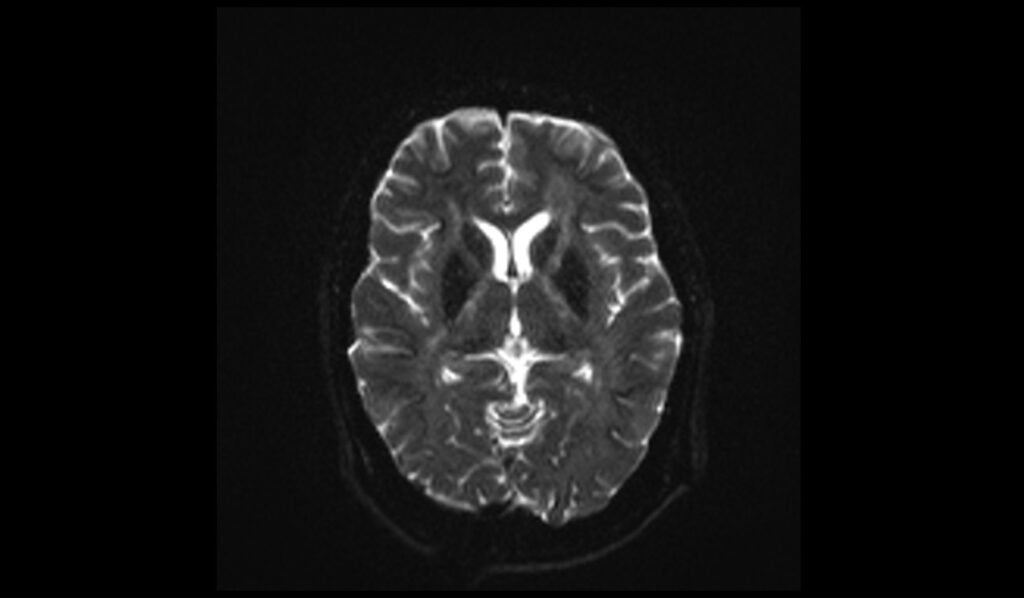
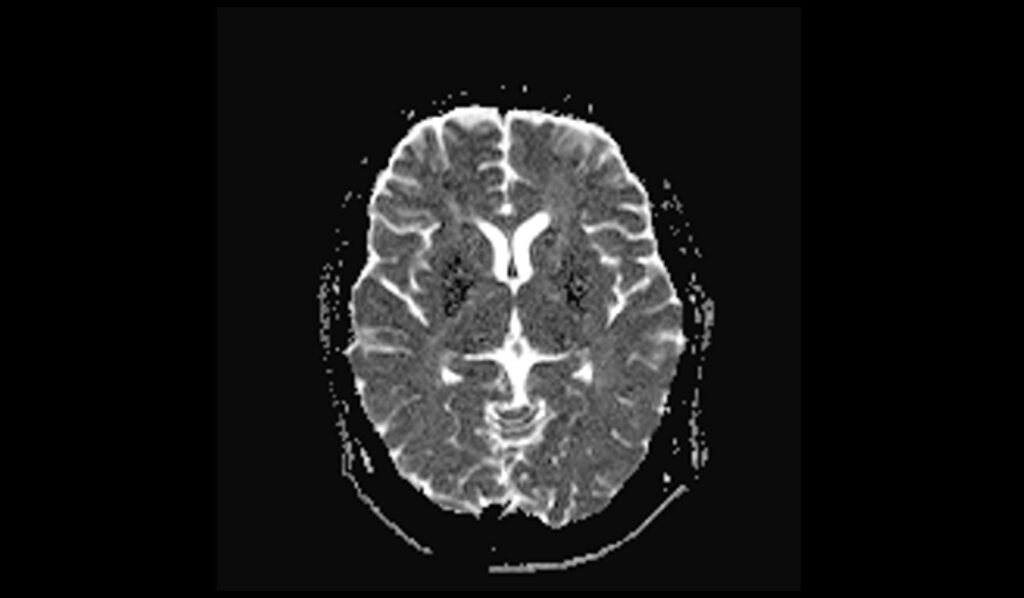
MRI FLAIR Appearance of Fahr Syndrome
In FLAIR (Fluid-Attenuated Inversion Recovery) sequences, Fahr syndrome typically exhibits iso- to hypointense signals in the calcified areas. The suppression of fluid signals in FLAIR imaging accentuates the visibility of pathological changes, but calcifications tend to appear less conspicuous compared to their presentation on T1-weighted images. The iso- to hypointense appearance helps in confirming the presence of calcifications while providing a clearer contrast of the brain’s parenchymal structure.
MRI DWI and ADC Appearance of Fahr Syndrome
Diffusion-weighted imaging (DWI) and apparent diffusion coefficient (ADC) maps in Fahr syndrome usually show no significant abnormalities. The b0 and b1000 DWI images do not typically display diffusion restriction, meaning the calcified areas do not appear hyperintense (bright) on DWI sequences. Similarly, ADC maps do not show reduced diffusion, as the calcifications do not affect the water diffusion properties of the brain tissue in a manner that would be detected by these sequences. This normal appearance on DWI and ADC can help differentiate Fahr syndrome from other conditions that might cause diffusion abnormalities.
T2 axial image shows Fahr Syndrome
FLAIR axial image shows Fahr Syndrome
T1 axial images shows Fahr Syndrome
T1 coronal images shows Fahr Syndrome
T2 sagittal images shows Fahr Syndrome
DWI b0 images shows Fahr Syndrome
DWI b500 images shows Fahr Syndrome
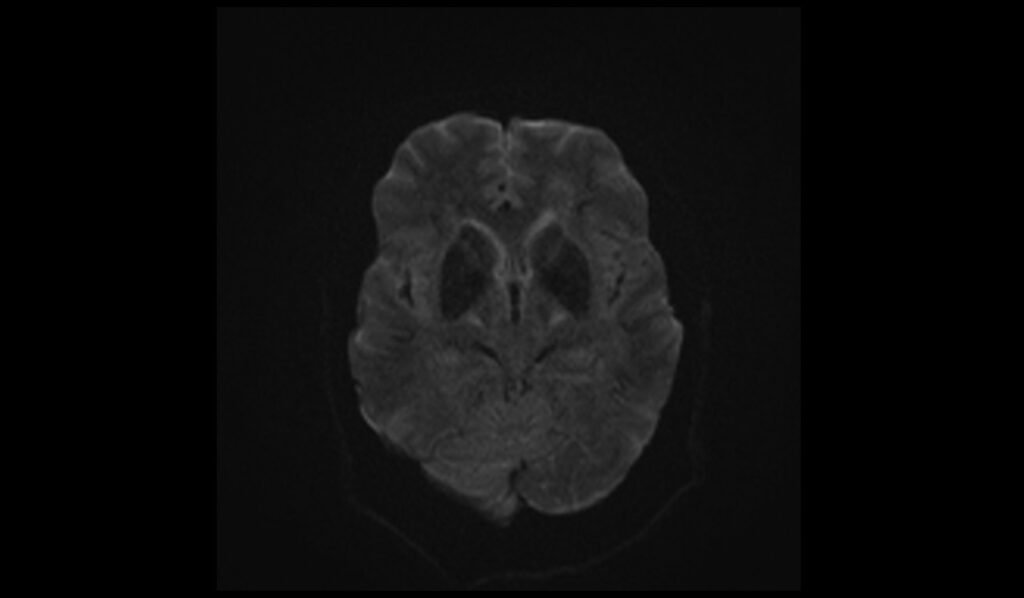
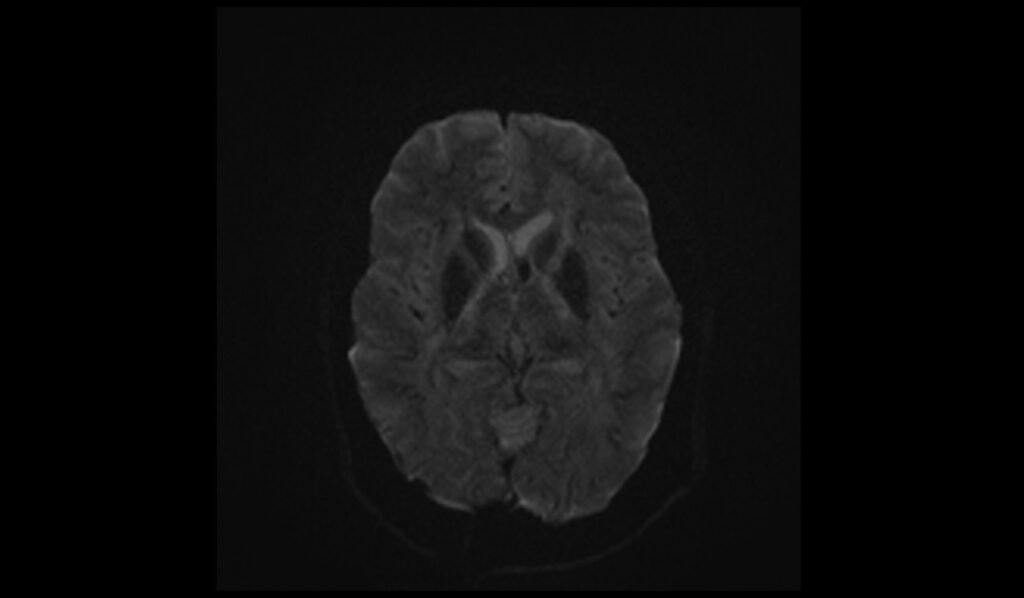
DWI b1000 images shows Fahr Syndrome


DWI ADC images shows Fahr Syndrome
References
- Fnu Amisha, & Munakomi, S. (2023, August 13). Fahr Syndrome. In StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK539883/
- Govindarajan, A. (2013). Imaging in Fahr’s disease: how CT and MRI differ? BMJ Case Reports. https://doi.org/10.1136/bcr-2013-201523
- Sahin, N., Solak, A., Genc, B., & Kulu, U. (2015). Fahr disease: Use of susceptibility-weighted imaging for diagnostic dilemma with magnetic resonance imaging. Quantitative Imaging in Medicine and Surgery, 5(4), 628-632. https://doi.org/10.3978/j.issn.2223-4292.2015.04.01
- Saleem, S., Aslam, H. M., Anwar, M., Anwar, S., Saleem, M., Saleem, A., & Rehmani, M. A. K. (2013). Fahr’s syndrome: literature review of current evidence. Orphanet Journal of Rare Diseases, 8(156). https://doi.org/10.1186/1750-1172-8-156


