MRI Discitis (Spondylodiscitis)
Discitis is an infection in the intervertebral disc space that can lead to inflammation. It often occurs in children but can affect adults as well. This condition can result from a bacterial or viral infection and is relatively rare. The intervertebral discs are the spongy cushions that separate the bones (vertebrae) of the spine, and when these discs become infected, they can swell, causing pain and other symptoms.
Symptoms of Discitis
The symptoms of discitis can vary depending on the severity of the infection and the patient’s age. Common symptoms include:
- Back pain: This is the most frequent symptom, often localized to the affected disc space.
- Abdominal pain: Sometimes, especially in children, the pain may be referred to the abdomen.
- Fever: As with many infections, a fever may develop.
- Difficulty bending or moving the spine: Stiffness and discomfort may occur, making it hard to flex or bend.
- Irritability or discomfort: Especially in children, who may be unable to articulate the source of their discomfort.
- Neurological symptoms: In severe cases, if the infection compresses nerves, there could be numbness, tingling, or weakness.
Causes
Discitis can be caused by a range of bacterial or viral organisms. Staphylococcus aureus is a common bacterial culprit. The infection can reach the disc space through the bloodstream, direct external inoculation, or as a complication from surgery or invasive procedures.
Diagnosis
Diagnosing discitis typically involves a combination of clinical evaluation and imaging tests, such as:
- MRI (Magnetic Resonance Imaging): The most sensitive test for detecting discitis.
- CT (Computed Tomography) Scan: Can also be used, particularly if MRI is not available.
- X-rays: May show narrowing of the disc space or bony erosion in chronic cases.
- Blood tests: Elevated white blood cell count, C-reactive protein (CRP), and erythrocyte sedimentation rate (ESR) can indicate infection.
Treatment
Treatment of discitis involves several approaches:
- Antibiotics or Antivirals: Long-term treatment with the appropriate medications is the mainstay for managing an infectious cause of discitis. The exact type of antibiotics will depend on the suspected or confirmed causative agent.
- Pain Management: Pain relief is an essential part of the treatment, often requiring analgesics and sometimes narcotics, depending on the severity of the pain.
- Rest: Immobilization of the spine can reduce pain and inflammation. In children, this may sometimes require bed rest.
- Bracing: A spinal brace may help to immobilize the affected area and relieve pain by reducing motion at the infected disc space.
- Surgery: In severe or refractory cases, particularly if there is abscess formation, neural compression, or severe vertebral destruction, surgery may be necessary to debride the infection and stabilize the spine.
MRI Appearance of Discitis
T1-weighted images: On T1-weighted MRIs, the normal intervertebral disc appears as a structure with intermediate signal intensity. In discitis, the affected disc space often appears with lower signal intensity (darker) compared to the normal disc due to the presence of edema and inflammation. There may also be a decrease in the height of the intervertebral disc.
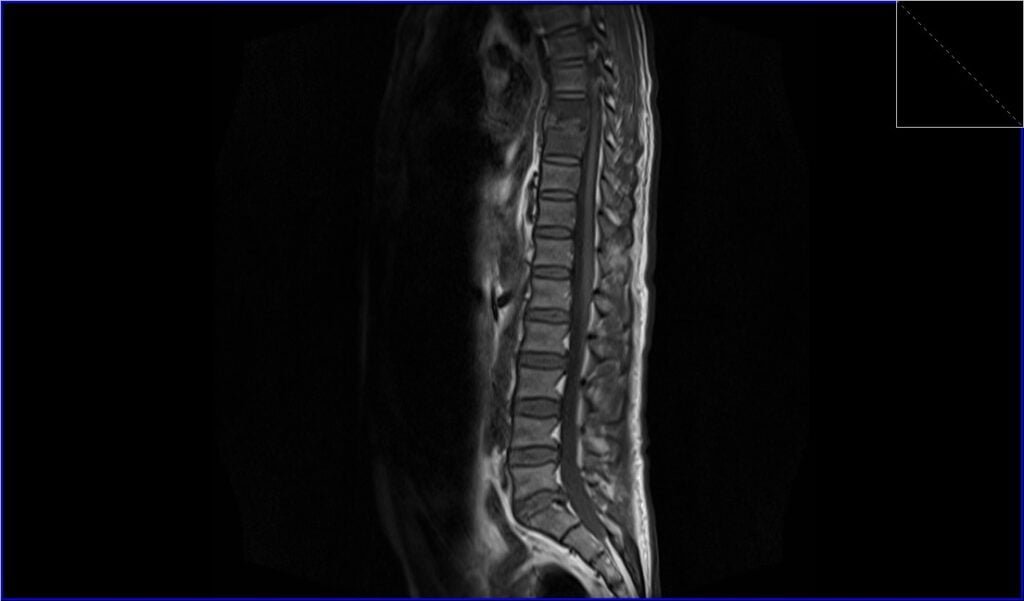
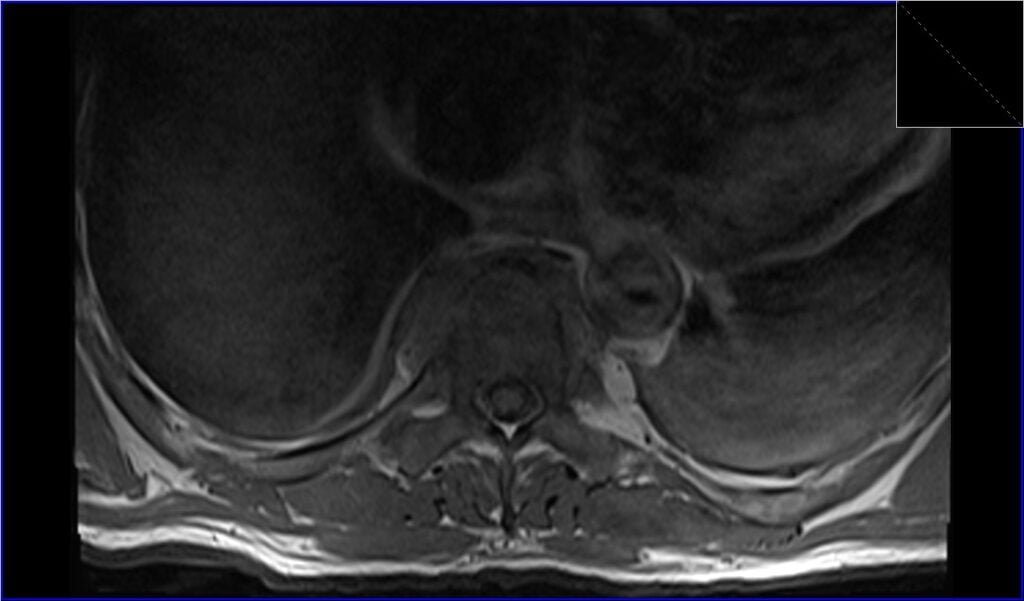
T2-weighted images: On T2-weighted images, fluid and edema associated with inflammation typically appear with higher signal intensity (brighter). An infected disc often shows increased signal intensity, and you may also notice evidence of adjacent bone marrow edema in the vertebral bodies bordering the infected disc space.
STIR images: The STIR sequence is very sensitive to changes in water content and is particularly useful for detecting edema. In the case of discitis, the affected disc space and adjacent bone marrow will appear hyperintense (very bright) due to the presence of inflammation and edema.
Post-contrast T1 with fat saturation images: After the administration of intravenous contrast (usually gadolinium-based), the disc space and adjacent endplates can enhance (appear brighter), indicating increased vascularity and breakdown of the normal blood-disc barrier. Fat saturation is used to suppress the signal from fat, which enhances the contrast between the infected tissues and the surrounding fat, making it easier to detect inflammation, abscess formation, or other complications. In discitis, this can highlight areas of abscess or soft tissue involvement that are not as apparent on non-contrast images.
T2 TSE sagittal image shows discitis

STIR sagittal image shows discitis

T1 TSE sagittal image shows discitis
T2 TSE axial image shows discitis

T1 TSE axial image shows discitis
Post-contrast T1 fat saturation sagittal image shows discitis

Post-contrast T1 fat saturation axial image shows discitis

References
- Yeom JA, Lee IS, Suh HB, Song YS, Song JW. Magnetic Resonance Imaging Findings of Early Spondylodiscitis: Interpretive Challenges and Atypical Findings. Korean J Radiol. 2016 Sep-Oct;17(5):565–580. Published online 2016 Aug 23. doi: 10.3348/kjr.2016.17.5.565. PMID: 27587946. PMCID: PMC5007384.
- Salaffi, F., Ceccarelli, L., Carotti, M., Di Carlo, M., Polonara, G., Facchini, G., Golfieri, R., & Giovagnoni, A. (2021). Differentiation between infectious spondylodiscitis versus inflammatory or degenerative spinal changes: How can magnetic resonance imaging help the clinician? Radiol Med, 126(6), 843–859. doi: 10.1007/s11547-021-01347-7
- Boudabbous, S., Nicodème Paulin, E., Delattre, B. M. A., Hamard, M., & Vargas, M. I. (2021). Spinal disorders mimicking infection. Insights into Imaging, 12, 176. doi:10.1186/s13244-021-01094-7
- Dunbar, J. A. T., Sandoe, J. A. T., Rao, A. S., Crimmins, D. W., Baig, W., & Rankine, J. J. (2010). The MRI appearances of early vertebral osteomyelitis and discitis. Clinical Radiology, 65(12), 974-981.
- Chandrasenan, J., Klezl, Z., Bommireddy, R., Calthorpe, D. (2011). Spondylodiscitis in children: A retrospective series. The Journal of Bone & Joint Surgery British Volume, 93-B(8), 1122-1125.
- Dunbar, J. A. T., Sandoe, J. A. T., Rao, A. S., Crimmins, D. W., Baig, W., & Rankine, J. J. (2010). The MRI appearances of early vertebral osteomyelitis and discitis. Case Reports Clin Radiol, 65(12), 974-981.
- Förster A, Pothmann R, Winter K, Baumann-Rath CA. Magnetic resonance imaging in non-specific discitis. Case Reports Pediatr Radiol. 1987;17(2):162-3. doi:10.1007/BF02388100. PMID: 3562112.
