Chondromalacia MRI
Chondromalacia, also known as chondromalacia patellae, is a condition characterized by the softening and breakdown of the cartilage on the underside of the patella. This condition often leads to pain and inflammation in the knee joint and is commonly associated with overuse, injury, or other conditions affecting the knee.
Chondromalacia: Overview
Chondromalacia refers to the softening and breakdown of the cartilage on the underside of the kneecap (patella). This condition is often referred to as “runner’s knee” and can cause knee pain and discomfort, especially during activities that put stress on the knee joint.
Causes
Chondromalacia can be caused by:
- Overuse: Repetitive stress on the knee from activities such as running, jumping, or cycling.
- Injury: Direct trauma to the knee, like a fall or a blow.
- Misalignment: Misalignment of the kneecap due to structural abnormalities can cause uneven wear on the cartilage.
- Arthritis: Degenerative changes associated with osteoarthritis can lead to chondromalacia.
Symptoms
The symptoms of chondromalacia may include:
- Knee Pain: A dull, aching pain in the front of the knee, especially when going up or down stairs, kneeling, or sitting for extended periods.
- Swelling: Mild swelling or a feeling of fullness in the knee joint.
- Grinding Sensation: A sensation of grinding or crunching when moving the knee.
- Tenderness: Tenderness around the kneecap, especially when pressing on the area.
Diagnosis
Diagnosis of chondromalacia involves:
- Physical Examination: A doctor will assess the knee for pain, swelling, and tenderness. They may also evaluate the alignment and movement of the patella.
- Imaging Tests: MRI scan is used to visualize the cartilage and rule out other conditions such as bone erosion.
Grading
Chondromalacia is typically graded on a scale from I to IV based on the severity of cartilage damage:
- Grade I: Softening of the cartilage.
- Grade II: Cartilage shows early signs of fragmentation and fissuring (crabmeat appearance).
- Grade III: Fissuring deepens to a size of more than 1.5 cm.
- Grade IV: Erosion of cartilage down to the bone.
Treatment:
Treatment of chondromalacia may involve a combination of approaches:
- Rest and activity modification: Avoiding activities that exacerbate symptoms.
- Physical therapy: Strengthening and stretching exercises to improve muscle balance and knee alignment.
- Orthotics: Shoe inserts or knee braces to improve alignment and reduce stress on the knee.
- Surgery: In severe cases, surgical options such as arthroscopic debridement,
MRI Appearance of Chondromalacia
Grade I Chondromalacia:
- T1:
- Minimal changes are seen. There may be slight irregularities or softening of the cartilage but overall cartilage thickness is maintained.
- PD Fat Sat:
- Minimal or no increase in signal intensity within the cartilage.
- STIR:
- Minimal or no increase in signal intensity within the cartilage.
Grade II Chondromalacia:
- T1:
- Focal areas of increased signal intensity indicating softening or fibrillation of cartilage, but cartilage thickness is still preserved.
- PD Fat Sat:
- Increased signal intensity within the cartilage indicating early cartilage damage.
- STIR:
- Increased signal intensity within the cartilage indicating early cartilage damage and possible edema.
Grade III Chondromalacia:
- T1:
- Areas of thinning of cartilage with irregular surface and increased signal intensity indicating more advanced cartilage damage.
- PD Fat Sat:
- Higher signal intensity within the cartilage with visible cartilage defects.
- STIR:
- High signal intensity within the cartilage with possible subchondral bone edema.
Grade IV Chondromalacia:
- T1:
- Full-thickness cartilage loss with exposed subchondral bone. The subchondral bone may show irregularities and increased signal intensity.
- PD Fat Sat:
- High signal intensity at the site of cartilage loss. The exposed subchondral bone is often hyperintense.
- STIR:
- High signal intensity both in the area of cartilage loss and within the subchondral bone indicating bone marrow edema or subchondral cysts.
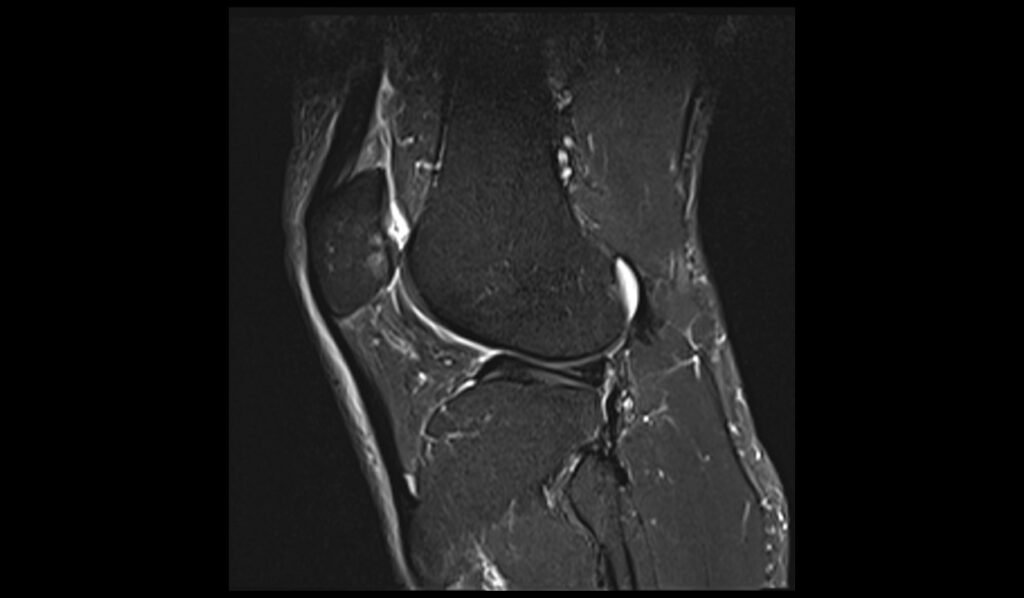
STIR sagittal image shows grade IV Chondromalacia
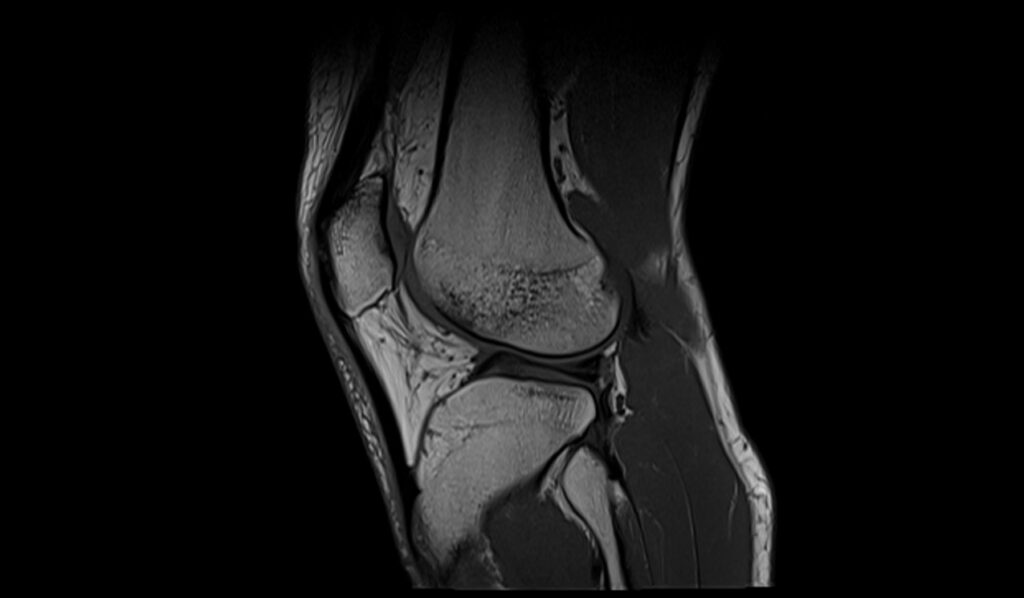
T1 sagittal image shows grade IV Chondromalacia
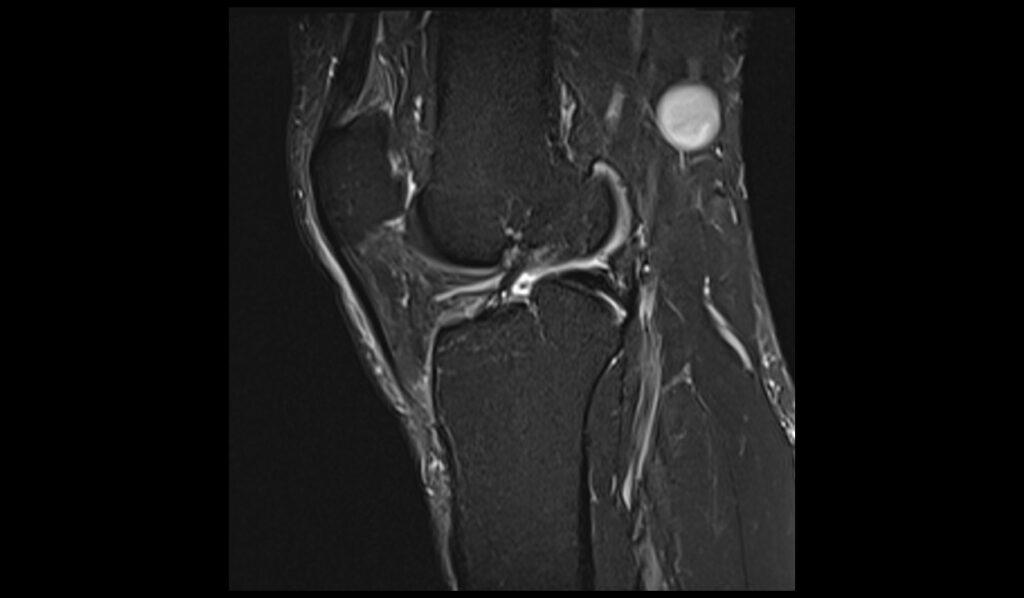
PD FS coronal image shows grade IV Chondromalacia

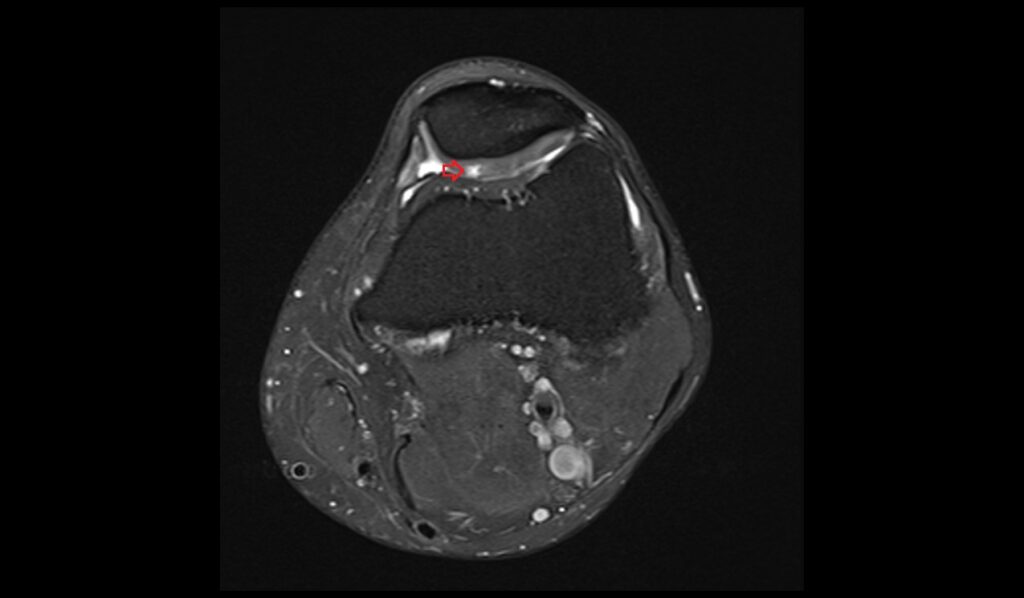
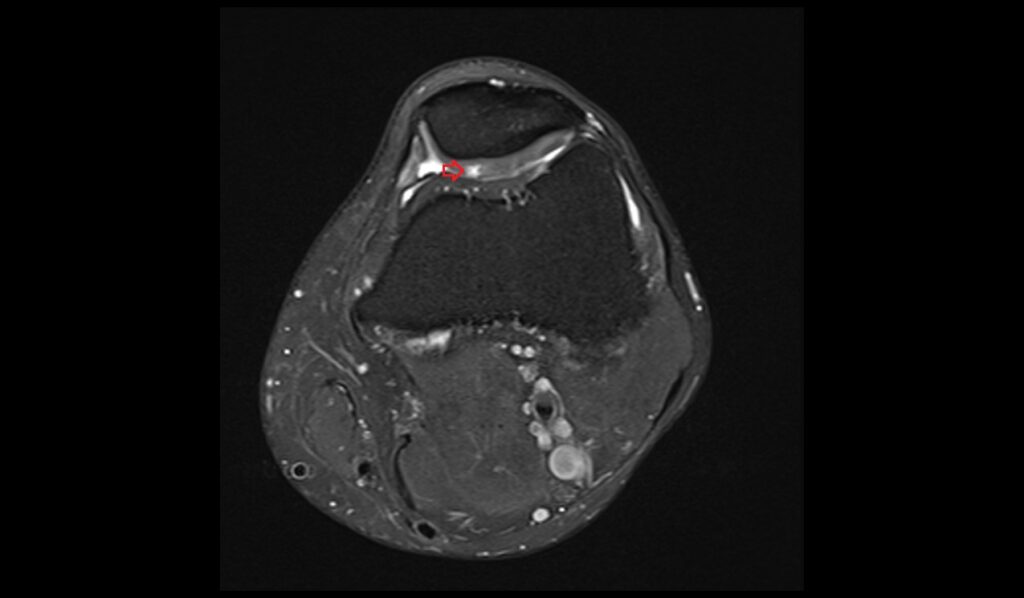
PD FS axial image shows grade IV Chondromalacia
STIR sagittal image shows grade III Chondromalacia
PD FS axial image shows grade III Chondromalacia
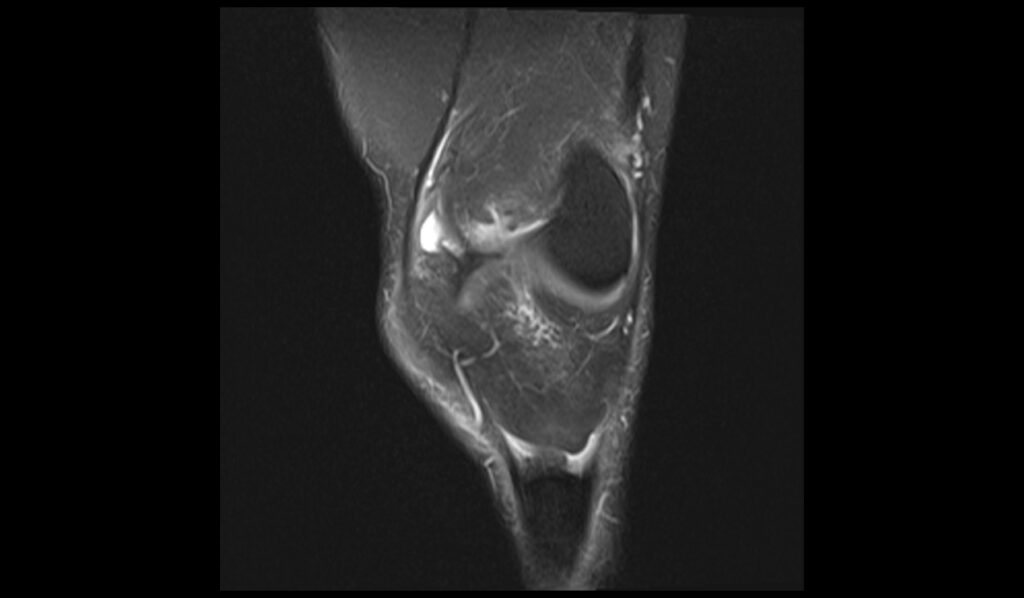
PD FS axial coronal shows grade III Chondromalacia
References
- Pihlajamäki, H. K., Kuikka, P.-I., Leppänen, V.-V., Kiuru, M. J., & Mattila, V. M. (2010). Reliability of clinical findings and magnetic resonance imaging for the diagnosis of chondromalacia patellae. The Journal of Bone and Joint Surgery. American Volume, 92(4), 927-934. https://doi.org/10.2106/JBJS.H.01527
- Ali, S. A., Helmer, R., & Terk, M. R. (2010). Analysis of the Patellofemoral Region on MRI: Association of Abnormal Trochlear Morphology With Severe Cartilage Defects. American Journal of Roentgenology, 194(3), 721-727.
- Özgen, A., Taşdelen, N., & Fırat, Z. (2016). A new MRI grading system for chondromalacia patellae. Acta Radiologica, 58(4). https://doi.org/10.1177/0284185116654332


