FLAIR MRI \ Long Tau Inversion Recovery \ Turbo Dark Fluid
FLAIR MRI Physics, Image and Pathological Appearance
FLAIR (Fluid-Attenuated Inversion Recovery) MRI is an imaging technique used to suppress the signal from fluids in the body and improve the contrast between fluids and surrounding tissues.
The physics behind FLAIR MRI involves the use of an inversion recovery pulse sequence. In this sequence, a 180-degree radiofrequency pulse is used to invert the magnetization of the protons in the imaged tissue. This is followed by a delay, known as the inversion time (TI), during which the protons are allowed to recover some of their longitudinal magnetization.
Next, a 90-degree radiofrequency pulse is used to excite the protons, and the resulting signal is measured by the MRI scanner. As the magnetization of the fluids in the tissue (such as cerebrospinal fluid) has not fully recovered, their signal is suppressed in the resulting image, leading to improved contrast between brain tissue and cerebrospinal fluid.
The value of TI (inversion time) used in FLAIR depends on the manufacturer, the strength of the MRI machine, and the desired imaging parameters. Typically, the TI value for FLAIR is set long enough to nullify the signal from CSF, while preserving the signal from other tissues of interest. This value can range from around 2000 to 2500 ms on most MRI machines.
There are mainly two types of FLAIR MRI:
T2-Weighted FLAIR: In this type of FLAIR MRI, the image contrast primarily relies on T2 relaxation properties. T2-Weighted FLAIR is useful for visualizing structures with high water content, such as CSF, edema, and white matter lesions.
T1-Weighted FLAIR: In this type of FLAIR MRI, the image contrast mainly arises from T1 relaxation properties. T1-Weighted FLAIR is useful for visualizing general anatomy and for post-contrast imaging.
The main difference between T1 and T2 FLAIR lies in the type of tissue contrast that is emphasized. T1-weighted FLAIR is more akin to a standard T1 Turbo Spin Echo (TSE) sequence with enhanced tissue contrast, making it suitable for imaging lesions with low water content or for post-contrast imaging of pathology. T2-weighted FLAIR is more effective for imaging lesions with high water content, such as edema or inflammatory processes.

T2 FLAIR MRI
T2 FLAIR (Fluid Attenuated Inversion Recovery) is a type of MRI sequence designed to suppress the signal from fluids such as cerebrospinal fluid (CSF) and to highlight abnormalities that would otherwise be obscured by the high signal of CSF. In T2 FLAIR, long TR (time to repetition) and long TE (time to echo) are used, along with an inversion pulse that suppresses the signal from fluids. The resulting image highlights white matter lesions, infarcts, and other pathologies, making it a useful diagnostic tool in neuroimaging.
Tissue Appearance in T2 FLAIR Imaging
On FLAIR MRI, cerebrospinal fluid (CSF), which typically has a high water content, appears dark due to the specific suppression of its signal. Gray matter appears brighter than white matter, allowing for clear distinction between the two. Any pathological changes or lesions within white matter will manifest as bright spots against the intermediate background of healthy white matter. Here are some examples of tissue appearances in FLAIR MRI:
- Cerebrospinal fluid (CSF): Appears dark on FLAIR MRI due to the selective suppression of its fluid signal.
- Gray matter: Appears intermediate to bright on T2 FLAIR.
- White matter: Appears intermediate to dark on T2 FLAIR.
- Ligaments: Appear hypointense (dark) on T2 FLAIR.
- Muscle: Appears as an intermediate signal on T2 FLAIR.
- Edema: Appears bright on T2 FLAIR due to increased water content.
- Bone: Appears hypointense (dark) on T2 FLAIR.
- Blood vessels: Generally, blood vessels display low signal intensity on FLAIR images, similar to their appearance on T2-weighted images. However, in some situations, they might appear hyperintense due to slow flow or other factors.
- Spinal cord: On T2 FLAIR, the spinal cord appears intermediate to bright because of CSF signal suppression. The surrounding cerebrospinal fluid (CSF) and subarachnoid space appear dark, enhancing visualization of the spinal cord tissue.

Pathology appearance in FLAIR imaging
T2 FLAIR MRI is particularly useful in detecting and characterizing brain and spinal cord pathologies, as it enhances the contrast between areas of abnormal tissue and healthy tissue. Here are some examples of how different brain pathologies and spinal cord conditions appear on FLAIR MRI:
Brain Pathologies:
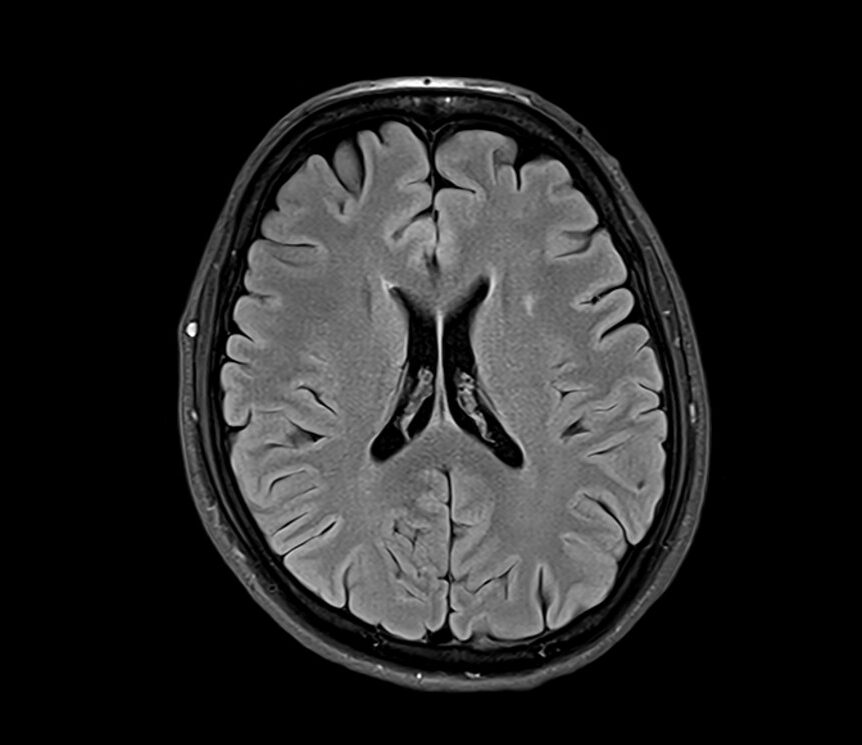
Multiple Sclerosis (MS): FLAIR images often show hyperintense lesions, referred to as plaques, within the brain’s white matter in MS patients. These arise from inflammatory cell accumulation and demyelination.
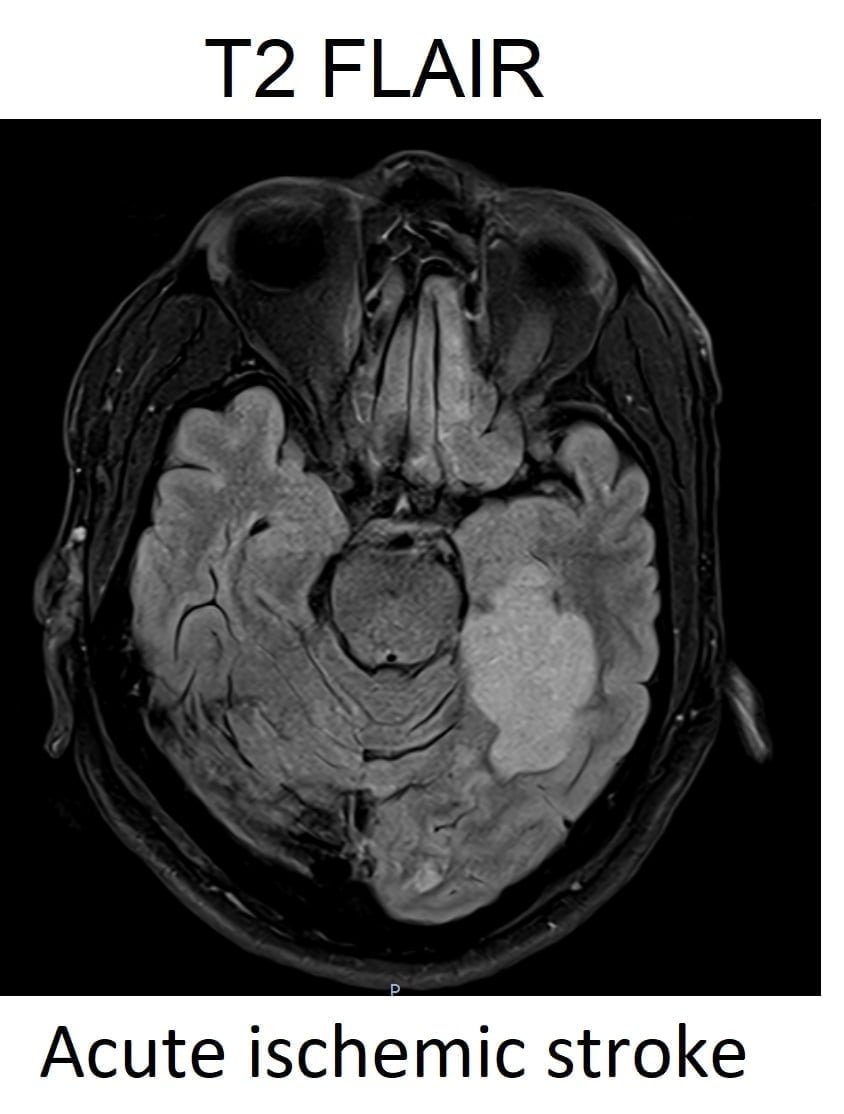
Cerebral Infarction: In the acute phase of an ischemic stroke, affected areas exhibit hyperintensity on FLAIR due to vasogenic edema. As the infarct matures, the FLAIR signal generally diminishes because of the reduced free water.
Brain Tumors: Many brain tumors exhibit hyperintensity on FLAIR due to their increased water content, assisting in their detection and delineation.
Normal Pressure Hydrocephalus (NPH): In NPH, the cerebral ventricles, which contain CSF, appear dark on FLAIR because FLAIR suppresses free fluid signals. The periventricular tissues might appear hyperintense due to transependymal CSF flow.
Inflammation: Inflammatory conditions like meningitis or encephalitis manifest as hyperintense areas on FLAIR owing to increased fluid from inflammation and potential disruption of the blood-brain barrier.
Spinal Cord Pathologies:
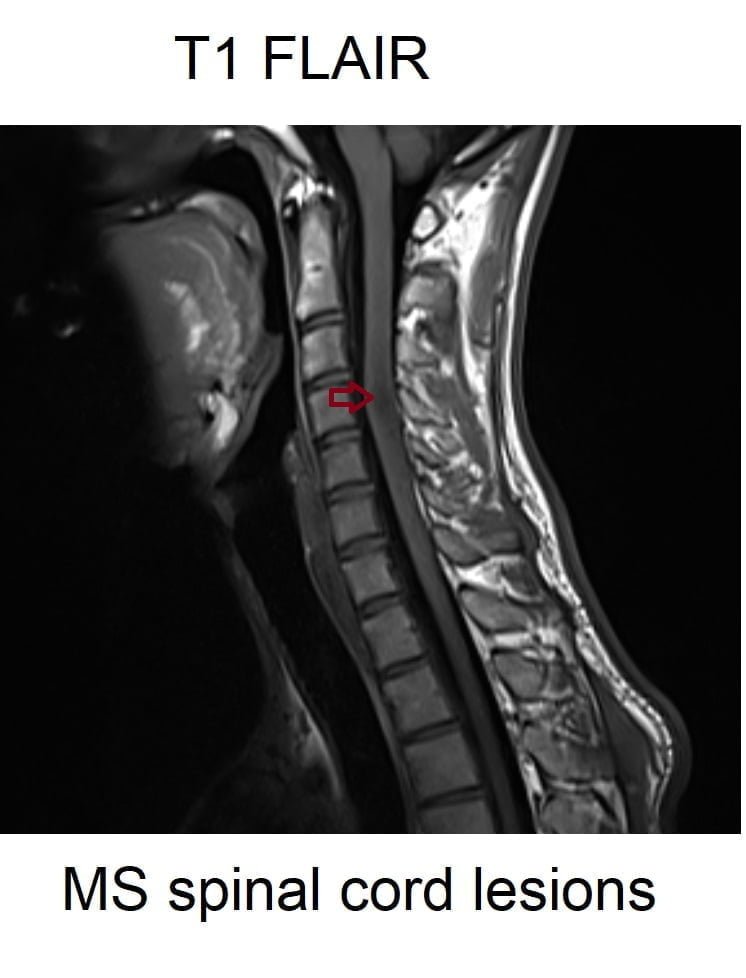
Multiple Sclerosis (MS) Lesions: Just as in the brain, spinal MS lesions are hyperintense on FLAIR, reflecting the water content in the demyelinating plaques.
Spinal Cord Injury: FLAIR can help identify edema and other changes in the spinal cord post-injury, which would appear hyperintense due to increased water content.
Tumors: While many spinal tumors can appear hyperintense on FLAIR due to increased water content or edema, some might appear isointense or even hypointense depending on their specific tissue characteristics.
Infections: Conditions like spinal abscesses or meningitis often present as hyperintense areas on FLAIR, reflecting the increased water content in inflamed or infected regions.



T1 FLAIR MRI
T1 FLAIR (Fluid Attenuated Inversion Recovery) is an MRI sequence type based on the T1 relaxation time of tissues. It is designed to suppress the signal from fluids such as cerebrospinal fluid (CSF) and blood, while retaining the signal from most other tissues.
In T1 FLAIR imaging, a long TR (time to repetition) and a short TE (time to echo) are used, along with an inversion pulse that suppresses the signal from CSF. This results in images highlighting the gray and white matter of the brain, enhancing the visibility of small lesions and subtle pathologies.
T1 FLAIR is particularly useful in detecting contrast-enhancing lesions and has shown to improve the diagnostic accuracy of MRI in certain brain pathologies. It is often preferred over T1-weighted images in 3T MRI due to the increased signal-to-noise ratio and improved image quality at higher field strengths.
Tissue appearances in T1 FLAIR imaging:
On T1 FLAIR MRI of the brain, different tissues exhibit varying appearances due to their inherent T1 relaxation times and the effects of the FLAIR pulse sequence. Here is a summary of tissue appearances:
- Gray matter: Appears darker than white matter due to its shorter T1 relaxation time.
- White matter: Appears brighter than gray matter due to its longer T1 relaxation time.
- Cerebrospinal fluid (CSF): Appears dark due to the suppression of the signal from free water molecules.
- Blood vessels: Appear dark due to the suppression of the signal from flowing blood.
- Bone: Appears dark due to its short T1 relaxation time and the suppression of the signal from the surrounding CSF.
- Muscles: Muscles appear hypointense, but to a lesser degree than bone. This is because muscles have a higher water content than bone, but still have low signal due to the suppression of the high signal from CSF.
- Spinal cord: The spinal cord appears as a homogenous, low signal intensity structure. This is because the fluid in the spinal cord, which would normally produce a high signal, is suppressed by the FLAIR technique

Pathology appearance in T1 FLAIR imaging
T1 FLAIR MRI is primarily used to evaluate structural and functional changes in the brain, spinal cord, and other tissues. It provides high-contrast and high spatial resolution images of various pathologies, aiding in accurate diagnosis and treatment planning.
Here are examples of different pathologies and their appearances on T1 FLAIR MRI:
Multiple Sclerosis (MS): MS is characterized by the formation of demyelinating lesions in the brain and spinal cord. These lesions appear hypointense (dark) on T1 FLAIR MRI due to the absence of myelin.
Cerebral Infarction: Cerebral infarction, a type of stroke caused by the blockage of blood vessels in the brain, results in hypointense (dark) areas on T1 FLAIR MRI due to the accumulation of fluid in the injured tissue.
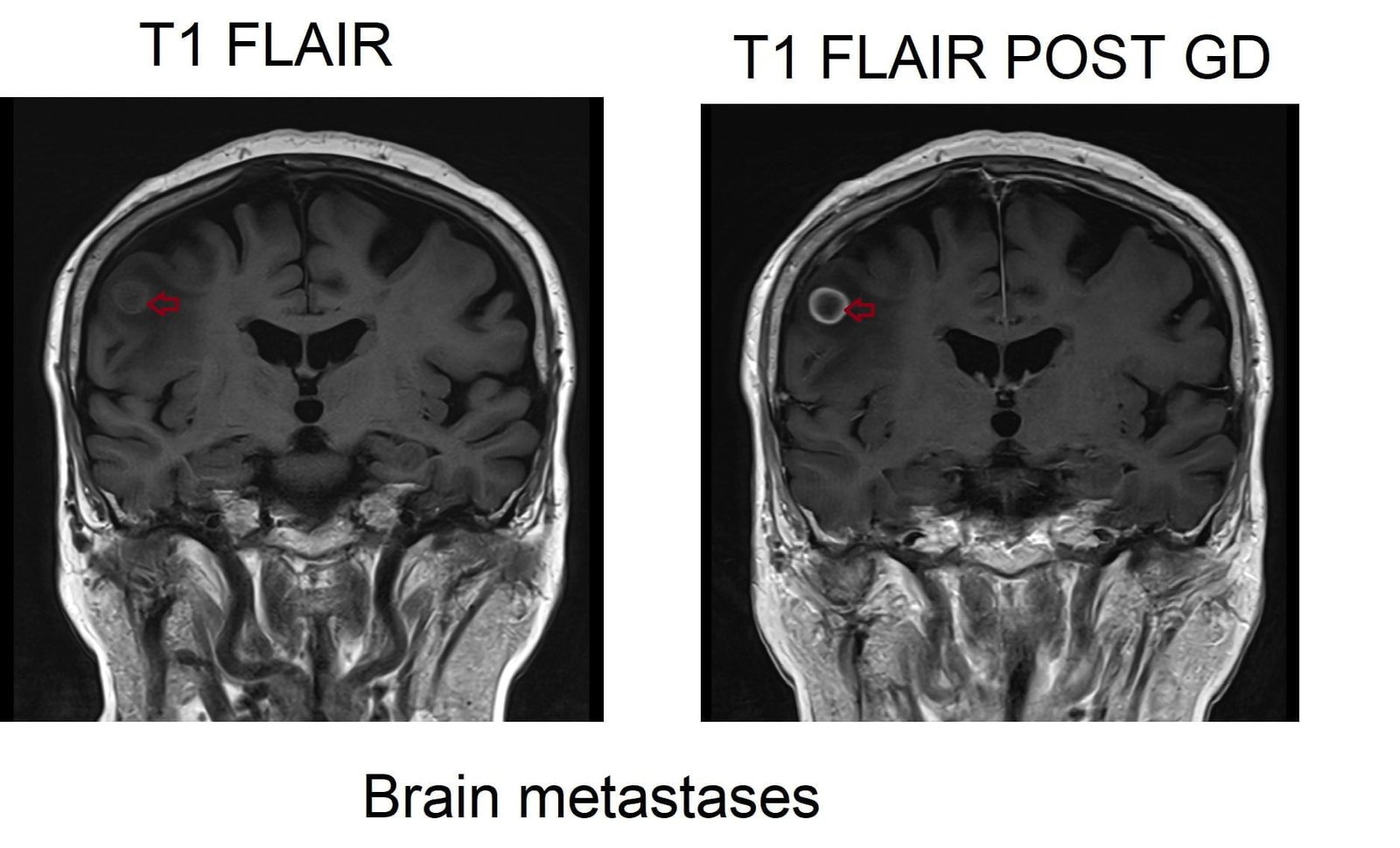
Brain Tumor: Tumors in the brain appear hypointense or isointense (similar to the surrounding tissue) on T1 FLAIR MRI. However, the appearance can vary based on the type, size, and location of the tumor.
Hemorrhage: Hemorrhage refers to bleeding in the brain, often caused by trauma or other medical conditions. The blood appears hyperintense on T1 FLAIR MRI due to the presence of deoxyhemoglobin.
Alzheimer’s Disease: Alzheimer’s disease, a neurodegenerative disorder affecting memory and cognitive function, leads to hypointensity in affected areas on T1 FLAIR MRI due to brain tissue loss.
Syringomyelia: This condition involves the formation of a fluid-filled cavity within the spinal cord. In T1-weighted MRI, the cavity appears as a hypointense (dark) area surrounded by hyperintense (bright) signals from the spinal cord tissue.
Spinal Cord Tumor: Tumors within the spinal cord can appear as masses with varying signal intensities on T1-weighted MRI. They may appear hypointense, isointense, or hyperintense compared to the surrounding spinal cord tissue.
Spinal Cord Infarction: This stroke-like condition occurs when blood flow to the spinal cord is disrupted. In T1 FLAIR MRI, the affected area appears hyperintense due to the accumulation of intracellular and extracellular edema.

T2 FLAIR Appearance of Tissues
Brain:
- CSF: Dark.
- Fat: Bright.
- White Matter: Intermediate to dark.
- Gray Matter: Intermediate to bright.
- Bone (skull): Dark.
- Muscles:Intermediate to dark.
- Bone Marrow: Intermediate to bright.
- Blood Vessels: Mostly Dark; Depending on flow characteristics, can be bright or dark
- Pituitary Gland: Intermediate.
- Choroid Plexus: Intermediate.
- Cerebellum: Gray matter Brighter than white matter.
- Brain Stem: Intermediate.
- Sinuses: Dark (air-filled).
- Thalamus, Hippocampus, Caudate Nucleus: Intermediate.
- Putamen: Intermediate to dark
- Corpus Callosum: Intermediate.
- Pineal Gland: Intermediate.
Spine:
- Spinal Cord: Intermediate.
- CSF: Dark.
- Fat: Bright
- Bone: Dark.
- Bone Marrow: Intermediate to bright.
- Intervertebral Disc: Intermediate
- Ligaments: Intermediate to Dark.
- Nerve Roots: Intermediate.
T1 FLAIR Appearance of Tissues
Brain:
- CSF: Dark.
- Fat: Bright.
- White Matter: Intermediate to bright.
- Gray Matter: Intermediate to dark.
- Bone (skull): Dark.
- Bone Marrow: Intermediate to bright.
- Blood Vessels: Mostly Dark; Depending on flow characteristics, can be bright or dark
- Pituitary Gland: Intermediate.
- Choroid Plexus: Intermediate.
- Cerebellum: Gray matter darker than white matter.
- Brain Stem: Intermediate to dark.
- Sinuses: Dark (air-filled).
- Thalamus, Putamen, Hippocampus, Caudate Nucleus: Intermediate.
- Corpus Callosum: Intermediate to dark.
- Pineal Gland: Intermediate.
Spine:
- Spinal Cord: Intermediate.
- CSF: Dark.
- Fat: Bright
- Bone: Dark.
- Bone Marrow: Intermediate to bright.
- Intervertebral Disc: Intermediate
- Ligaments: Intermediate to Dark.
- Nerve Roots: Intermediate.
T2 FLAIR axial sequence used in 1.5T brain imaging

T2 FLAIR FS axial sequence used in 3T brain imaging
T2 FLAIR sagittal sequence used in 3T cervical spine imaging

T1 FLAIR coronal sequence used in 3T Brain imaging

T1 FLAIR sagittal sequence used in 3T cervical spine imaging

T2 FLAIR axial sequence showing multiple sclerosis lesions

References:
- Sati P, George IC, Shea CD, Gaitán MI, Reich DS. FLAIR*: A Combined MR Contrast Technique for Visualizing White Matter Lesions and Parenchymal Veins. Radiology. 2012 Dec;265(3):926-932. doi: 10.1148/radiol.12120208. PMID: 23074257; PMCID: PMC3504317.
- Zwanenburg, J. J. M., Hendrikse, J., Visser, F., Takahara, T., & Luijten, P. R. (2010). Fluid attenuated inversion recovery (FLAIR) MRI at 7.0 Tesla: comparison with 1.5 and 3.0 Tesla. European Radiology, 20(4), 915–922. doi: 10.1007/s00330-009-1620-2.
- Brant-Zawadzki, M., Atkinson, D., Detrick, M., Bradley, W. G., & Scidmore, G. (1996). Fluid-Attenuated Inversion Recovery (FLAIR) for Assessment of Cerebral Infarction: Initial Clinical Experience in 50 Patients. Stroke, 27(7), 1187–1191. DOI: 10.1161/01.STR.27.7.1187.
- Gabr, R.E., Hasan, K.M., Haque, M.E., Nelson, F.M., Wolinsky, J.S., & Narayana, P.A. (2016). Optimal combination of FLAIR and T2-weighted MRI for improved lesion contrast in multiple sclerosis. Journal of Magnetic Resonance Imaging, 43(6), 1501-1502.
- Mustafa, W., Ali, S., Elgendy, N., Salama, S., El Sorogy, L., & Mohsen, M. (2021). Role of contrast-enhanced FLAIR MRI in diagnosis of intracranial lesions. The Egyptian Journal of Neurology, Psychiatry and Neurosurgery, 57, Article 108
- Tsuchiya, K., Katase, S., Yoshino, A., & Hachiya, J. (June 2001). FLAIR MR Imaging for Diagnosing Intracranial Meningeal Carcinomatosis. Neuroradiology, 176(6),
- Zeng L, Wang Q, Liao H, Ren F, Zhang Y, Du J, Liao H, Xie M, Wu W. "FLAIR Vascular Hyperintensity: An Important MRI Marker in Patients with Transient Ischemic Attack." Int J Gen Med. 2022 Jul 14;15:6165-6171. doi: 10.2147/IJGM.S371894. PMID:
- Huisman TA, Sorensen AG. MRI: Basic Principles and Applications. 5th ed. John Wiley & Sons; 2014.
- Huisman, T. A. G. M. (2014). MRI Principles. Springer.
- Jackson, A., & Buckley, D. L. (2014). MRI in practice. John Wiley & Sons.


