Cecal Carcinoma MRI
Cecal carcinoma is a type of cancer that originates in the cecum, which is the first part of the large intestine (colon) located in the lower right abdomen. This type of cancer falls under the broader category of colorectal cancer.
Causes
The exact cause of cecal carcinoma is not known, but several risk factors have been identified:
- Genetic predisposition: Family history of colorectal cancer or inherited conditions such as Lynch syndrome and familial adenomatous polyposis (FAP).
- Age: Most cases occur in individuals over the age of 50.
- Diet: A diet high in red or processed meats and low in fiber.
- Lifestyle factors: Lack of physical activity, obesity, smoking, and heavy alcohol use.
- Medical conditions: Inflammatory bowel diseases, such as Crohn’s disease or ulcerative colitis.
Symptoms
Symptoms of cecal carcinoma can be subtle and often develop slowly. Common symptoms include:
- Abdominal Pain: Often on the right side.
- Changes in Bowel Habits: Persistent diarrhea or constipation, or a change in stool consistency.
- Blood in Stool: Can be either visible blood or occult blood detectable by tests.
- Unexplained Weight Loss: Significant, unintentional weight loss.
- Fatigue: Due to anemia caused by chronic blood loss.
- Bloating or Feeling of Fullness: Particularly after eating small amounts of food.
Diagnosis
Diagnosis of cecal carcinoma involves several steps:
- Colonoscopy: A procedure to visually examine the entire colon and rectum using a colonoscope. Biopsies can be taken during this procedure.
- Imaging Tests: CT scans, MRI, and sometimes PET scans to determine the extent of the cancer and if it has spread.
- Biopsy: Examination of tissue samples under a microscope to confirm the diagnosis.
TNM Staging of Cecal Carcinoma
T – Tumor
This category describes the size and extent of the primary tumor.
- Tis (Carcinoma in situ): Cancer is found only in the innermost lining of the cecum. This is also known as high-grade dysplasia or intramucosal carcinoma.
- T1: The tumor has grown into the submucosa, the layer of tissue underneath the mucosa.
- T2: The tumor has grown into the muscularis propria, the thick muscle layer of the colon wall.
- T3: The tumor has grown through the muscularis propria and into the subserosa or into tissues surrounding the cecum but not into nearby organs.
- T4a: The tumor has grown through the serosa (the outermost layer) of the colon wall.
- T4b: The tumor has grown into or attached to nearby organs or structures.
N – Nodes
This category describes whether the cancer has spread to nearby lymph nodes.
- N0: No regional lymph node involvement.
- N1: Cancer has spread to 1-3 nearby lymph nodes.
- N1a: Cancer is found in 1 regional lymph node.
- N1b: Cancer is found in 2-3 regional lymph nodes.
- N1c: There are no cancer cells in the lymph nodes, but there are small clusters of cancer cells in areas of fat near the lymph nodes.
- N2: Cancer has spread to 4 or more nearby lymph nodes.
- N2a: Cancer is found in 4-6 regional lymph nodes.
- N2b: Cancer is found in 7 or more regional lymph nodes.
M – Metastasis
This category describes whether the cancer has spread to distant parts of the body.
- M0: No distant metastasis (cancer has not spread to other parts of the body).
- M1: Distant metastasis is present.
- M1a: Cancer has spread to one distant organ or set of distant lymph nodes.
- M1b: Cancer has spread to more than one distant organ or to the peritoneum (lining of the abdominal cavity).
- M1c: Cancer has spread to the peritoneum with deposits larger than 2 cm or has spread to multiple organs/regions.
Staging Groups
Based on the TNM categories, the cancer is grouped into stages, from Stage 0 to Stage IV.
- Stage 0 (Tis, N0, M0): The cancer is in its earliest stage and confined to the innermost lining of the cecum.
- Stage I (T1-2, N0, M0): The tumor has grown into the submucosa (T1) or the muscularis propria (T2), but there is no lymph node involvement or distant metastasis.
- Stage II: The tumor has grown more extensively into or through the colon wall, but there is no lymph node involvement or distant metastasis.
- Stage IIA (T3, N0, M0): The tumor has grown through the muscularis propria into nearby tissues.
- Stage IIB (T4a, N0, M0): The tumor has grown through the serosa.
- Stage IIC (T4b, N0, M0): The tumor has grown into or attached to nearby organs or structures.
- Stage III: The cancer has spread to nearby lymph nodes, but there is no distant metastasis.
- Stage IIIA (T1-2, N1/N1c, M0): The tumor has spread to 1-3 lymph nodes.
- Stage IIIB (T3-4a, N1/N1c, M0): The tumor has spread to 1-3 lymph nodes and has grown into nearby tissues.
- Stage IIIC (Any T, N2, M0): The tumor has spread to 4 or more lymph nodes.
- Stage IV: The cancer has spread to distant organs (distant metastasis).
- Stage IVA (Any T, Any N, M1a): Cancer has spread to one distant organ or set of lymph nodes.
- Stage IVB (Any T, Any N, M1b): Cancer has spread to more than one distant organ or to the peritoneum.
- Stage IVC (Any T, Any N, M1c): Cancer has spread to the peritoneum with large deposits or multiple distant organs/regions.
MRI Appearance of Cecal Carcinoma
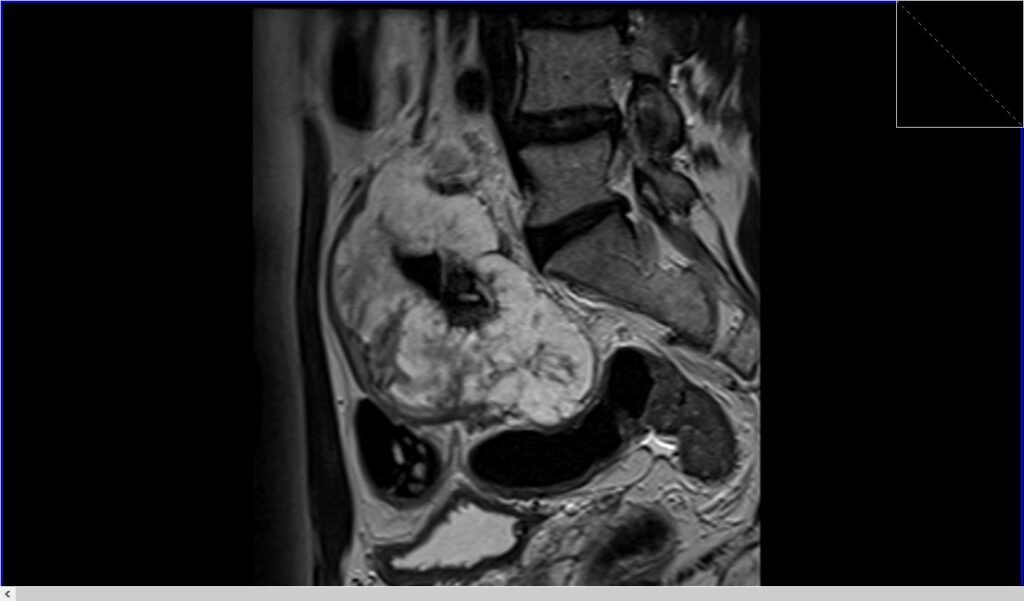
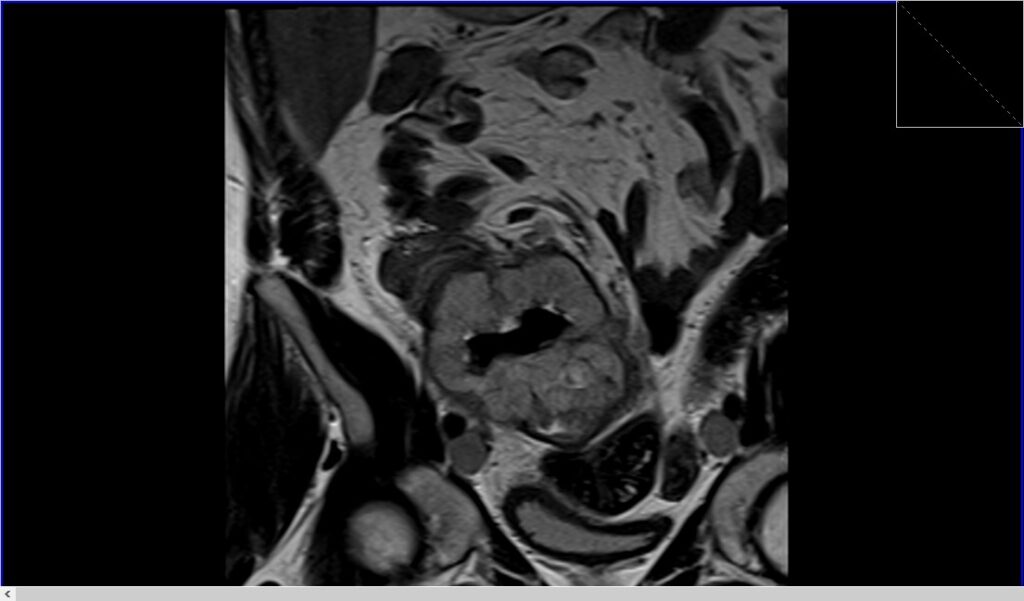
MRI T2 Appearance of Cecal Carcinoma
- On T2-weighted imaging, cecal carcinoma often appears as a heterogeneous mass with mixed signal intensity. The tumor may exhibit areas of high signal intensity due to necrosis or mucinous components, while solid tumor regions might show intermediate to low signal intensity. T2-weighted sequences are crucial for delineating the tumor’s extent and involvement with surrounding structures, providing detailed anatomical information essential for surgical planning and assessment of local invasion.
MRI DWI (b0, b1000, ADC) of Cecal Carcinoma
- DWI Imaging (b0, b1000): Diffusion-weighted imaging (DWI) at b0 and b1000 is a useful tool in the detection of cecal carcinoma. At b0 (no diffusion weighting), the image appears similar to a conventional T2-weighted image, providing anatomical detail. At b1000 (high diffusion weighting), cecal carcinoma often appears as a hyperintense area due to the restricted diffusion of water molecules within the dense cellular structure of the tumor. While DWI is valuable for detecting tumors, it is not commonly used for the staging of cecal carcinoma cancers, as it does not provide sufficient anatomical detail and tissue differentiation required for accurate staging.
- Apparent Diffusion Coefficient (ADC): The apparent diffusion coefficient (ADC) map is derived from DWI images and quantifies the degree of water diffusion within tissues. In the context of cecal carcinoma, the ADC values are typically lower than those of normal tissues due to the restricted diffusion within the tumor. This results in the tumor appearing as a hypointense area on ADC maps.
T2 axial image shows cecal carcinoma at T4 stage

T2 TSE sagittal image shows cecal carcinoma at T4 stage
T2 coronal shows image shows cecal carcinoma at T4 stage
References
- Dam, C., Lindebjerg, J., Jakobsen, A., Jensen, L. H., Rahr, H., & Rafaelsen, S. R. (2017). Local staging of sigmoid colon cancer using MRI. Acta Radiologica Open, 6(7), 2058460117720957. https://doi.org/10.1177/2058460117720957
- Bates, D. D. B., El Homsi, M., Chang, K., Lalwani, N., Horvat, N., & Sheedy, S. (2022). MRI for rectal cancer: Staging, mrCRM, EMVI, lymph node staging and post-treatment response. Clinical Colorectal Cancer, 21(1), 10-18. https://doi.org/10.1016/j.clcc.2021.10.007
- American Cancer Society. (n.d.). Colorectal Cancer Stages. Retrieved May 29, 2024, from https://www.cancer.org/cancer/types/colon-rectal-cancer/detection-diagnosis-staging/staged.html
- American College of Radiology. (n.d.). Staging of colorectal cancer. Retrieved from https://acsearch.acr.org/docs/69339/Narrative/
- Gondal, T. A., Chaudhary, N., Bajwa, H., Rauf, A., Le, D., & Ahmed, S. (2023). Anal Cancer: The Past, Present, and Future. Current Oncology, 30(3), 3232–3250. https://doi.org/10.3390/curroncol30030246


