Baker's cyst rupture MRI
A Baker’s cyst rupture occurs when a Baker’s cyst, also known as a popliteal cyst, bursts or leaks. This cyst is a fluid-filled sac that forms behind the knee joint due to an accumulation of synovial fluid, often caused by another issue within the knee like arthritis or a cartilage tear. When the cyst ruptures, the fluid from inside spills into the calf area, causing pain and swelling.
Causes
The rupture of a Baker’s cyst can be triggered by several factors, including:
- Underlying Knee Conditions: Conditions such as osteoarthritis, rheumatoid arthritis, or meniscal tears, which lead to increased production of synovial fluid.
- Injury or Trauma: Direct trauma or injury to the knee can cause the cyst to rupture.
- Overuse: Repetitive strain or overuse of the knee joint can increase the pressure within the cyst, leading to rupture.
Symptoms
A ruptured Baker’s cyst can present with the following symptoms:
- Sudden Pain: A sharp, intense pain in the calf.
- Swelling: Noticeable swelling in the calf and behind the knee.
- Bruising: Bruising or discoloration may appear below the knee due to the leakage of fluid.
- Stiffness and Reduced Mobility: Difficulty bending or straightening the knee.
- Warmth and Redness: The affected area may feel warm to the touch and appear red.
Diagnosis
Diagnosis of a ruptured Baker’s cyst involves a combination of clinical evaluation and imaging studies:
- Physical Examination: A doctor may detect tenderness, swelling, and bruising in the affected area.
- Ultrasound: Helps visualize the cyst and any fluid leakage into the calf.
- MRI: Provides detailed images of the knee joint and surrounding structures, confirming the presence of a ruptured cyst and ruling out other conditions such as deep vein thrombosis (DVT).
- Doppler Ultrasound: Used to exclude DVT, as the symptoms of a ruptured Baker’s cyst can mimic those of a blood clot.
Treatment
Treatment of a ruptured Baker’s cyst focuses on relieving symptoms and addressing the underlying cause:
- Rest and Elevation: Keeping the leg elevated and avoiding activities that exacerbate symptoms.
- Ice Therapy: Applying ice packs to reduce swelling and pain.
- Compression: Using compression bandages to manage swelling.
- Pain Relief: Over-the-counter pain relievers such as ibuprofen or acetaminophen.
- Aspiration: In some cases, a healthcare provider may drain the fluid from the knee joint.
- Physical Therapy: Exercises to strengthen the muscles around the knee and improve joint function.
- Corticosteroid Injections: To reduce inflammation and pain in the knee joint.
- Surgery: Rarely needed, but may be considered if the cyst is associated with an underlying issue like a meniscal tear or severe arthritis.
MRI Appearance of Baker's cyst rupture
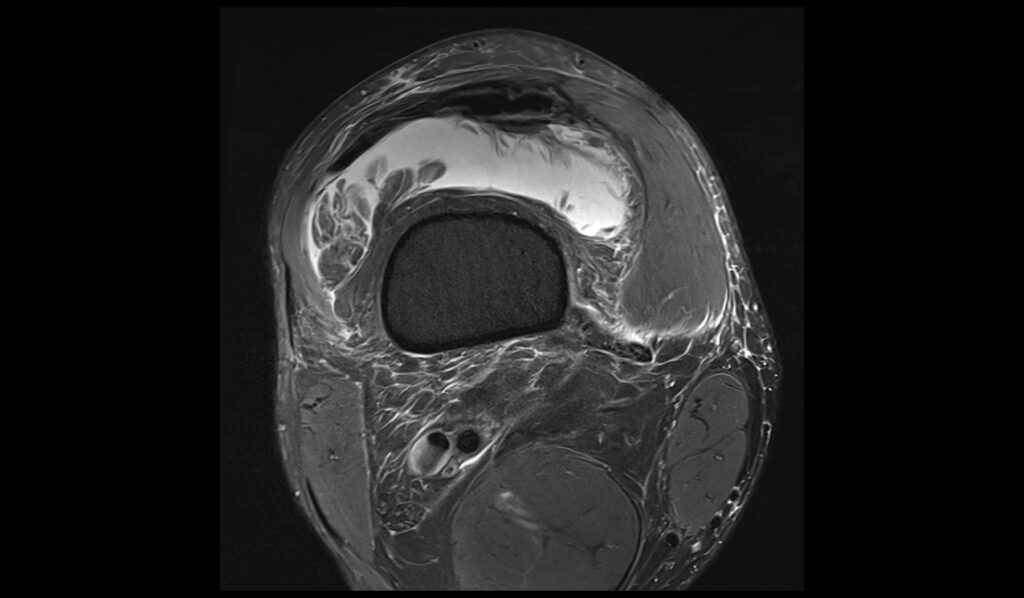
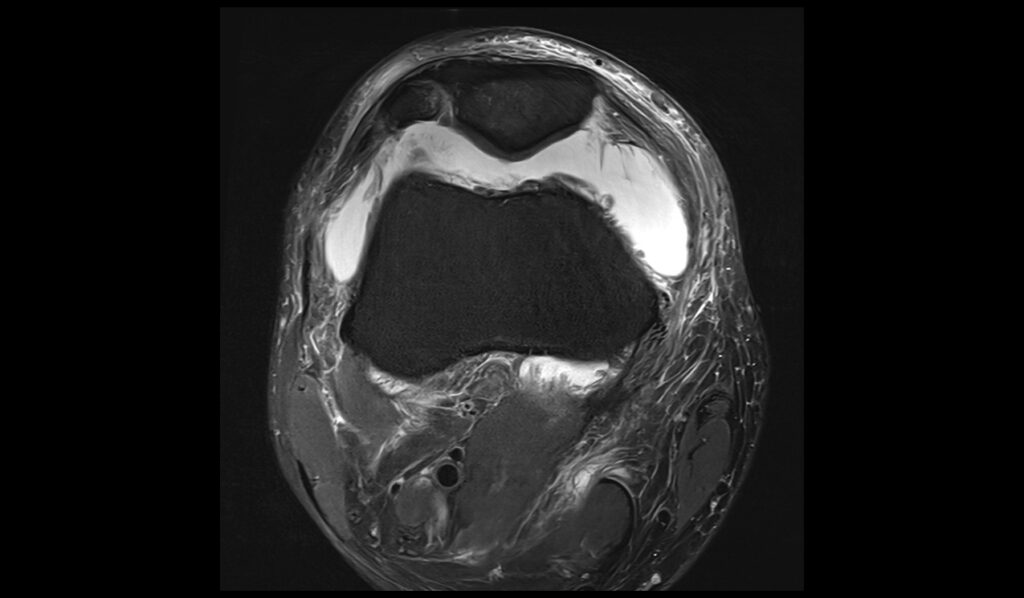
PD FS (Proton Density Fat-Saturated): In the context of a ruptured Baker’s cyst, MRI PD FS imaging typically shows a well-defined fluid collection in the popliteal fossa with high signal intensity, indicative of its fluid content. The fat-saturation technique effectively suppresses the signal from fat, enhancing the contrast between the cyst and surrounding fatty tissues. In cases of rupture, there may be evidence of fluid tracking along the fascial planes of the calf, appearing as linear high-signal areas extending distally from the cyst.
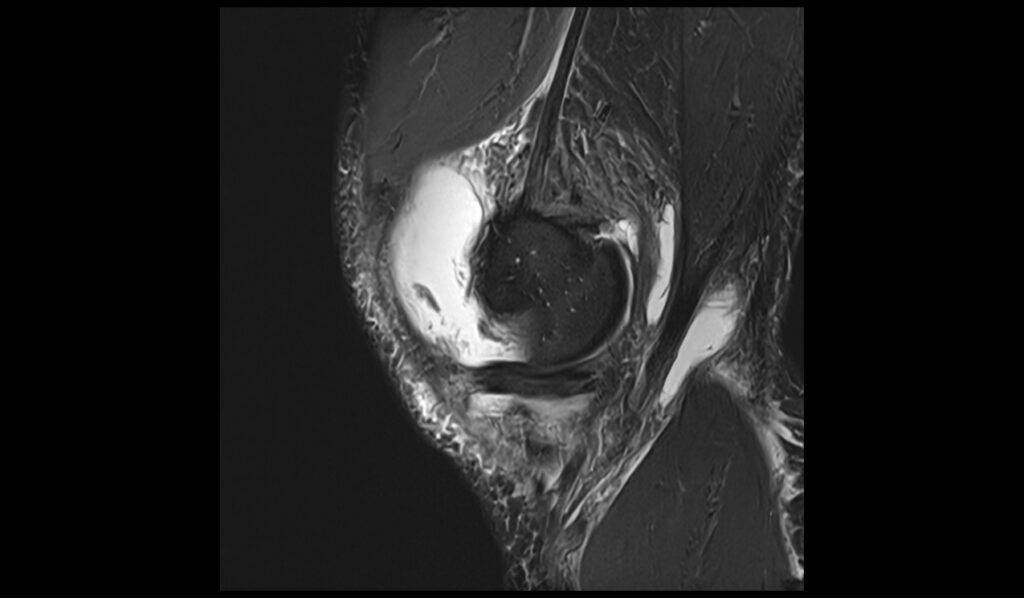
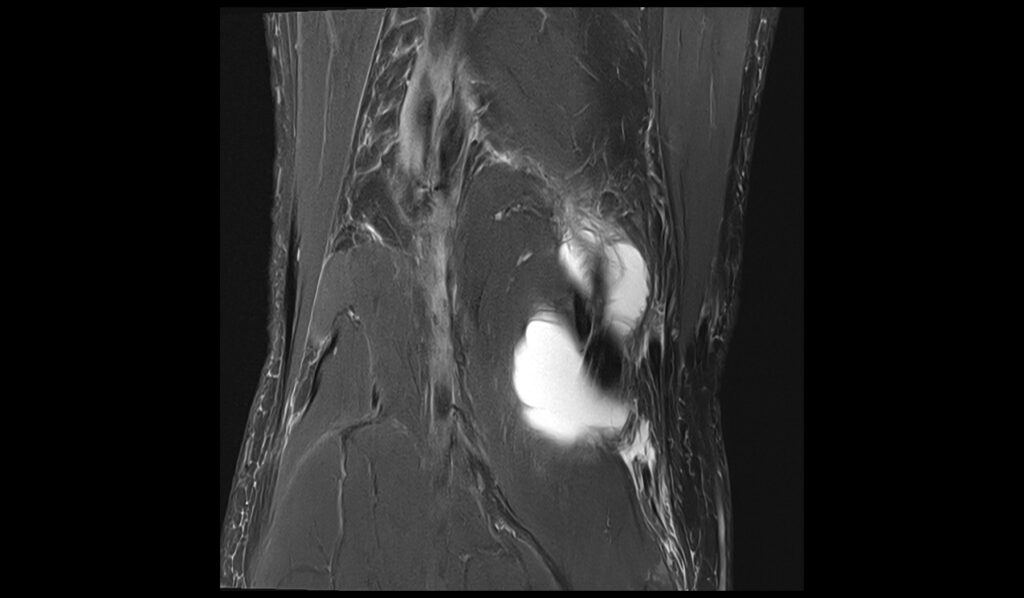
STIR (Short Tau Inversion Recovery): STIR sequences are highly sensitive to fluid and edema, making them particularly useful in visualizing a ruptured Baker’s cyst. The ruptured cyst appears as a high-signal intensity mass in the popliteal fossa. The rupture results in the leakage of cyst fluid, which can cause extensive edema in the surrounding tissues. This edema is characterized by a diffuse high signal on STIR images, often extending along the posterior aspect of the leg, demonstrating the extent of the inflammatory response and fluid dissemination.
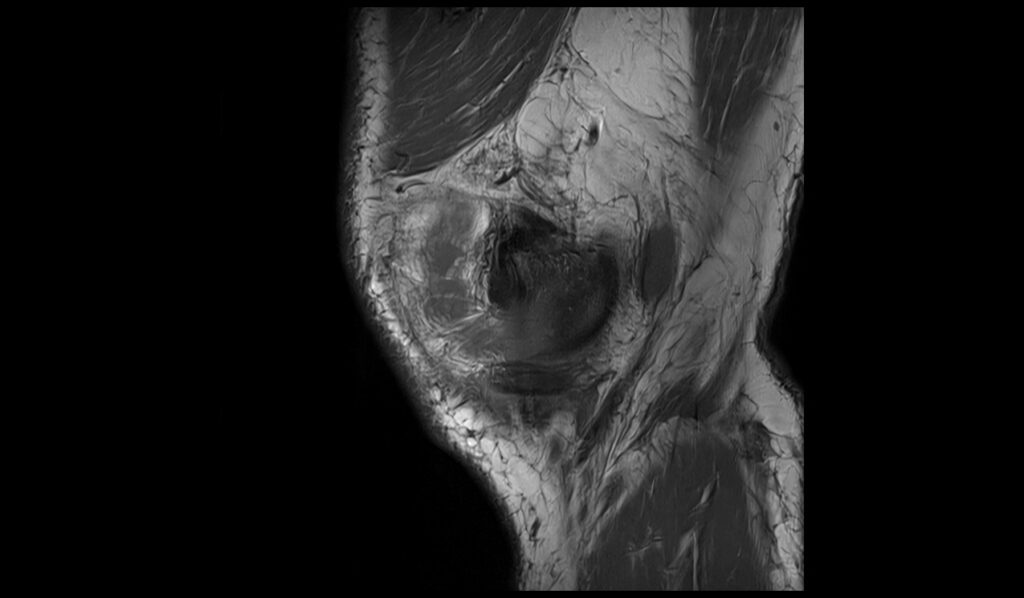
T1-weighted: On T1-weighted MRI images, a Baker’s cyst generally appears as a well-defined mass with low signal intensity, reflecting its fluid content. Upon rupture, the cyst’s fluid content may disperse into the adjacent soft tissues, but it remains low in signal intensity on T1-weighted images. The surrounding inflammatory changes or hemorrhage, if present, might show slightly increased signal intensity due to proteinaceous fluid or blood products. However, the overall contrast between the cyst fluid and surrounding tissues is less pronounced compared to T2-weighted or fat-saturated sequences.
STIR sagittal image shows Baker's cyst rupture





T1 sagittal image shows Baker's cyst rupture


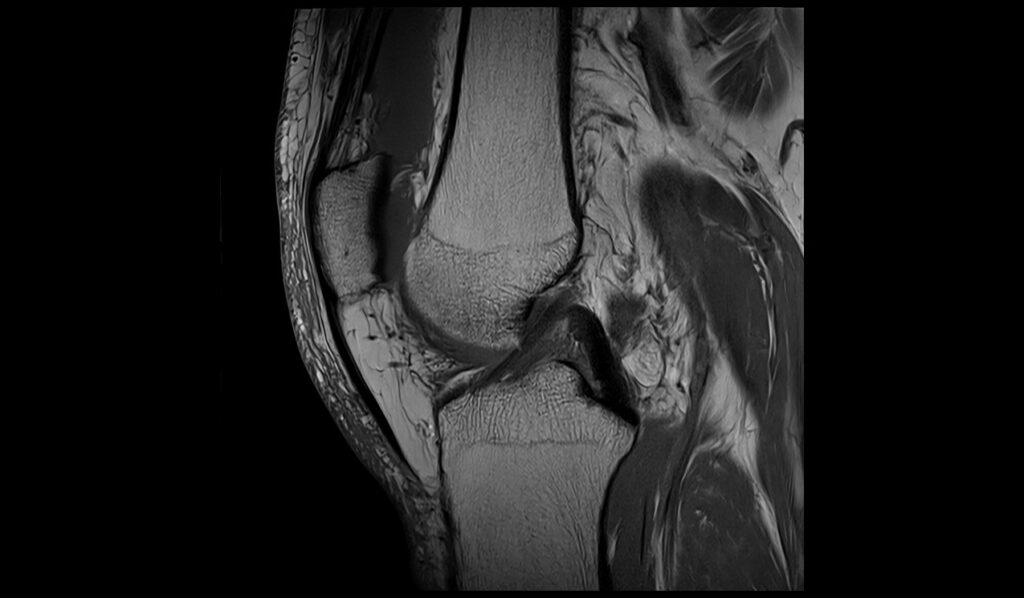

PD FS coronal image shows Baker's cyst rupture





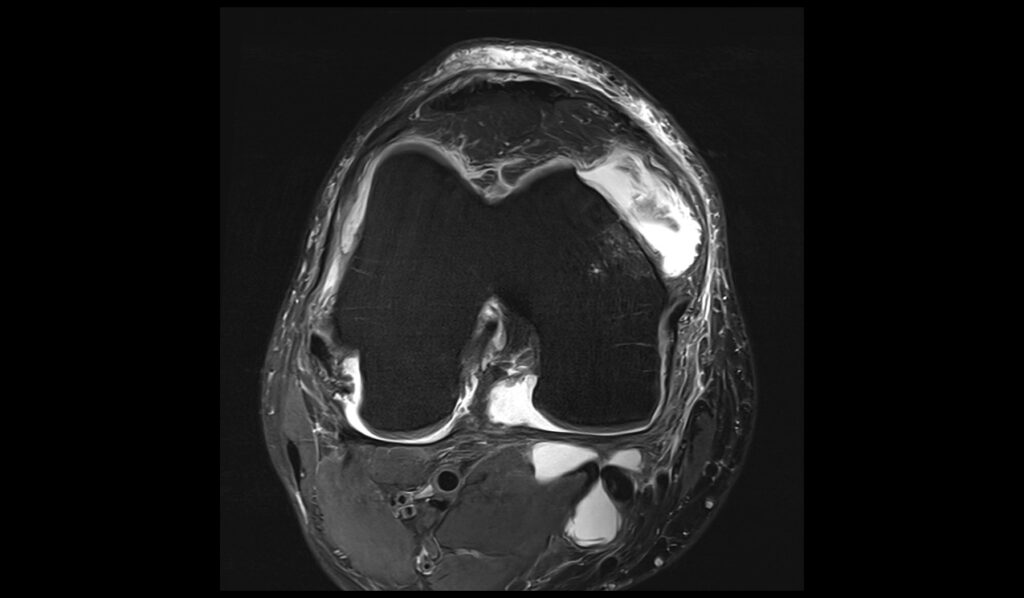
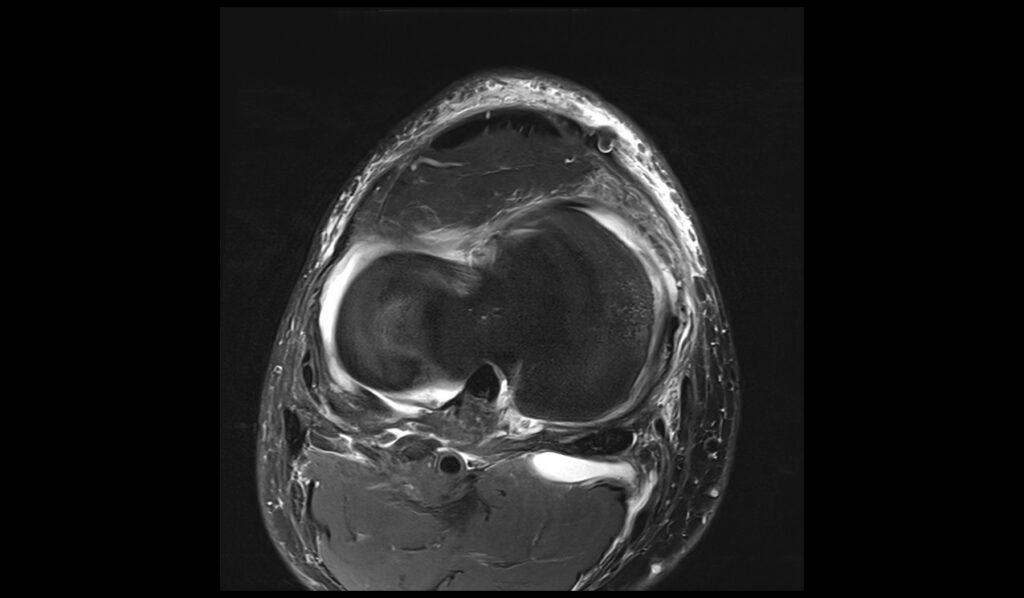
PD FS axial image shows Baker's cyst rupture
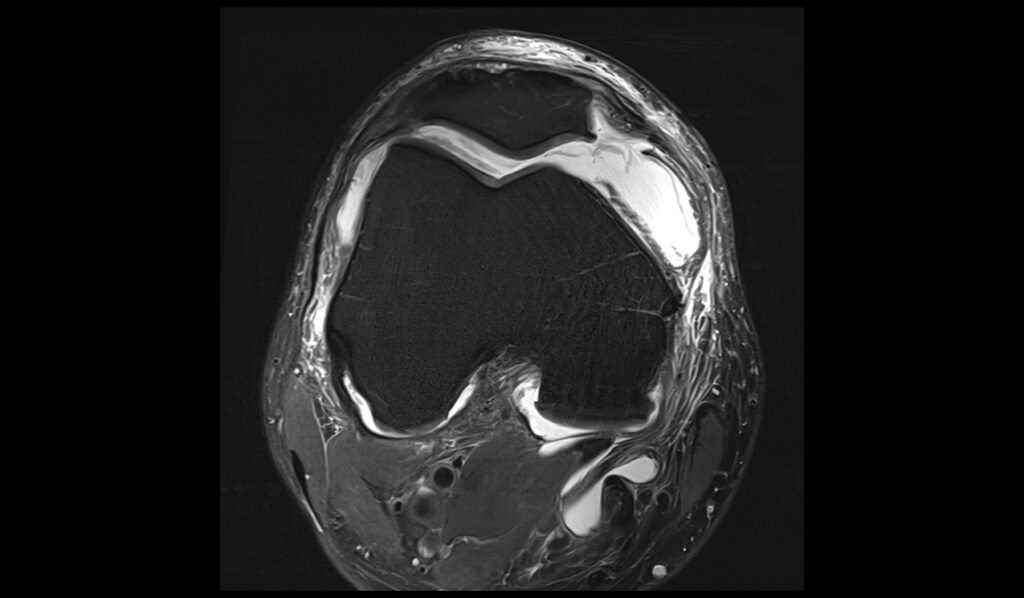
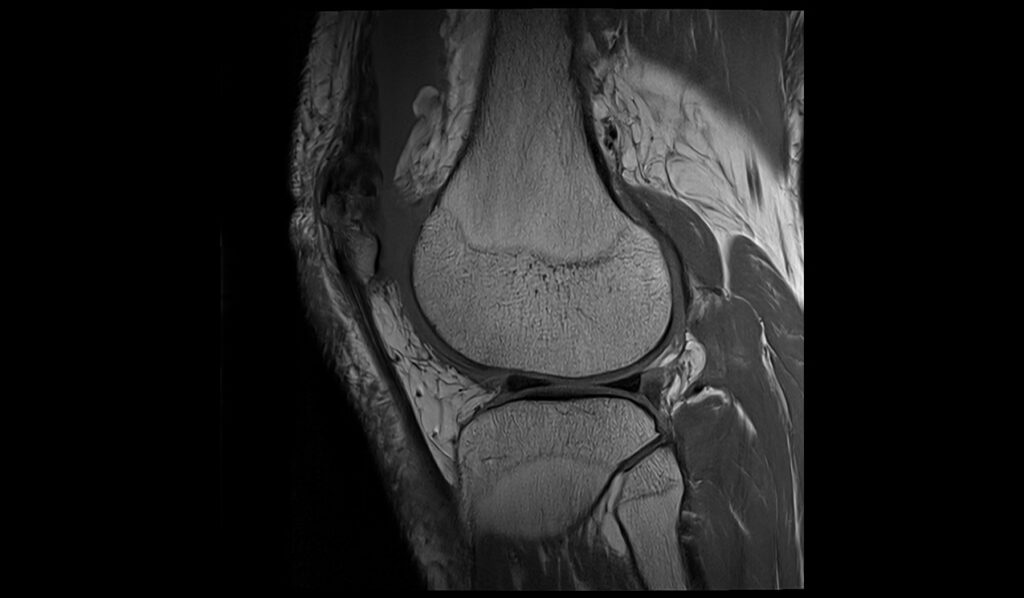
MEDIC(T2*) sagittal image shows Baker's cyst rupture




References
- Kim DK, Lee KC, Kim JK, Kim T. Assessment of Imaging Factors Associated with Baker’s Cyst Rupture on Knee MRI. J Belg Soc Radiol. 2023 Sep 27;107(1):77. doi: 10.5334/jbsr.3258. PMCID: PMC10540859. PMID: 37781476.
- Miller, T. T., Staron, R. B., Koenigsberg, T., Levin, T. L., & Feldman, F. (1996). MR imaging of Baker cysts: Association with internal derangement, effusion, and degenerative arthropathy. Radiology, 201(1). https://doi.org/10.1148/radiology.201.1.8816552
- Verbner, J. M., Pereira-Duarte, M., Zicaro, J. P., Yacuzzi, C., & Costa-Paz, M. (2018). Infected Baker’s Cyst: A New Classification, Diagnosis and Treatment Recommendations. Journal of Orthopaedic Case Reports, 8(6), 16-23. doi: 10.13107/jocr.2250-0685.1238. PMCID: PMC6424320. PMID: 30915286.
- Frush, T. J., & Noyes, F. R. (2015). Baker’s cyst: Diagnostic and surgical considerations. Sports Health, 7(4), 359–365. https://doi.org/10.1177/1941738113520130


