Apparent Diffusion Coefficient (ADC) Map MRI
Apparent Diffusion Coefficient (ADC) mapping is a technique used in magnetic resonance imaging (MRI) to measure and visualize the diffusion of water molecules within tissues. It’s derived from Diffusion-Weighted Imaging (DWI), where diffusion gradients are applied to a T2-weighted spin-echo sequence to assess the mobility of water molecules. The ADC map provides a quantitative measure of this diffusion, reflecting tissue structure at a molecular level.
Physics behind the Apparent Diffusion Coefficient (ADC)
The Apparent Diffusion Coefficient (ADC) map in MRI represents the diffusion of water molecules within tissues and is derived from Diffusion-Weighted Imaging (DWI). In DWI, magnetic gradients are applied to cause dephasing of spins in moving water molecules, leading to a loss of signal from areas of higher molecular motion. The ADC is calculated by applying at least two different strengths of these gradients (denoted as b-values), allowing for the measurement of molecular diffusion independent of other MRI signal influences like the T2 shine-through effect. The resulting ADC value is inversely proportional to the degree of diffusion restriction: higher ADC values indicate freer water mobility (typical of fluids or necrotic tissue), whereas lower ADC values suggest restricted diffusion, as seen in dense cellular structures or fibrotic tissue. This quantitative measurement provides critical insights into the microscopic structure and pathology of tissues.
Importance of b-values in ADC Map
In DWI and ADC mapping, the b-value refers to the strength and timing of the gradients used to generate diffusion weighting. It is a critical factor in ADC quantification:
- Low b-values (e.g., 0-200 s/mm²) are sensitive to slow and fast-moving molecules, but may include T2 shine-through effects.
- High b-values (e.g., 800-1000 s/mm²) enhance the visibility of restricted diffusion by minimizing T2 effects and highlighting areas of high cellular density.
The choice of b-values affects the ADC calculation by influencing the signal intensity decay observed with increased diffusion weighting. Typically, at least two different b-values are used to accurately compute the ADC, helping to eliminate confounding T2 effects and improve the specificity of the imaging findings.
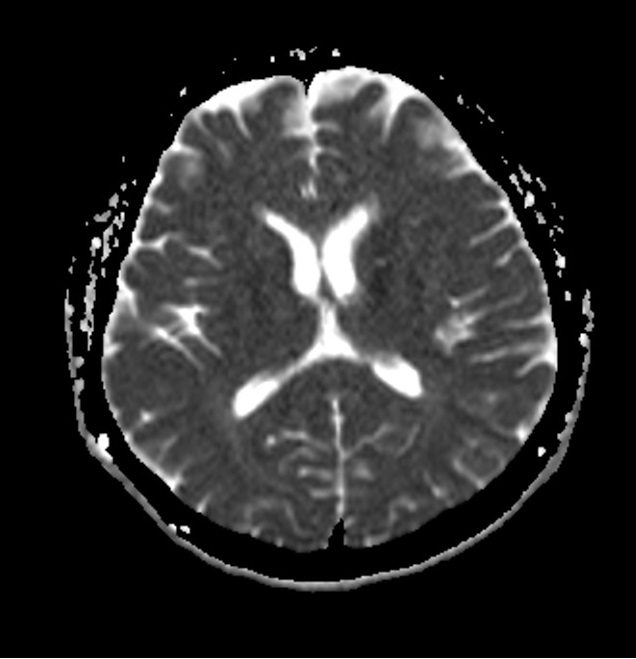
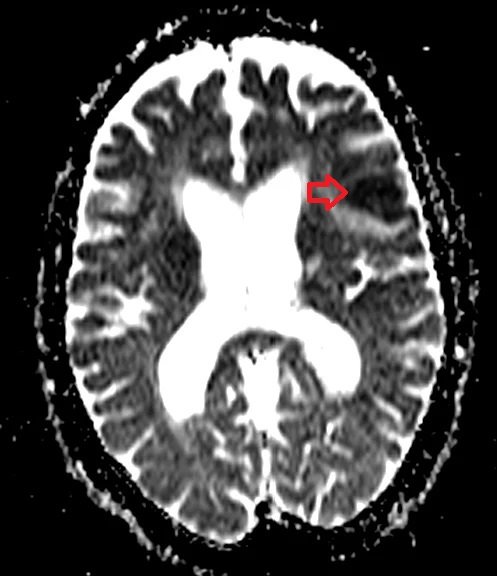
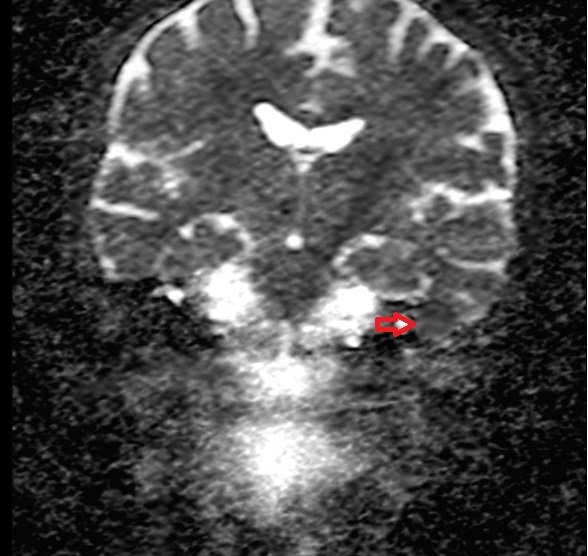
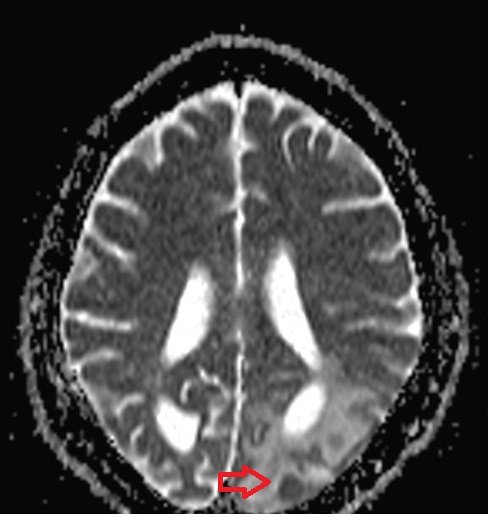
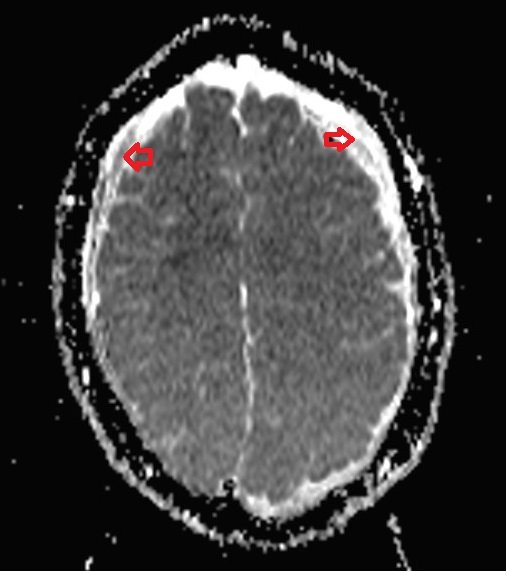
ADC map brain DWI
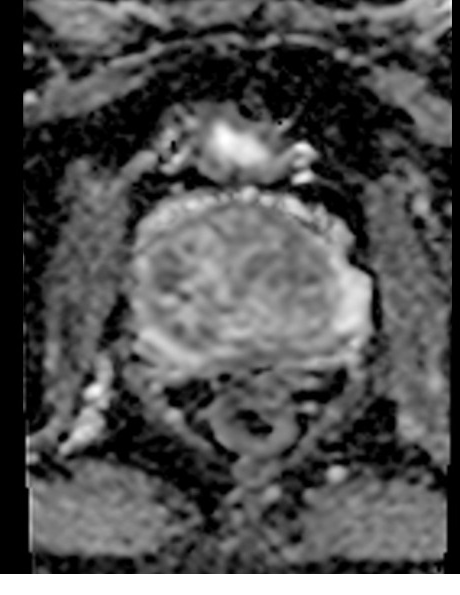
ADC map prostate DWI
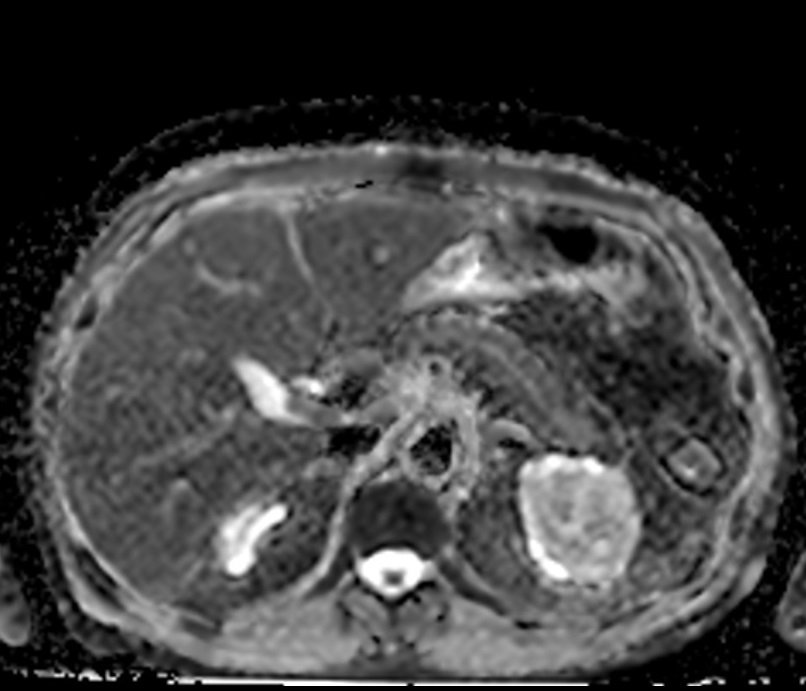
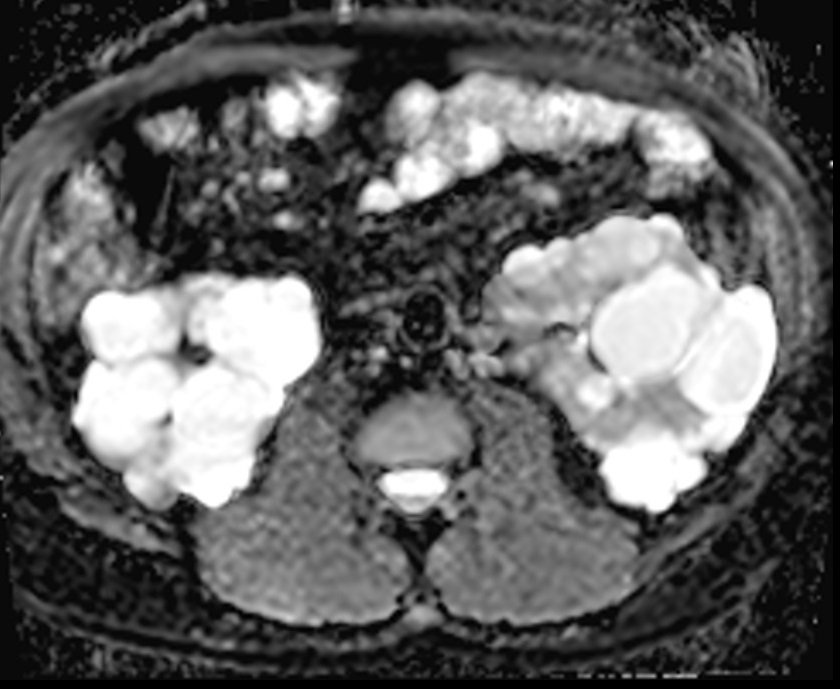
ADC map pancreas DWI
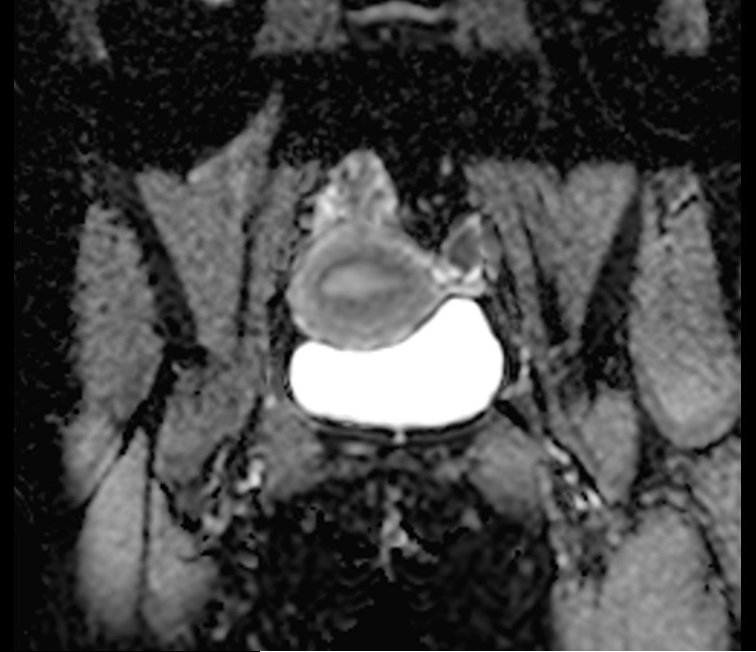
ADC map endometrium DWI
Clinical applications of ADC Map
Stroke Diagnosis: ADC mapping is crucial in the early detection of ischemic strokes. In an acute stroke, the diffusion of water in the brain tissue is restricted due to cellular swelling. ADC maps can help differentiate acute ischemic stroke from other types of brain lesions by showing these areas of restricted diffusion.
Cancer Imaging: ADC maps are used to characterize and differentiate between benign and malignant tumors, especially in the brain, breast, and prostate. Tumors generally restrict diffusion compared to normal tissue, and ADC values can provide insights into tumor cellularity and the integrity of the tissue’s microstructure.
Response to Therapy: ADC mapping can monitor the response of tumors to treatment. For instance, effective therapy typically increases water diffusion in tumors, reflected by higher ADC values. This change can be detected before any actual size reduction of the tumor, providing an early indicator of treatment success.
Fibrosis and Cirrhosis: In liver imaging, ADC mapping can help assess the degree of fibrosis and cirrhosis. Lower ADC values are often associated with increased liver stiffness due to fibrosis.
Neurological Disorders: Beyond strokes and tumors, ADC mapping can assist in the diagnosis of other neurological conditions such as encephalopathies and degenerative diseases, by showing variations in normal and pathological tissue diffusion properties.
- Detecting bone metastases: Especially in cases where other imaging modalities might be inconclusive.
ADC map shows acute stroke
ADC map shows brain glioma

ADC map shows cholesteatoma
ADC map shows brain TB
ADC map shows hematoma
ADC map shows Warthin's tumor

ADC map shows polycystic kidney
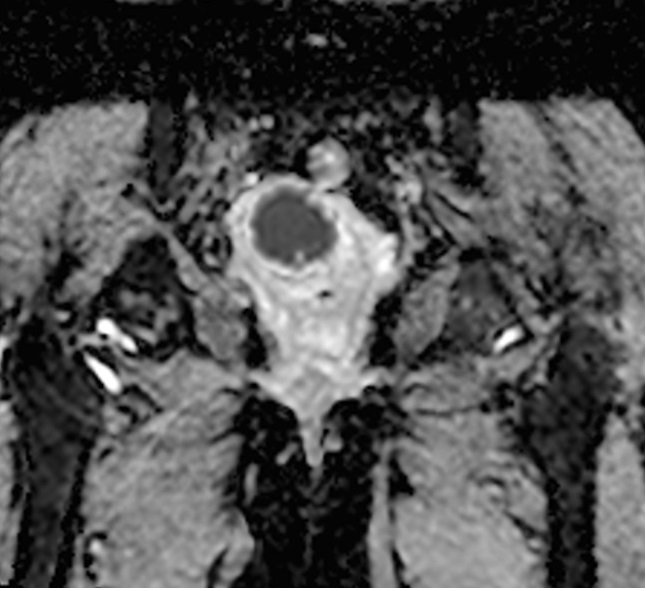
ADC map shows cervical cancer
ADC values for different tissues in the human body
Apparent Diffusion Coefficient (ADC) values can vary significantly based on the pathology, the specific body tissue being examined, and the imaging technique used. Here are some approximate ADC values for different tissues
Brain Tissue:
- Gray matter: Approximately 0.80 to 0.90 x 10^-3 mm^2/s
- White matter: Approximately 0.70 to 0.80 x 10^-3 mm^2/s
- Cerebrospinal Fluid (CSF): Around 2.0 to 3.0 x 10^-3 mm^2/s
- Cerebellum: 0.68 x 10^-3 mm²/s
Liver:
- Normal liver tissue: 0.60 to 1.10 x 10^-3 mm^2/s
Kidney:
- Cortex: 1.50 to 2.50 x 10^-3 mm^2/s
- Medulla: 1.80 to 2.20 x 10^-3 mm^2/s
Breast:
- Normal glandular tissue: 1.20 to 1.80 x 10^-3 mm^2/s
- Fat: 0.90 to 1.10 x 10^-3 mm^2/s
Prostate:
- Normal prostate tissue: 1.40 to 1.80 x 10^-3 mm^2/s
Muscle:
- Skeletal muscle: Approximately 1.00 to 1.50 x 10^-3 mm^2/s
Bone marrow:
- Normal adult bone marrow: 0.20 to 0.60 x 10^-3 mm^2/s
- Cervical vertebrae: 0.43 x 10^-3 mm²/s
- Thoracic vertebrae: 0.29 x 10^-3 mm²/s
- Lumbar vertebrae: 0.33 x 10^-3 mm²/s
- Iliac crest: 0.43 x 10^-3 mm²/s
- Femur: 0.21 x 10^-3 mm²/s
ADC values of different pathologies
Apparent Diffusion Coefficient (ADC) values can vary widely across different pathologies, reflecting changes in tissue characteristics such as cellularity, necrosis, or fibrosis. Below are typical ADC values of a few pathologies.
Brain Pathologies:
- Acute Ischemic Stroke: Typically less than 0.5 x 10^-3 mm^2/s in the affected areas, indicating restricted diffusion due to cytotoxic edema.
- High-grade Gliomas (brain tumors): Often show low ADC values, approximately 0.7-1.0 x 10^-3 mm^2/s due to high cellularity.
- Chronic Infarcts: Higher ADC values than acute strokes, typically greater than 1.2 x 10^-3 mm^2/s, reflecting the loss of cellular structure and increased extracellular space.
Liver Pathologies:
- Hepatocellular Carcinoma (HCC): Generally has lower ADC values ranging from 0.9 to 1.5 x 10^-3 mm^2/s, depending on the level of necrosis and fibrosis.
- Liver Metastases: ADC values can range widely but are often lower than normal liver tissue, typically around 0.8-1.3 x 10^-3 mm^2/s.
- Cirrhosis: Shows decreased ADC values due to increased fibrosis and architectural distortion, generally around 0.5-1.1 x 10^-3 mm^2/s.
Breast Pathologies:
- Malignant Breast Tumors: Typically show lower ADC values, about 0.8-1.3 x 10^-3 mm^2/s, due to increased density and cellularity.
- Benign Breast Lesions: Usually have higher ADC values, about 1.2-2.0 x 10^-3 mm^2/s, reflecting less dense cellular structures.
Prostate Pathologies:
- Prostate Cancer: Lower ADC values generally ranging from 0.6 to 1.0 x 10^-3 mm^2/s, indicating higher cellularity.
- Benign Prostatic Hyperplasia (BPH): Higher ADC values, around 1.5-2.0 x 10^-3 mm^2/s, reflecting the presence of more fluid and less dense tissue.
Musculoskeletal Pathologies:
- Bone Marrow Lesions: ADC values depend on the specific condition but often lower in malignant lesions such as metastases or lymphoma, typically around 0.4-0.7 x 10^-3 mm^2/s.
- Soft Tissue Sarcomas: Vary widely but often exhibit lower ADC values in the range of 0.8-1.2 x 10^-3 mm^2/s due to high tumor cellularity.
Note ****
The ADC values provided above are for illustrative purposes only and should not be used as baseline values for medical diagnosis. These values can vary depending on the pathology, different scanners, and software used. For accurate values, please refer to journals dedicated to specific pathologies.
References
- Kim, B., Yi, K., Jung, S., Ji, S., Choi, M., & Yoon, J. (2014). Clinical applications and characteristics of apparent diffusion coefficient maps for the brain of two dogs. Journal of Veterinary Science, 15(3), 455-458.
- Jacobs, M. A., Ouwerkerk, R., Petrowski, K., & Macura, K. J. (2008). Diffusion Weighted Imaging with ADC Mapping and Spectroscopy in Prostate Cancer. Top Magn Reson Imaging, 19(6), 261–272.
- Ghosh, A., Singh, T., Singla, V., Bagga, R., & Khandelwal, N. (2017). Comparison of absolute apparent diffusion coefficient (ADC) values in ADC maps generated across different postprocessing software: Reproducibility in endometrial carcinoma. American Journal of Roentgenology, 209(6).
- Berro, D. H., Collet, S., Constans, J.-M., Barré, L., Derlon, J.-M., Emery, E., Guillamo, J.-S., & Valable, S. (2019). Comparison between MRI-derived ADC maps and ^18FLT-PET in pre-operative glioblastoma. Journal of Neuroradiology, 46(6), 359-366. Elsevier.
- Perovic, D. J. (2017). Contribution of the determination of numeric value of ADC map in early detection of prostate cancer. Porto Biomedical Journal, 2(5), 213-214.
- Jacobs, M. A., Macura, K. J., Zaheer, A., Antonarakis, E. S., Stearns, V., Wolff, A. C., Feiweier, T., Kamel, I. R., Wahl, R. L., & Pan, L. (2018). Multiparametric whole-body MRI with diffusion-weighted imaging and ADC mapping for the identification of visceral and osseous metastases from solid tumors. Academic Radiology, 25(11), 1405-1414.
- Vermeulen, R. J., van Schie, P. E. M., Hendrikx, L. H., Barkhof, F., & van Weissenbruch, M. (2008). Diffusion-weighted and conventional MR imaging in neonatal hypoxic ischemia: Two-year follow-up study. Radiology, 249(2071581).
