Cavernoma (Cavernous Hemangioma) MRI
A cavernoma, also known as a cavernous hemangioma, is a type of vascular malformation composed of clusters of abnormal, dilated blood vessels. These lesions can occur in various parts of the body but are most commonly found in the brain and spinal cord. Cavernomas are filled with slow-moving or stagnant blood, which can cause them to bleed or leak, leading to various neurological symptoms.
Causes
The exact cause of cavernomas is not fully understood, but they can be either sporadic or familial. Sporadic cases occur without any known family history, while familial cavernomas are inherited in an autosomal dominant pattern. Mutations in the CCM1 (KRIT1), CCM2, and CCM3 genes are known to be associated with the familial form of the disease.
Symptoms
The symptoms of cavernomas can vary widely depending on their location, size, and whether they have bled. Common symptoms include:
- Seizures: Especially if the cavernoma is located in the brain.
- Headaches: These can range from mild to severe.
- Neurological Deficits: Depending on the location, this can include weakness, numbness, balance problems, difficulty speaking, and vision problems.
- Hemorrhage: Bleeding from a cavernoma can cause sudden and severe symptoms such as severe headache, nausea, vomiting, and loss of consciousness.
Diagnosis
Cavernomas are usually diagnosed through imaging studies, which include:
- Magnetic Resonance Imaging (MRI): This is the most sensitive test for detecting cavernomas. It provides detailed images of the brain and spinal cord and can reveal the characteristic “popcorn-like” appearance of cavernomas.
- Computed Tomography (CT) Scan: This can detect bleeding from cavernomas but is less sensitive than MRI for identifying the lesions themselves.
- Genetic Testing: For individuals with a family history of cavernomas, genetic testing can identify mutations associated with the condition.
Treatment
The treatment approach for cavernomas depends on the symptoms, size, location, and whether the lesion has bled. Options include:
- Observation: For asymptomatic cavernomas or those causing mild symptoms, regular monitoring with MRI scans may be recommended.
- Medications: Anti-epileptic drugs can be used to control seizures caused by cavernomas.
- Surgical Removal: This is considered if the cavernoma is accessible and causing significant symptoms or has bled. The goal is to remove the lesion and reduce the risk of future hemorrhages.
- Stereotactic Radiosurgery: A non-invasive procedure that uses targeted radiation to shrink the cavernoma. This option is considered for lesions that are difficult to reach surgically.
MRI appearance of Cavernoma
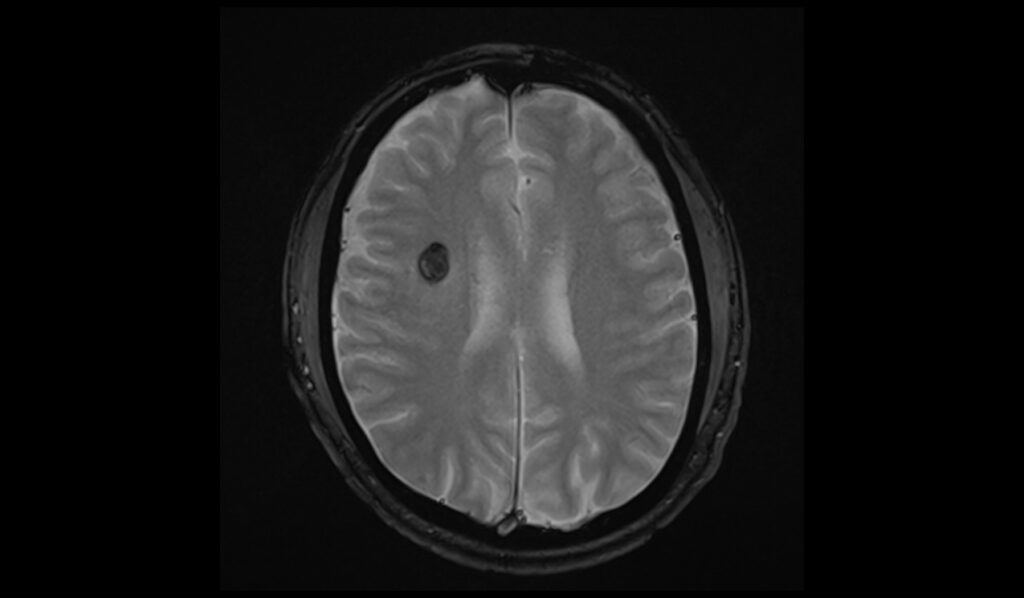
MRI T1 Appearance of Cavernoma
On T1-weighted MRI sequences, cavernomas typically appear as lesions with mixed signal intensity. These vascular malformations often contain areas of hemosiderin deposition, which appear as hypointense (dark) regions due to previous hemorrhage. Additionally, the central part of the cavernoma may show hyperintense (bright) signals if there is subacute blood or methemoglobin present. The mixed signal intensity on T1 images reflects the varied stages of blood breakdown products within the lesion.
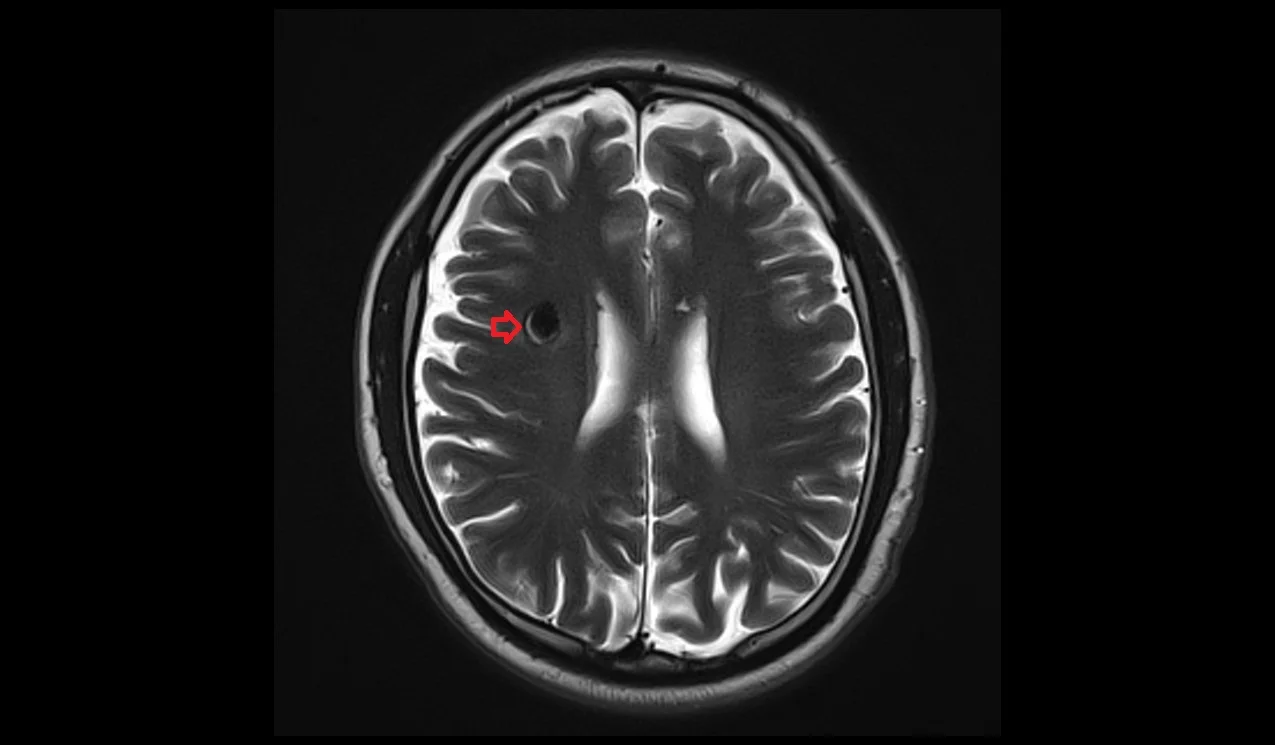
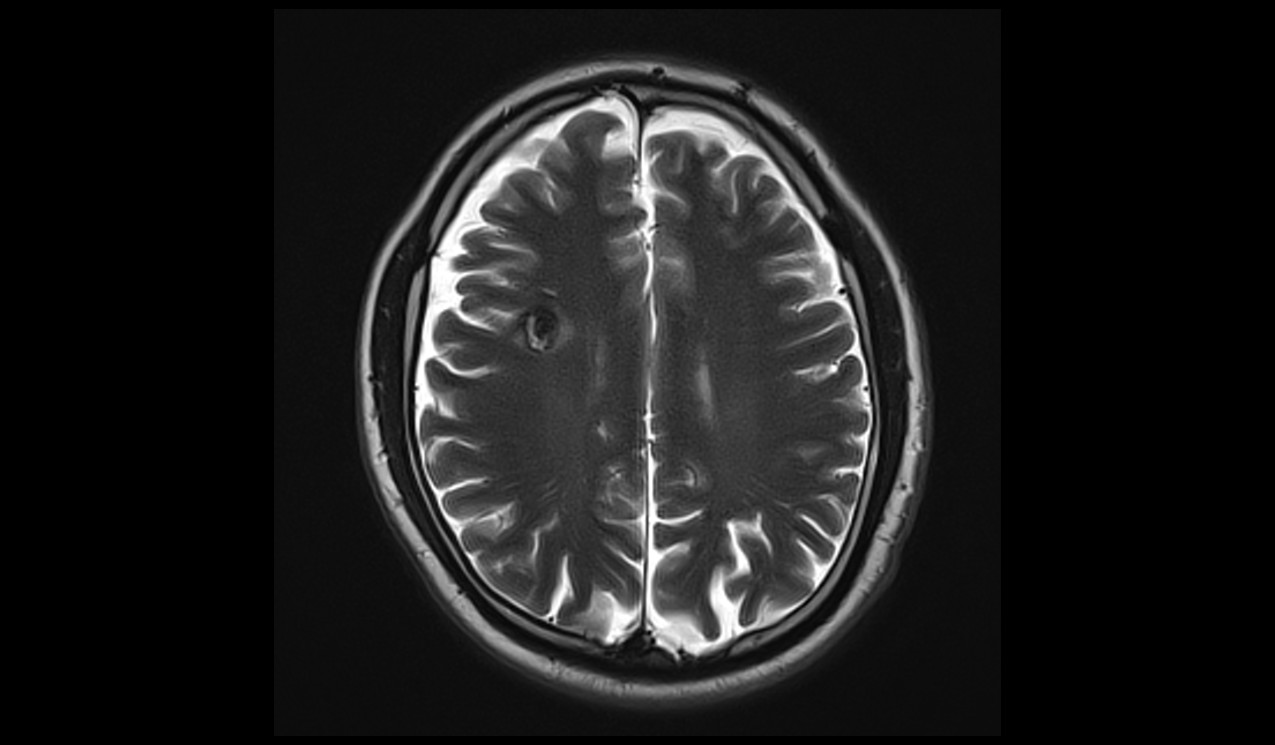
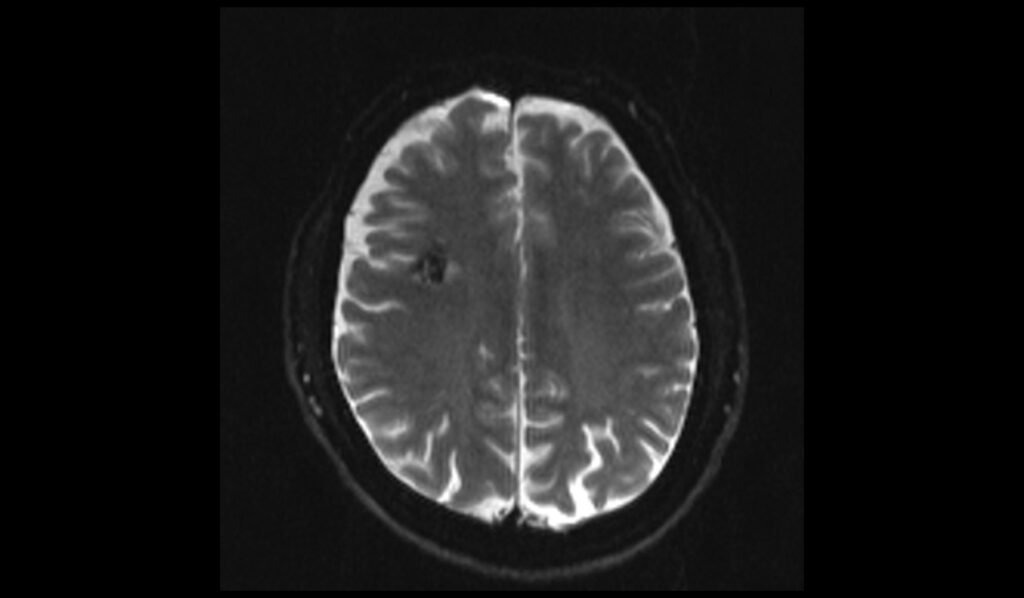
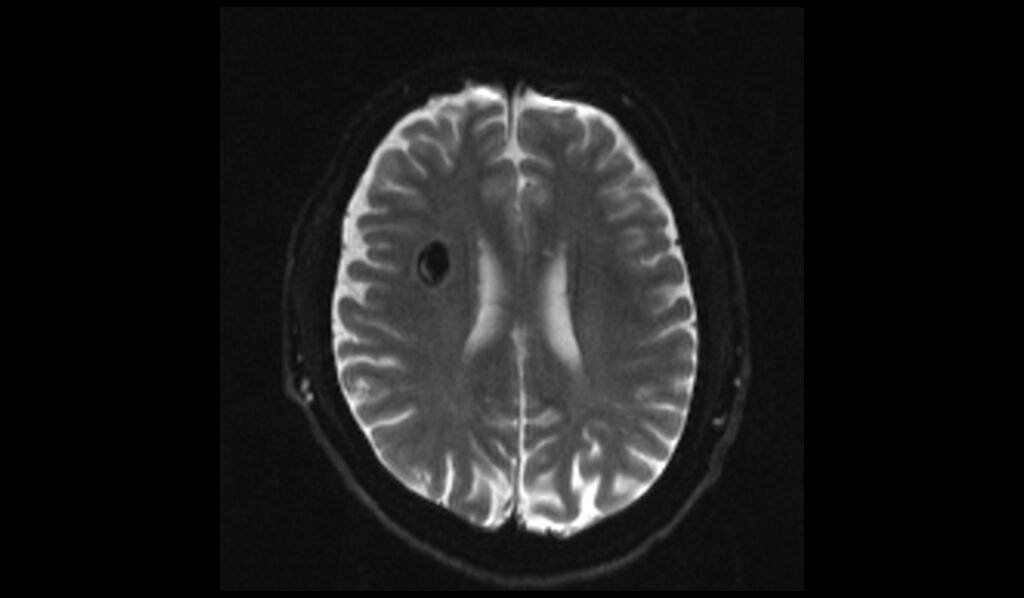
MRI T2 Appearance of Cavernoma
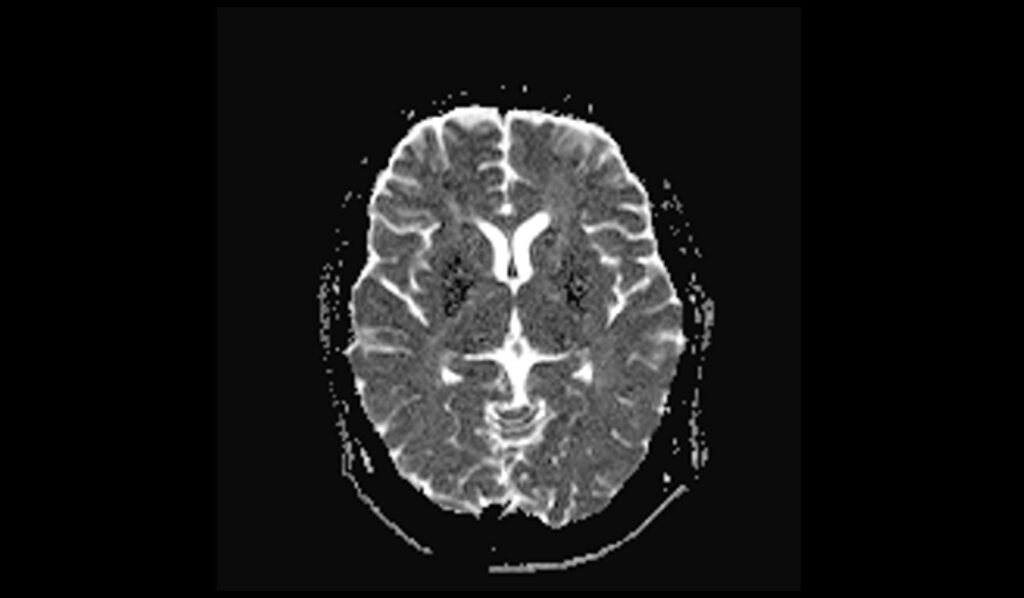
On T2-weighted MRI sequences, cavernomas are characterized by a “popcorn” or “mulberry” appearance with a heterogeneous signal intensity. The lesion often has a central area of mixed signal intensity due to the presence of blood products in various stages of degradation, surrounded by a hypointense rim of hemosiderin. This hypointense rim is due to susceptibility effects from the hemosiderin, which helps in differentiating cavernomas from other vascular malformations. The heterogeneous appearance on T2 images is a hallmark of cavernomas.
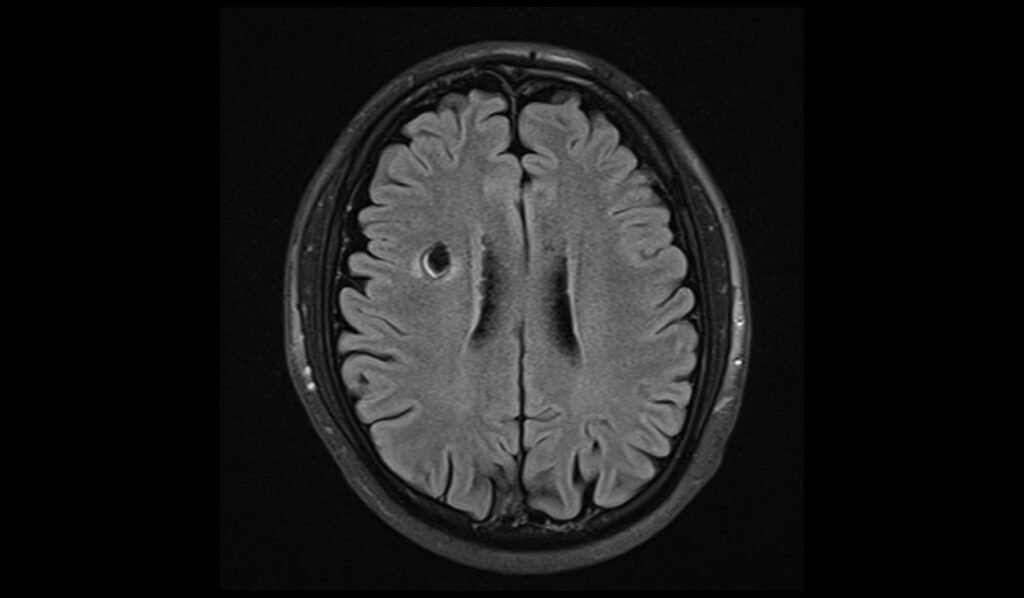
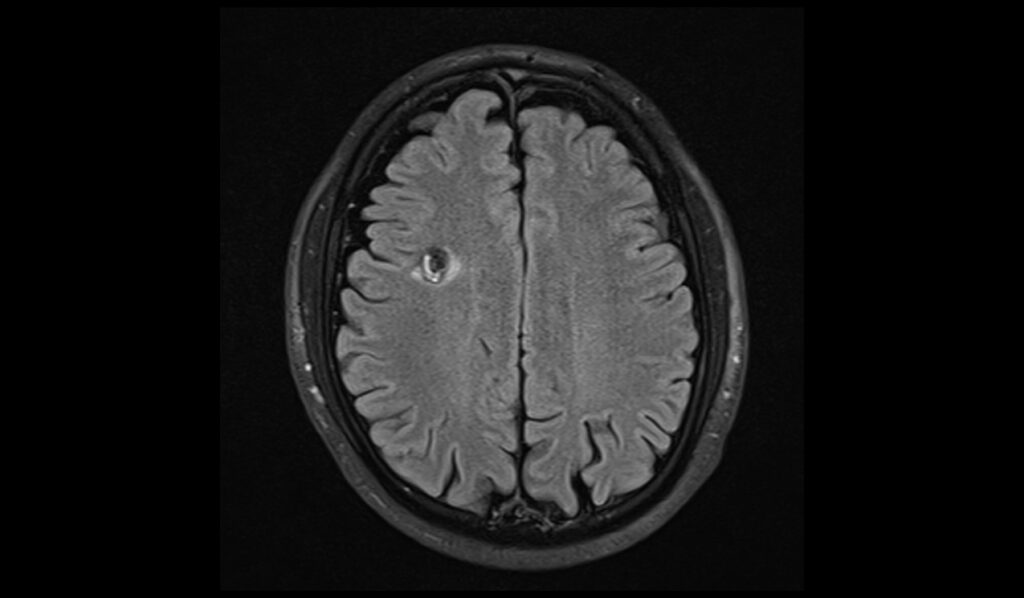
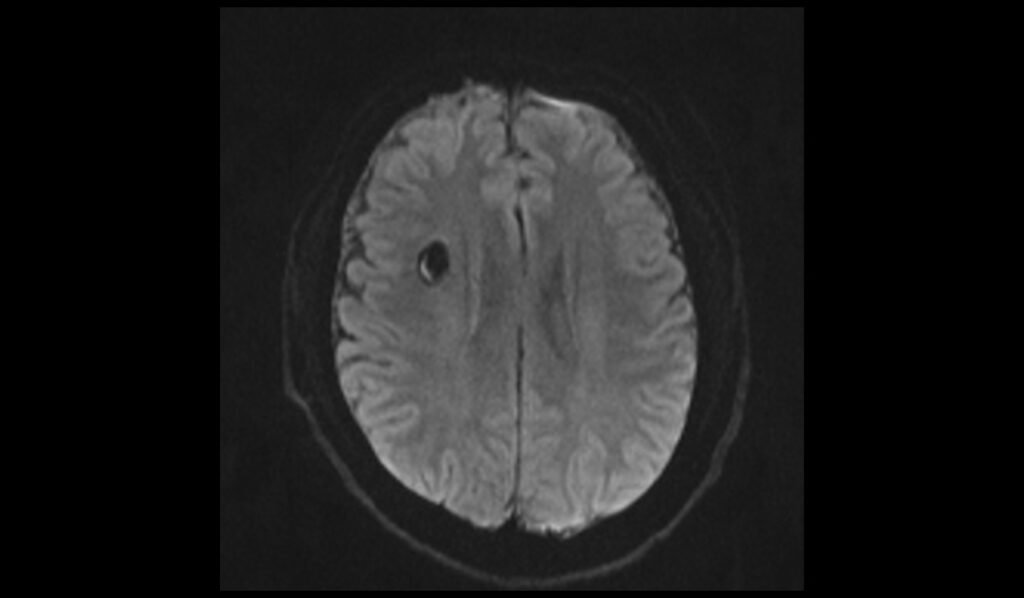
MRI FLAIR Appearance of Cavernoma
Fluid-attenuated inversion recovery (FLAIR) sequences can show cavernomas as lesions with mixed signal intensity, similar to T2 images but with cerebrospinal fluid (CSF) suppression. The central portion may appear hyperintense or isointense, while the surrounding hemosiderin rim remains hypointense. FLAIR is particularly useful for identifying adjacent edema or gliosis, which may present as hyperintense signals around the lesion. This sequence helps in assessing the impact of the cavernoma on the surrounding brain tissue.
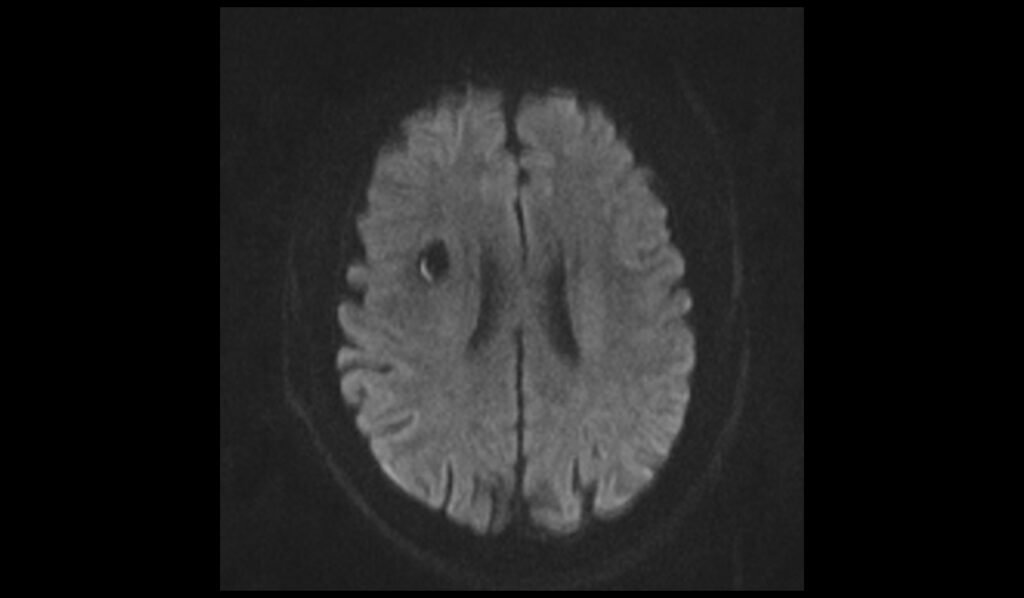
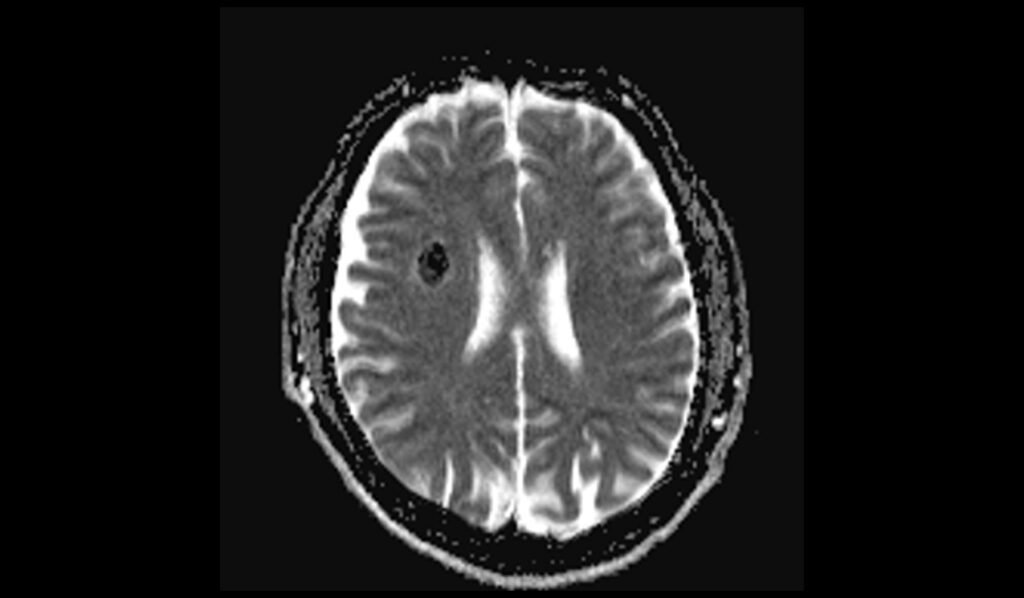
MRI DWI and ADC Appearance of Cavernoma
Diffusion-weighted imaging (DWI) and apparent diffusion coefficient (ADC) maps can provide additional insights into cavernomas, especially when hemorrhage is present. Cavernomas with acute hemorrhage may show mixed signal intensities on DWI, with hyperintense signals indicating restricted diffusion in fresh blood clots and hypointense areas due to chronic hemosiderin deposition. On ADC maps, areas corresponding to acute hemorrhage may show low ADC values (restricted diffusion), while chronic components display high ADC values (increased diffusion). The mixed signal intensity on DWI and varied ADC values help in identifying the hemorrhagic nature of the lesion.
MRI T1 Post-Contrast Appearance of Cavernoma
After the administration of contrast, T1-weighted MRI of a cavernoma may show no significant enhancement or only minimal peripheral enhancement. This lack of substantial enhancement is due to the absence of a blood-brain barrier in the cavernoma’s central core. However, peripheral enhancement may occasionally be seen, indicating associated vascular structures or reactive changes in the surrounding brain tissue. The primary diagnostic features remain the lesion’s heterogeneous signal intensity and hemosiderin rim rather than enhancement patterns.
T2 axial image shows cavernoma
FLAIR axial image shows Cavernoma
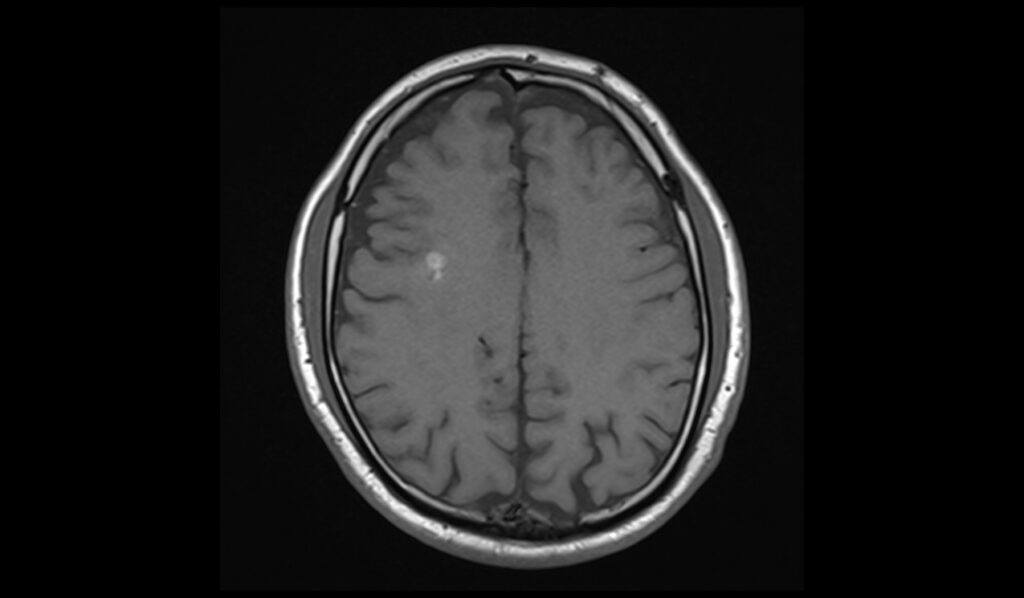
T1 axial images shows Cavernoma

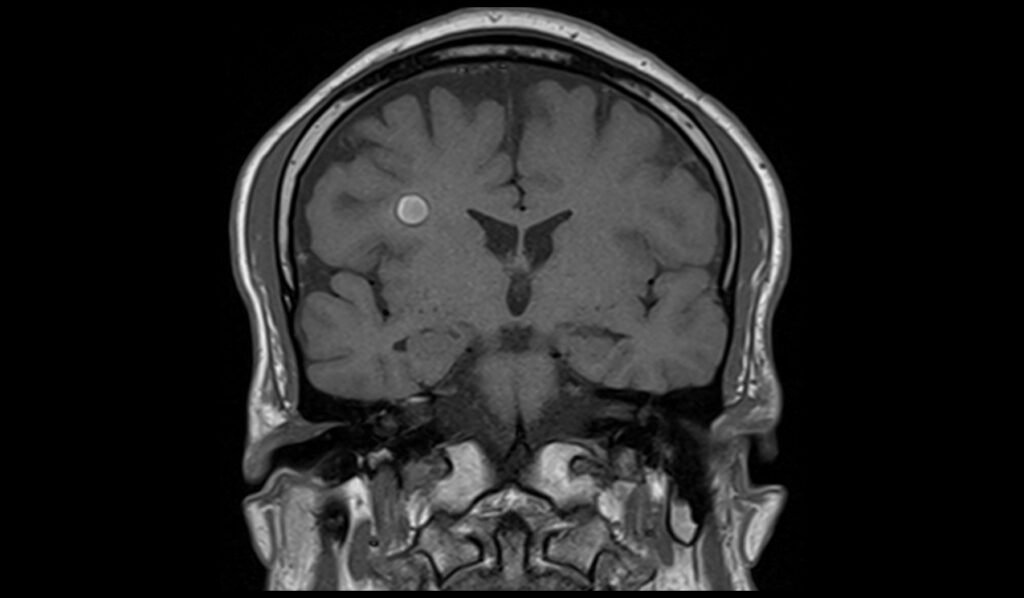
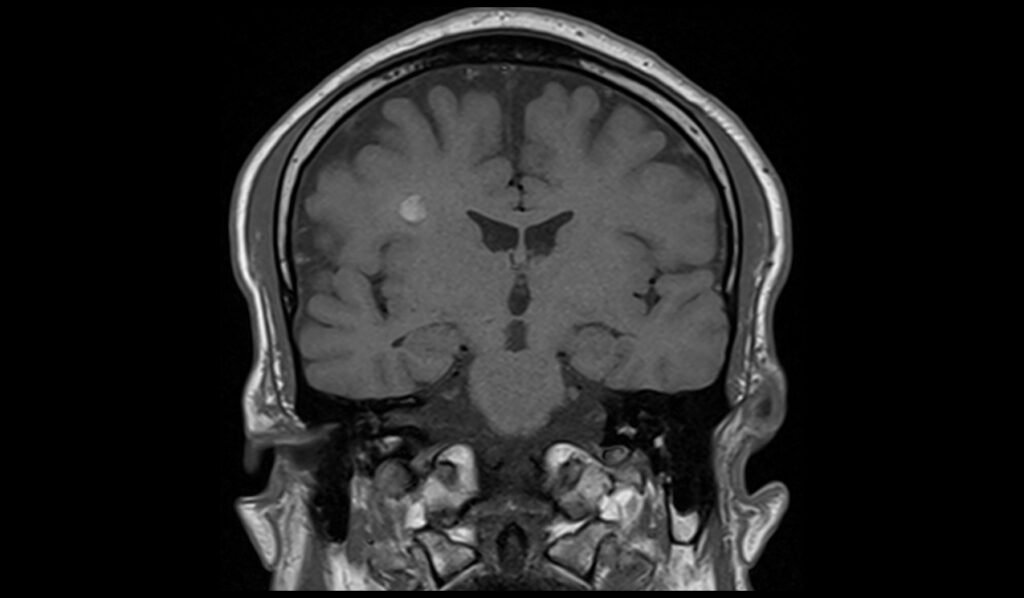
T1 coronal images shows Cavernoma
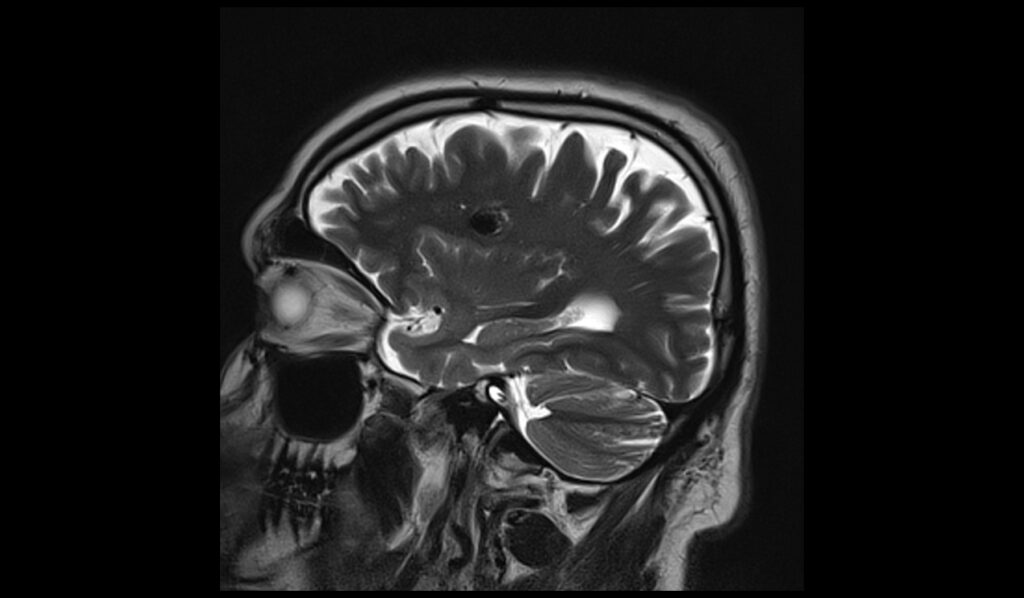
T2 sagittal images shows Cavernoma
T2* axial images shows Cavernoma

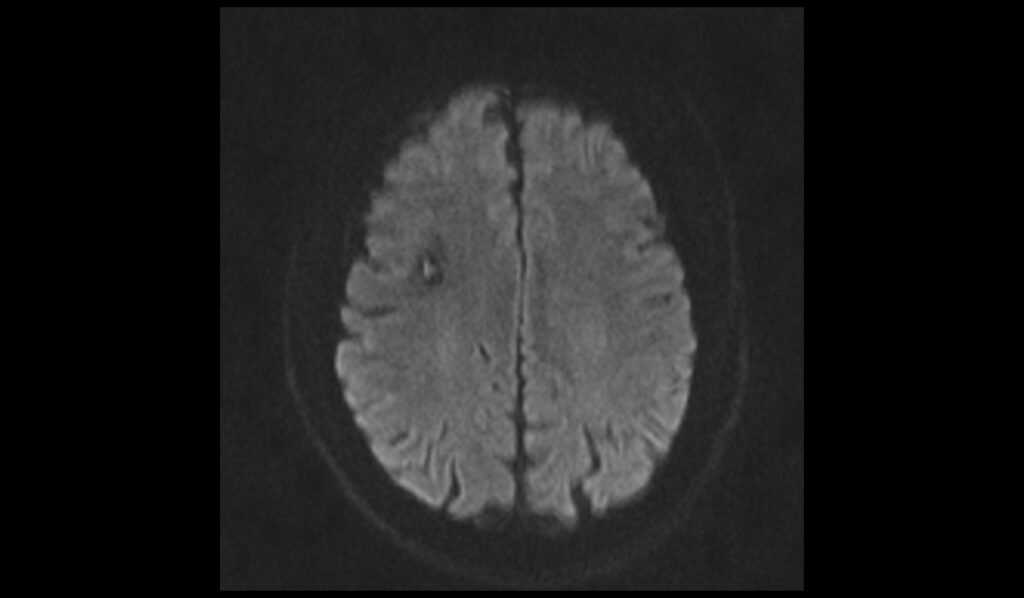
DWI b0 images shows Cavernoma
DWI b500 images shows Cavernoma

DWI b1000 images shows Cavernoma
DWI ADC images shows Cavernoma
References
- Kuroedov, D., Cunha, B., Pamplona, J., Castillo, M., & Ramalho, J. (2022). Cerebral cavernous malformations: Typical and atypical imaging characteristics. Journal of Neuroimaging, 32(6), 1013-1025. https://doi.org/10.1111/jon.13072
- Caton, M. T., & Shenoy, V. S. (2023). Cerebral Cavernous Malformations. In StatPearls [Internet]. StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538177/
- Lakhani, D. A., & Middlebrooks, E. H. (2023). T2*-weighted 7-T Imaging of Cerebral Cavernous Malformations. Radiology, 308(2). Published online August 8, 2023. https://doi.org/10.1148/radiol.230856
- Lehnhardt, F.-G., von Smekal, U., Rückriem, B., Stenzel, W., Neveling, M., Heiss, W.-D., & Jacobs, A. H. (2005). Value of Gradient-Echo Magnetic Resonance Imaging in the Diagnosis of Familial Cerebral Cavernous Malformation. Archives of Neurology, 62(4), 653-658. https://doi.org/10.1001/archneur.62.4.653


