Multiple sclerosis (MS) MRI
Multiple sclerosis (MS) is a chronic autoimmune disease that affects the central nervous system (CNS), specifically the brain and spinal cord. In MS, the immune system mistakenly attacks the protective covering of nerve fibers, called myelin, causing inflammation and damage. This damage disrupts the transmission of electrical signals between the brain and the rest of the body, resulting in a variety of neurological symptoms.
Causes
The exact cause of MS is unknown, but it is believed to result from a combination of genetic and environmental factors. Key factors that may contribute to the development of MS include:
- Genetic Susceptibility: Certain genes may increase the risk of developing MS, though no specific gene has been identified as the cause.
- Immune System Dysfunction: MS is considered an autoimmune disease where the body’s immune system attacks its own tissues.
- Environmental Triggers: Factors such as low vitamin D levels, smoking, and viral infections (e.g., Epstein-Barr virus) have been associated with an increased risk of MS.
Symptoms
MS symptoms vary widely depending on the location and severity of the nerve damage. Common symptoms include:
- Fatigue: A persistent sense of tiredness that is not alleviated by rest.
- Numbness or Tingling: Often occurs in the face, arms, legs, and fingers.
- Muscle Weakness: Particularly in the legs, which can affect mobility.
- Difficulty Walking: Problems with balance and coordination.
- Vision Problems: Blurred or double vision, partial or complete loss of vision (usually in one eye at a time), and pain during eye movement.
- Spasticity: Muscle stiffness and spasms.
- Pain: Acute or chronic pain, which can vary in intensity and duration.
- Cognitive Changes: Issues with memory, attention, and problem-solving skills.
- Bladder and Bowel Dysfunction: Urgency, frequency, or incontinence.
Diagnosis
Diagnosing MS can be challenging due to the variability of symptoms and their overlap with other conditions. A comprehensive evaluation typically involves:
- Medical History and Neurological Examination: Assessing symptoms, reflexes, coordination, balance, and other neurological functions.
- Magnetic Resonance Imaging (MRI): Detects lesions in the brain and spinal cord.
- Lumbar Puncture (Spinal Tap): Analyzes cerebrospinal fluid for signs of inflammation and specific proteins associated with MS.
Treatment
There is no cure for MS, but several treatments can help manage symptoms, modify the course of the disease, and improve quality of life:
- Disease-Modifying Therapies (DMTs): Medications designed to reduce the frequency and severity of relapses and slow disease progression. Examples include interferon beta, glatiramer acetate, and newer oral or infusion medications like fingolimod, dimethyl fumarate, and ocrelizumab.
- Corticosteroids: Used to reduce inflammation and manage acute relapses.
- Symptom Management: Medications and therapies to address specific symptoms such as pain, spasticity, fatigue, and bladder dysfunction. Physical therapy and occupational therapy can also help maintain mobility and function.
- Lifestyle Modifications: Regular exercise, a healthy diet, stress management, and avoiding smoking can improve overall health and potentially slow disease progression.
MRI appearance of Multiple sclerosis (MS)
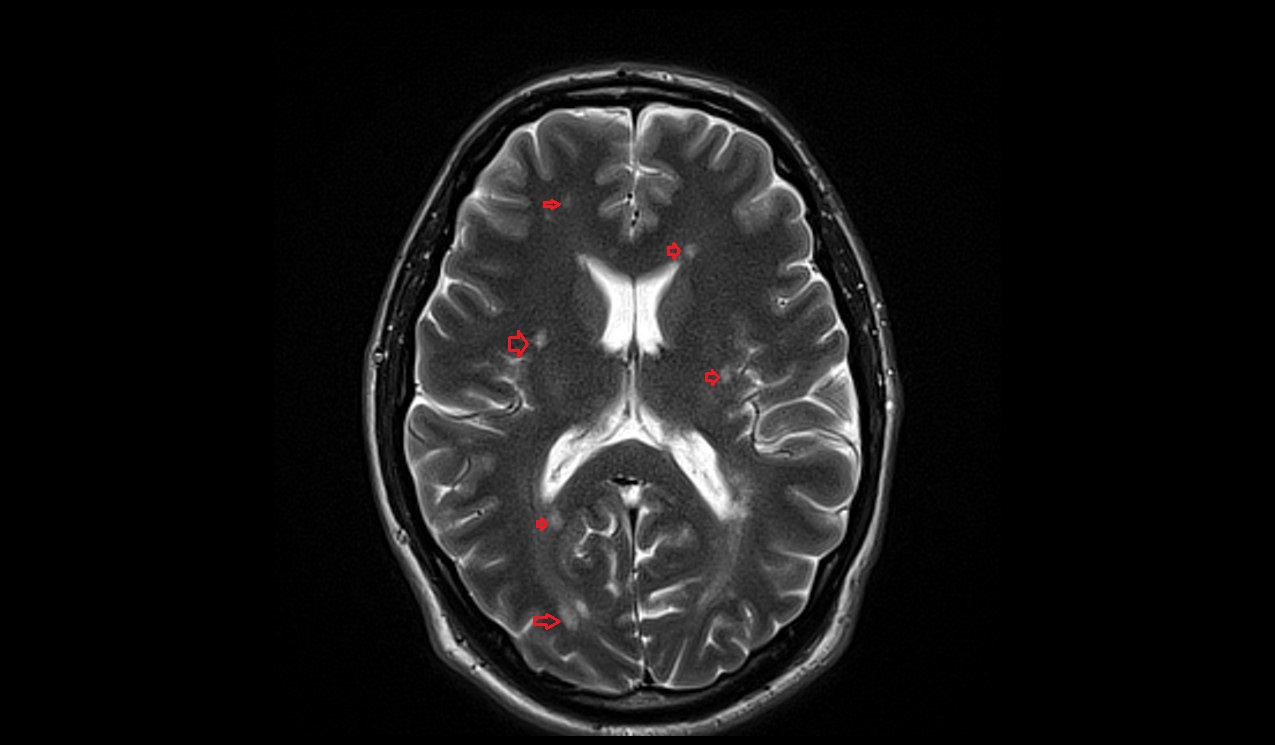
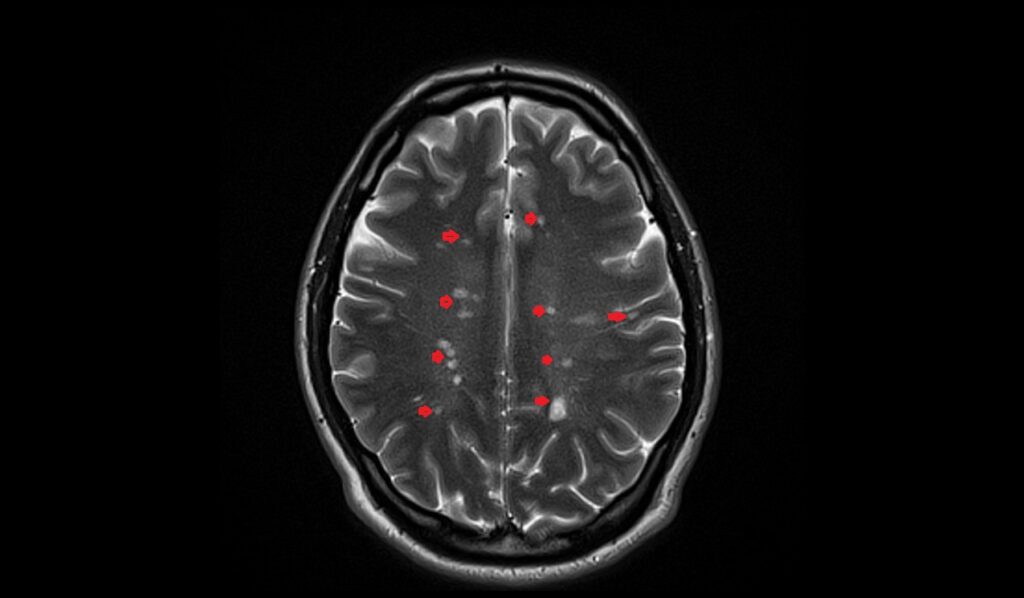
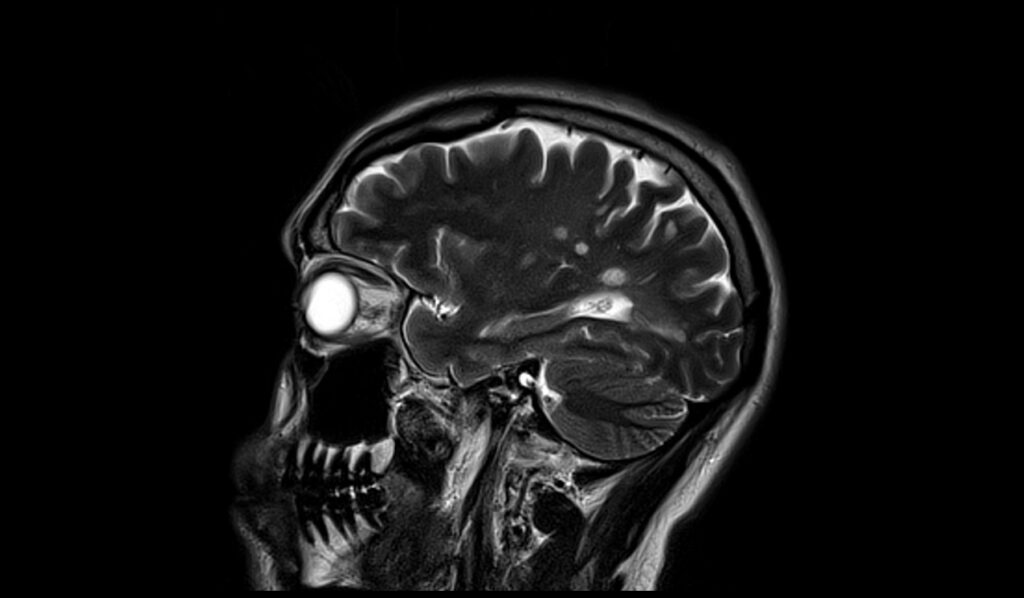
MRI T2 Appearance of Multiple Sclerosis (MS)
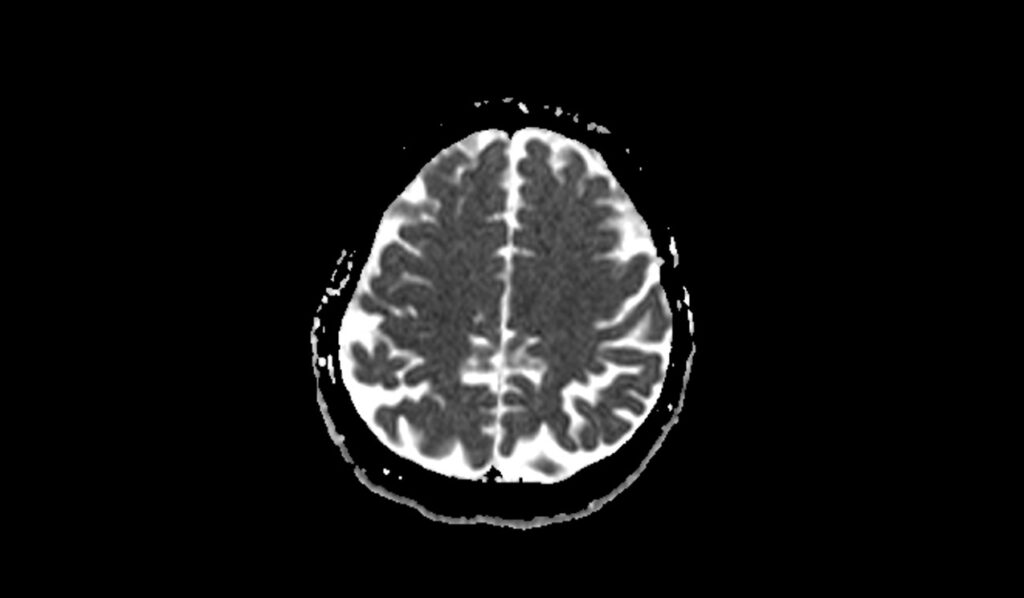
T2-weighted MRI images are highly sensitive to changes in water content and are effective in detecting MS lesions. In T2 imaging, MS lesions typically appear as hyperintense (bright) areas within the white matter of the brain and spinal cord. These bright spots represent areas of demyelination and inflammation. T2-weighted imaging is useful for identifying both acute and chronic lesions, and it is particularly valuable for assessing the burden of disease and monitoring lesion load over time. Lesions are commonly found in periventricular, juxtacortical, infratentorial, and spinal cord regions.
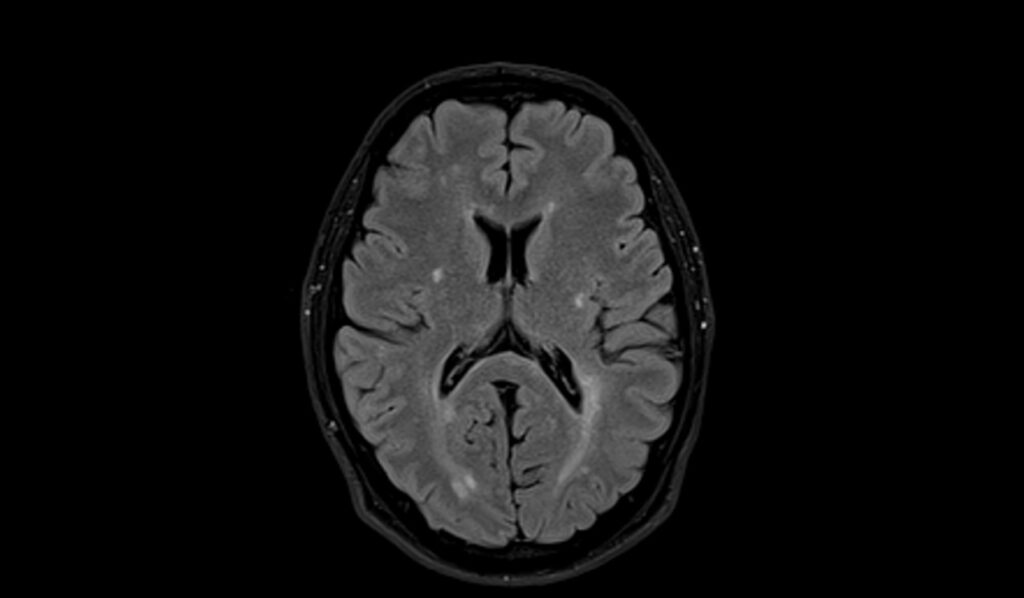
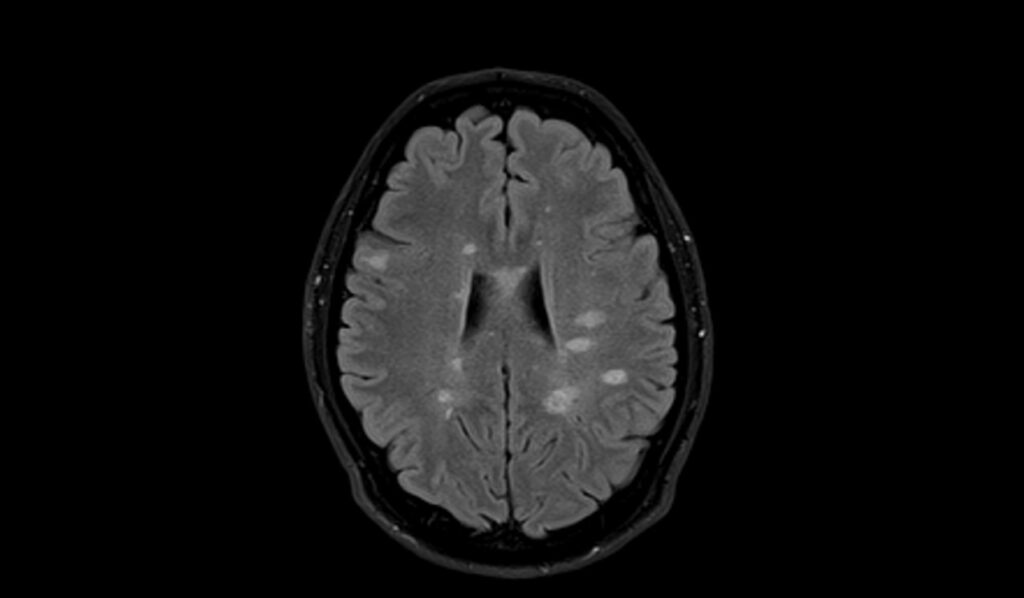
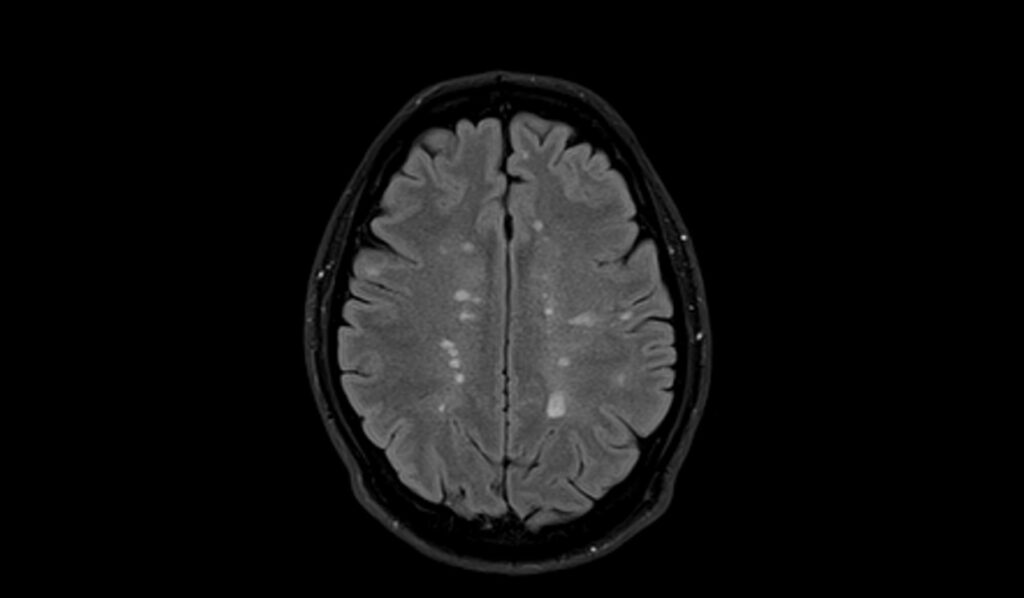
MRI FLAIR Appearance of Multiple Sclerosis (MS)
Fluid-attenuated inversion recovery (FLAIR) MRI sequences are particularly useful in visualizing MS lesions, as they suppress the signal from cerebrospinal fluid (CSF), enhancing the visibility of lesions near the ventricles. In FLAIR imaging, MS lesions appear as hyperintense (bright) areas, similar to T2-weighted images, but with better contrast against the surrounding brain tissue. This makes FLAIR sequences especially effective for detecting periventricular and cortical lesions, which are hallmark locations for MS plaques. FLAIR imaging is essential for diagnosing MS and differentiating it from other neurological conditions.
MRI DWI b0, b1000, and ADC Appearance of Multiple Sclerosis (MS)
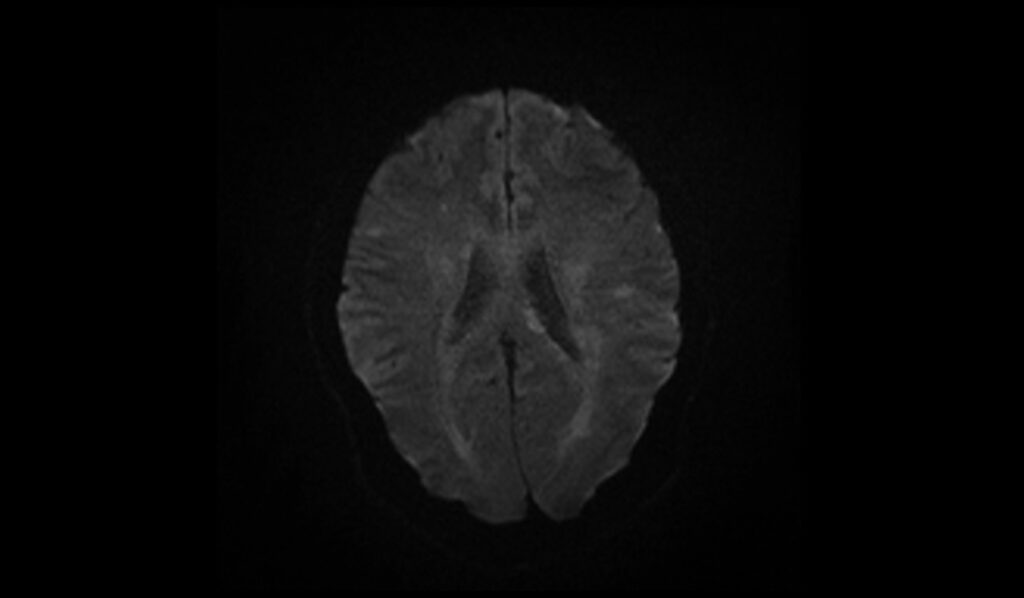
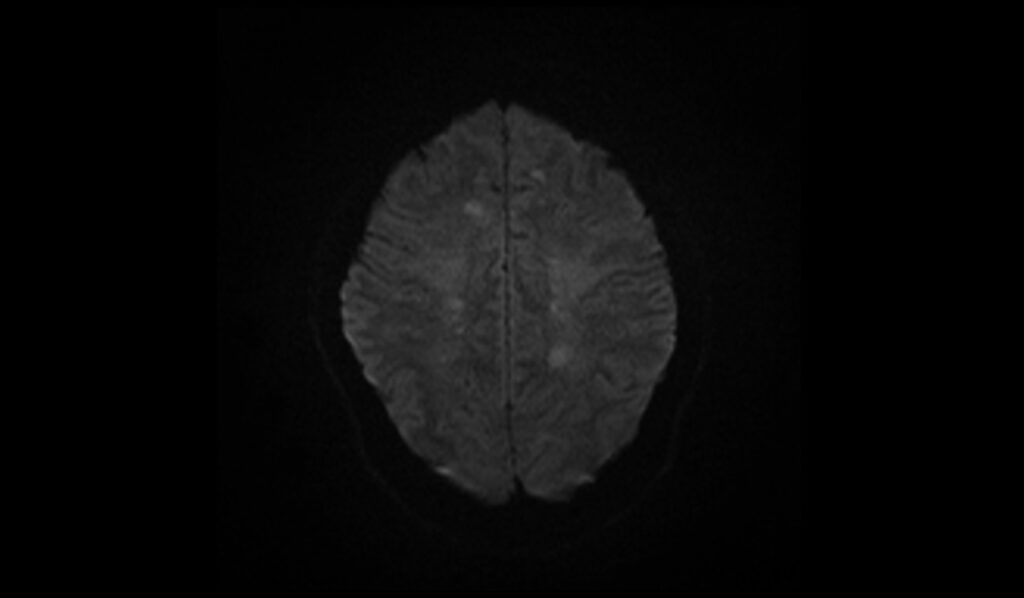
Diffusion-weighted imaging (DWI) and apparent diffusion coefficient (ADC) maps provide insights into the cellular environment and water diffusion within tissues. In DWI b0 images, which are similar to T2-weighted images, MS lesions appear hyperintense (bright). At b1000, diffusion-weighted images show acute MS lesions as hyperintense due to restricted diffusion from inflammation and cytotoxic edema. ADC maps help differentiate these lesions, as acute lesions often show low ADC values (indicating restricted diffusion), while chronic lesions may show normal or high ADC values, reflecting tissue repair or gliosis. DWI and ADC are valuable for identifying acute inflammatory activity in MS and assessing lesion evolution.
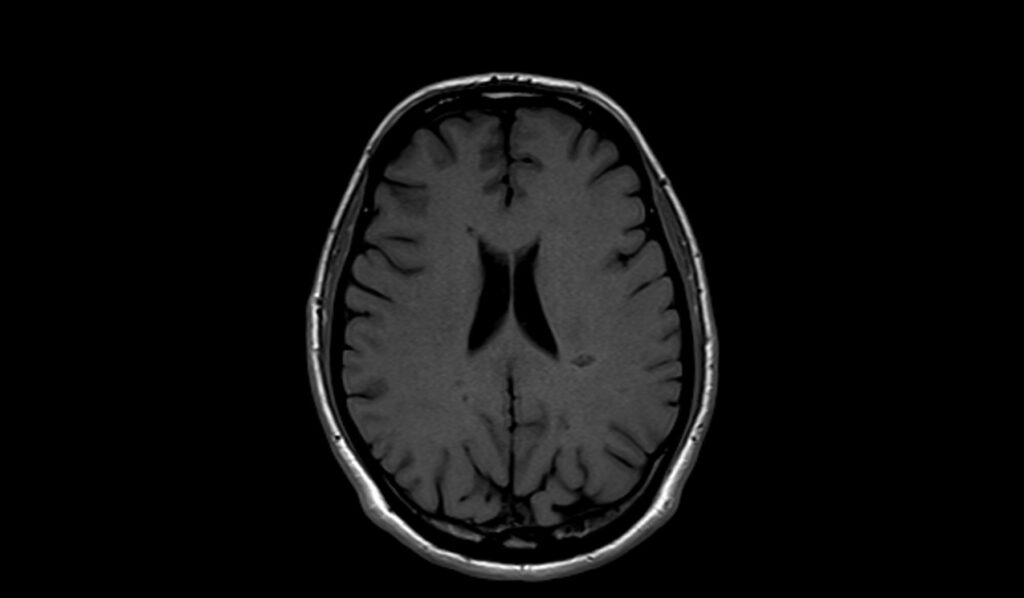
MRI T1 Appearance of Multiple Sclerosis (MS)
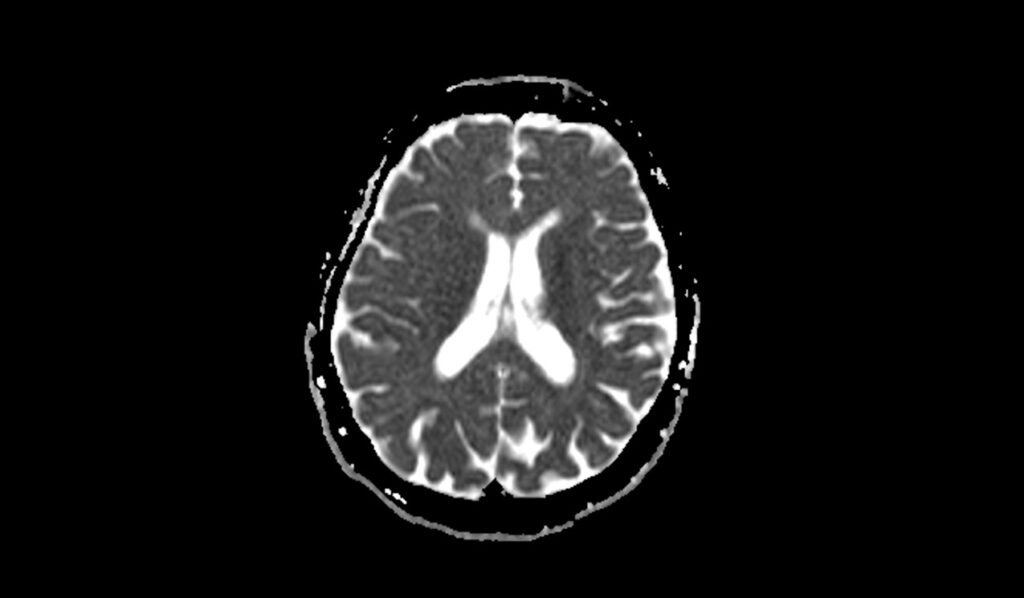
On T1-weighted MRI images, multiple sclerosis (MS) lesions typically appear as hypointense (dark) areas within the brain and spinal cord. These lesions, known as “black holes,” indicate chronic, severe tissue damage and axonal loss. They are most often seen in the periventricular white matter, corpus callosum, and spinal cord. The hypointensity on T1 images is indicative of more advanced disease and poorer prognosis, as it reflects permanent tissue destruction and gliosis. T1-weighted imaging is crucial for identifying the extent of irreversible damage caused by MS.
MRI T1 Post-Contrast Appearance of Multiple Sclerosis (MS)
Post-contrast T1-weighted MRI images are used to identify active MS lesions by highlighting areas of blood-brain barrier disruption. After administering gadolinium-based contrast agents, active MS lesions appear as hyperintense (bright) areas due to contrast enhancement. These enhancing lesions indicate ongoing inflammation and active demyelination. The presence of contrast-enhancing lesions is a marker of disease activity and is critical for diagnosing active MS, monitoring treatment response, and assessing disease progression. Non-enhancing lesions, on the other hand, reflect chronic, inactive plaques.
T2 axial images shows Multiple Sclerosis (MS)

FLAIR axial image shows Multiple Sclerosis (MS)
T1 axial image shows Multiple Sclerosis (MS)


T2 sagittal image shows Multiple Sclerosis (MS)
DWI b0 image shows Multiple Sclerosis (MS)
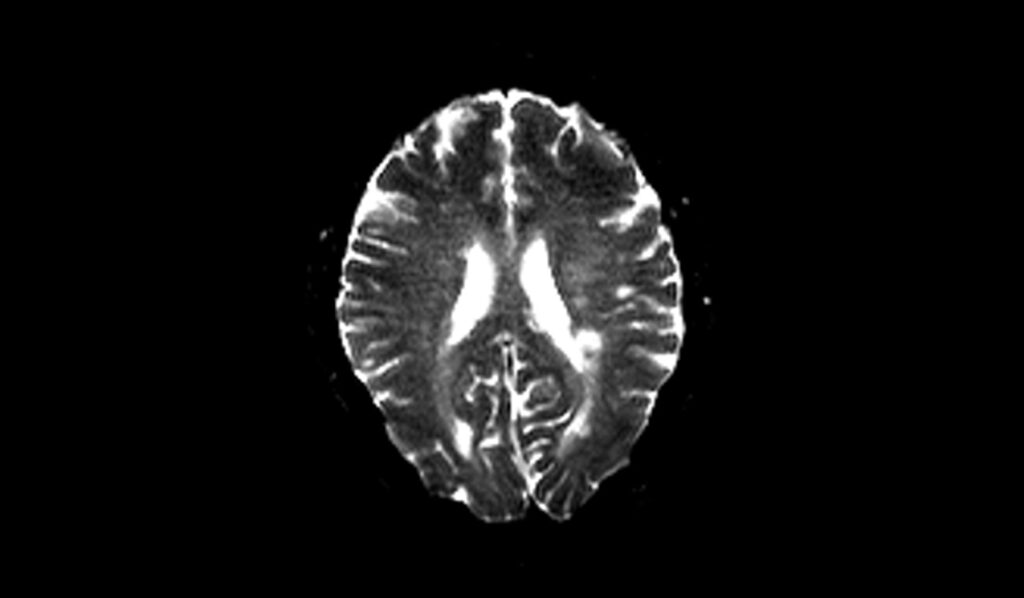

DWI b1000 image shows Multiple Sclerosis (MS)
DWI ADC map image shows Multiple Sclerosis (MS)
References
- Filippi, M., Rocca, M. A., Ciccarelli, O., De Stefano, N., Evangelou, N., Kappos, L., Rovira, A., Sastre-Garriga, J., Tintorè, M., Frederiksen, J. L., Gasperini, C., Palace, J., Reich, D. S., Banwell, B., Montalban, X., & Barkhof, F. (2016). MRI criteria for the diagnosis of multiple sclerosis: MAGNIMS consensus guidelines. Lancet Neurology, 15(3), 292–303. https://doi.org/10.1016/S1474-4422(15)00393-2
- Hemond, C. C., & Bakshi, R. (2018). Magnetic resonance imaging in multiple sclerosis. Cold Spring Harbor Perspectives in Medicine, 8(5), a028969. https://doi.org/10.1101/cshperspect.a028969
- Tomassini, V., Sinclair, A., Sawlani, V., Overell, J., Pearson, O. R., Hall, J., & Guadagno, J. (2020). Diagnosis and management of multiple sclerosis: MRI in clinical practice. Journal of Neurology, 267(10), 2917–2925.
- Filippi, M., Rocca, M. A., De Stefano, N., Enzinger, C., Fisher, E., Horsfield, M. A., Inglese, M., Pelletier, D., & Comi, G. (2011). Magnetic Resonance Techniques in Multiple Sclerosis: The Present and the Future. Archives of Neurology, 68(12), 1514-1520.
- Khoury, S. J., & Weiner, H. L. (1998). Multiple sclerosis: What have we learned from magnetic resonance imaging studies? Archives of Internal Medicine, 158(6), 565-573. https://doi.org/10.1001/archinte.158.6.565


