MRI Late Subacute Hemorrhage
A late subacute hemorrhage refers to a stage of bleeding, particularly observed in brain injuries, that occurs approximately 7 to 14 days after the initial incident. This stage is part of the healing process where blood initially turns from oxyhemoglobin to deoxyhemoglobin and then to methemoglobin, which can be seen in imaging studies.
Grading of Hemorrhages:
Hemorrhages can be classified based on the timing of their occurrence post-injury and their appearance on imaging:
- Hyperacute (first few hours): Fresh bleeding, where blood is primarily oxyhemoglobin. On MRI, hyperacute hemorrhage typically appears isointense to slightly hyperintense on T1-weighted images and isointense to hyperintense on T2-weighted images.
- Acute (within 1-3 days): Blood converts to deoxyhemoglobin, seen as hypointense to isointense on T1-weighted images and hypointense on T2-weighted images.
- Early Subacute (3-7 days): The presence of intracellular methemoglobin begins and appears bright on T1 MRI images.
- Late Subacute (7-14 days): Intracellular methemoglobin is more prominent and appears hyperintense on both T1-weighted and T2-weighted images
- Chronic (after 2 weeks): Hemoglobin breakdown continues to hemosiderin, with the hemorrhage appearing darker on both T1 scans.
Symptoms of Hemorrhage
The symptoms of a hemorrhage depend largely on the hemorrhage’s location and size but may include:
- Headache
- Nausea or vomiting
- Increased intracranial pressure
- Neurological deficits such as weakness, numbness, or decreased coordination
- Seizures in some cases
- Altered consciousness or confusion
Diagnosis of Late Subacute Hemorrhage
Diagnosis typically involves imaging techniques that can track the progression of blood breakdown products over time:
- MRI: Most effective for identifying the stage of hemorrhage due to its ability to distinguish between different blood breakdown products.
- CT Scan: Useful for initially identifying hemorrhage and assessing its size and potential effects on surrounding structures.
Treatment
Treatment of late subacute hemorrhage focuses on managing symptoms, preventing complications, and addressing the underlying cause:
Observation: Close monitoring of the patient’s neurological status and repeat imaging to assess the resolution of the hemorrhage.
Medication:
- Antihypertensives: To control blood pressure and prevent further bleeding.
- Anticonvulsants: To manage or prevent seizures.
- Pain Management: Analgesics for headache relief.
Surgery: In some cases, surgical intervention may be necessary to evacuate the hematoma, particularly if there is significant mass effect or if the patient’s condition deteriorates.
Addressing Underlying Causes: Identifying and treating the source of the hemorrhage (e.g., aneurysm, arteriovenous malformation, or anticoagulant therapy) to prevent recurrence.
MRI appearance of late subacute hemorrhage
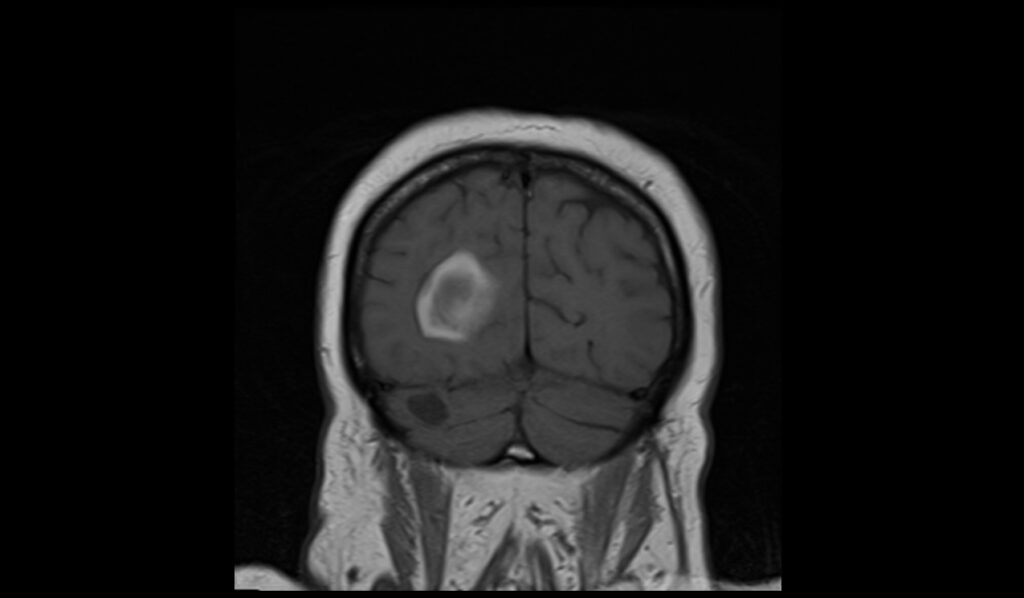
T1-Weighted Imaging
In the late subacute phase of hemorrhage, T1-weighted MRI images typically exhibit a hyperintense signal. This appearance is due to the presence of methemoglobin, which forms as the blood ages and transitions from oxyhemoglobin and deoxyhemoglobin. The bright or hyperintense signal on T1 reflects the high concentration of methemoglobin, particularly in the extracellular space, making these regions standout against the lower-intensity brain tissue.
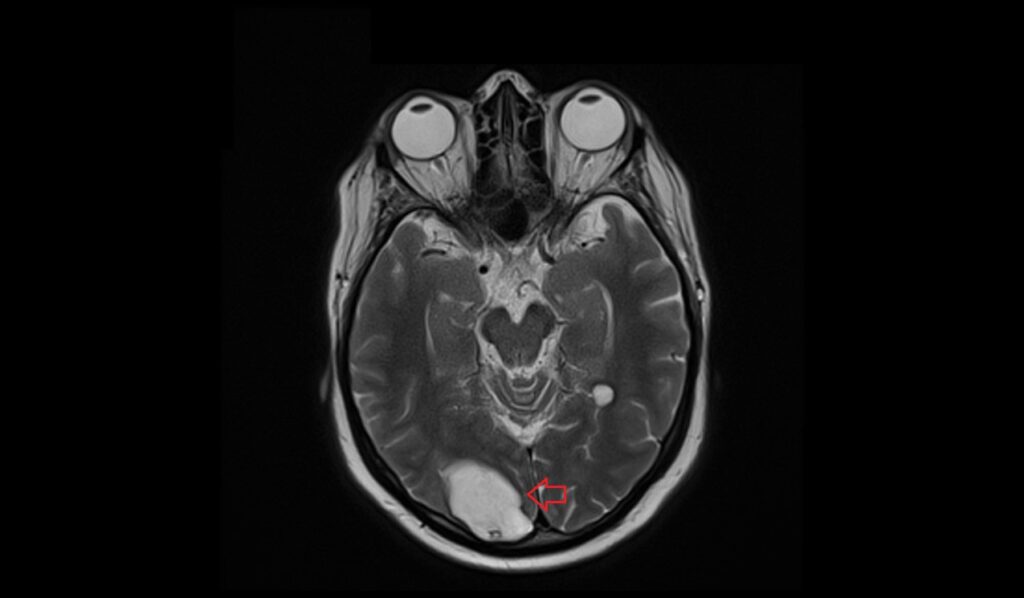
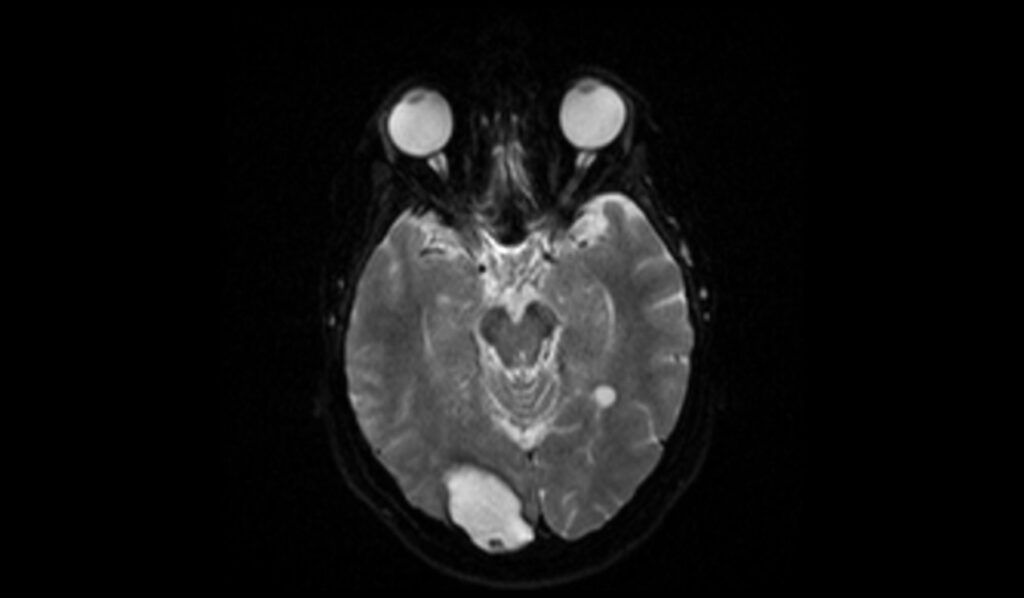
T2-Weighted Imaging
T2-weighted imaging of late subacute hemorrhage shows a heterogeneous appearance. The core of the hemorrhage is usually hyperintense, reflecting the paramagnetic effects of methemoglobin, surrounded by a hypointense rim due to hemosiderin deposition and the presence of deoxyhemoglobin in surrounding tissues. This mixed signal intensity is characteristic of the evolving nature of the hematoma.
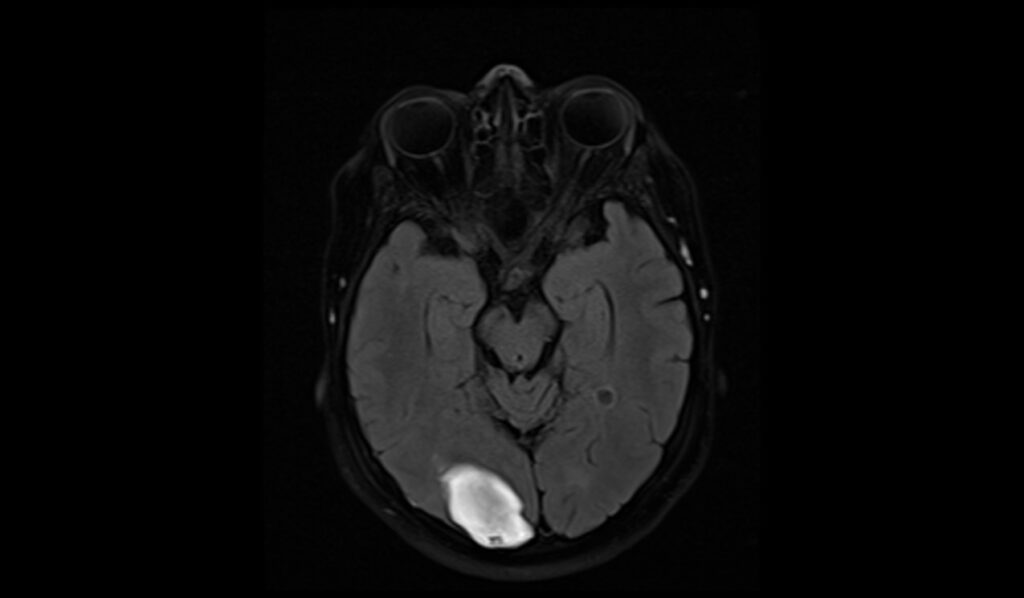
FLAIR (Fluid-Attenuated Inversion Recovery) Imaging
FLAIR imaging of late subacute hemorrhage shows mixed signal characteristics. The core of the hematoma may appear hyperintense due to methemoglobin, similar to T2-weighted imaging, but the surrounding edema and gliosis can also be hyperintense. The periphery of the lesion may have a hypointense rim, reflecting hemosiderin deposition and chronic blood product residue
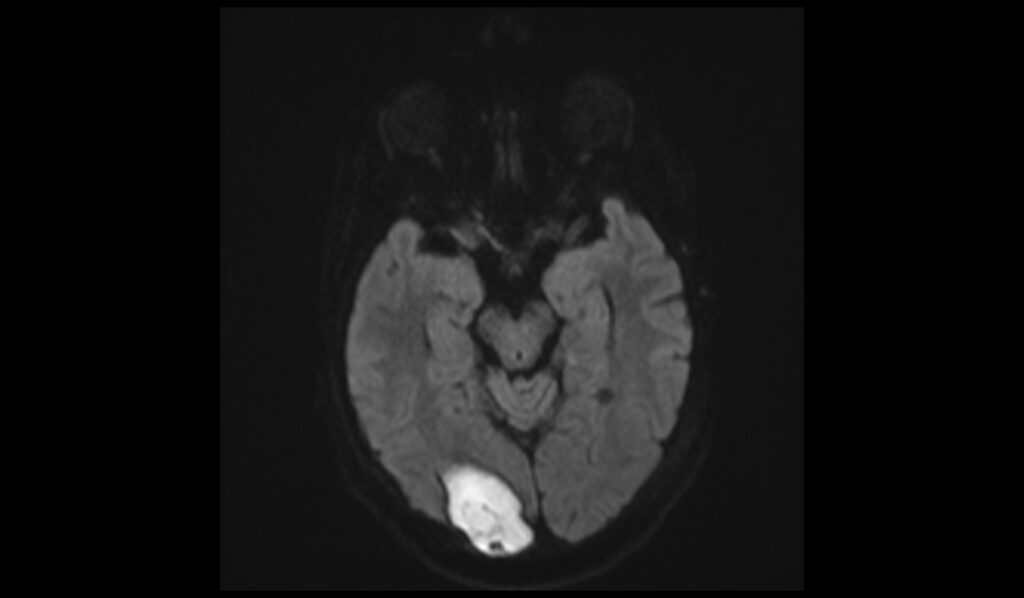
DWI b0 and b1000 Imaging
On diffusion-weighted imaging (DWI), the b0 images of late subacute hemorrhage usually show mixed signal intensity due to the varying magnetic properties of blood breakdown products and surrounding edema. At higher b-values, such as b1000, the hemorrhage might demonstrate restricted diffusion with a relatively hyperintense signal, reflecting the restricted movement of water molecules within the clot, although this can vary depending on the exact timing and characteristics of the hemorrhage.
ADC map Appearance
Apparent diffusion coefficient (ADC) maps typically show low ADC values within the hemorrhagic region during the late subacute phase, indicating restricted diffusion.
T2 axial image shows late subacute hemorrhage
FLAIR axial image shows late subacute hemorrhage
T1 coronal image shows late subacute hemorrhage
T2 sagittal image shows late subacute hemorrhage

DWI b0 image shows late subacute hemorrhage
DWI b1000 image shows late subacute hemorrhage
DWI ADC map image shows late subacute hemorrhage

References
- Chen, X., Li, Y., Guo, S., Han, X., Liu, R., Tian, C., Cui, R., Dong, Z., & Yu, S. (2022). Diffusion-weighted imaging hyperintensities during the chronic stage of intracerebral hemorrhage with surgery: A new clinical situation or post-surgery artifact? Frontiers in Neurology, 13, 948828.
- Grossman, R. I., Gomori, J. M., Goldberg, H. I., Hackney, D. B., Atlas, S. W., Kemp, S. S., Zimmerman, R. A., & Bilaniuk, L. T. (1988). MR imaging of hemorrhagic conditions of the head and neck. Radiographics, 8(3), 441-454.


