MRI Intracranial tuberculoma
Intracranial tuberculoma is a form of tuberculosis that affects the brain. It involves the formation of one or more mass-like lesions or tubercles within the cranial cavity. These lesions result from the infection caused by the bacterium Mycobacterium tuberculosis. Intracranial tuberculomas are part of a broader category of tuberculosis infections that can affect various parts of the body outside the lungs, known as extrapulmonary tuberculosis.
Causes
The primary cause of intracranial tuberculoma is the spread of Mycobacterium tuberculosis bacteria from another infected site in the body, typically the lungs, to the brain. This spread usually occurs through the bloodstream. Factors that may increase the risk include weakened immune systems, such as in individuals with HIV/AIDS, diabetes, or those taking immunosuppressive medications.
Symptoms
The symptoms of intracranial tuberculoma can vary depending on the location and size of the lesions. Common symptoms include:
- Headaches
- Seizures
- Neurological deficits (such as weakness or sensory losses in certain parts of the body)
- Behavioral changes or confusion
- Nausea and vomiting
- Fever and night sweats (general signs of infection)
Diagnosis
Diagnosing intracranial tuberculoma involves a combination of clinical evaluation, imaging studies, and laboratory tests:
- Imaging Studies: Magnetic Resonance Imaging (MRI) and Computed Tomography (CT) scans are commonly used to detect lesions in the brain. These imaging modalities can help differentiate tuberculomas from other types of brain tumors or lesions.
- Laboratory Tests: Tests such as cerebrospinal fluid (CSF) analysis, which may include PCR for tuberculosis, cultures, and sensitivity tests. Blood tests can also detect markers of infection and inflammation.
- Biopsy: In some cases, a biopsy of the lesion may be performed to confirm the diagnosis by directly observing the tuberculosis bacteria.
Treatment
The treatment of intracranial tuberculoma generally involves a long-term course of antibiotics to eradicate the tuberculosis infection. The typical regimen includes:
- Antituberculous Therapy (ATT): A combination of drugs such as isoniazid, rifampicin, ethambutol, and pyrazinamide, taken for a minimum of 6-12 months.
- Corticosteroids: May be used to reduce inflammation and edema around the lesions, particularly if they are causing significant pressure or symptoms.
- Surgery: Although less common, surgical intervention might be required if there is a need to relieve intracranial pressure, if the lesions are large or if the response to medical treatment is inadequate.
MRI appearance of Intracranial tuberculoma
MRI T1
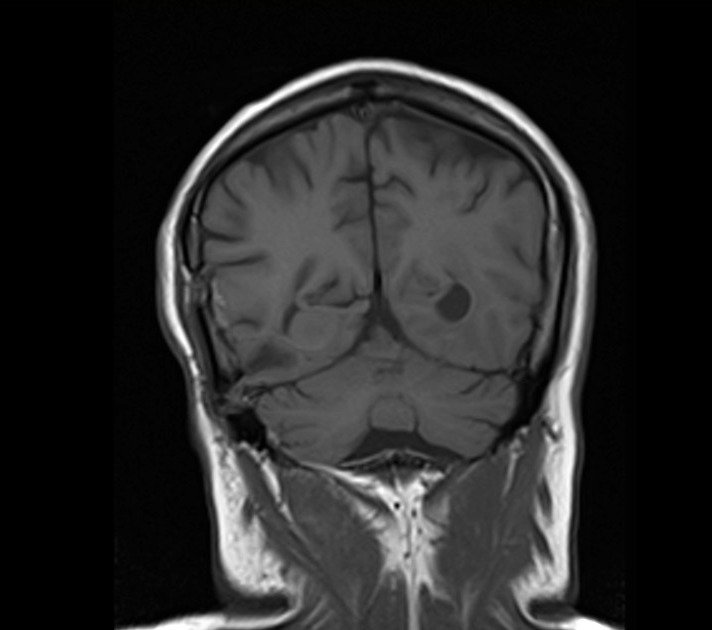
- On T1-weighted images, intracranial tuberculomas generally appear as hypointense (dark) lesions compared to the surrounding brain tissue. This is primarily due to the solid, caseating nature of the tuberculomas which have low proton density.
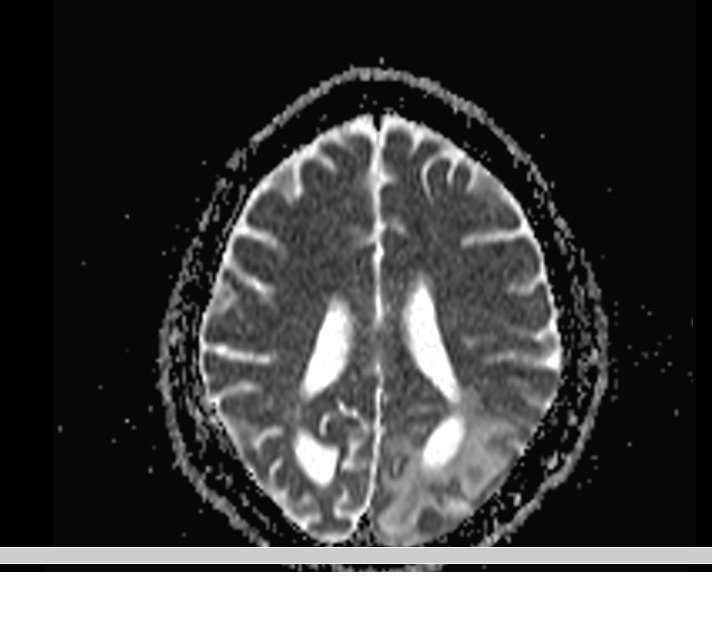
MRI T2
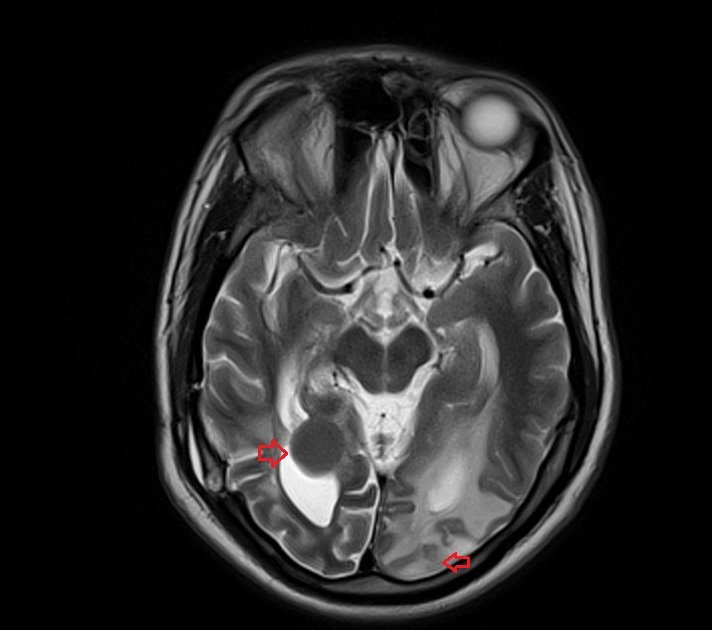
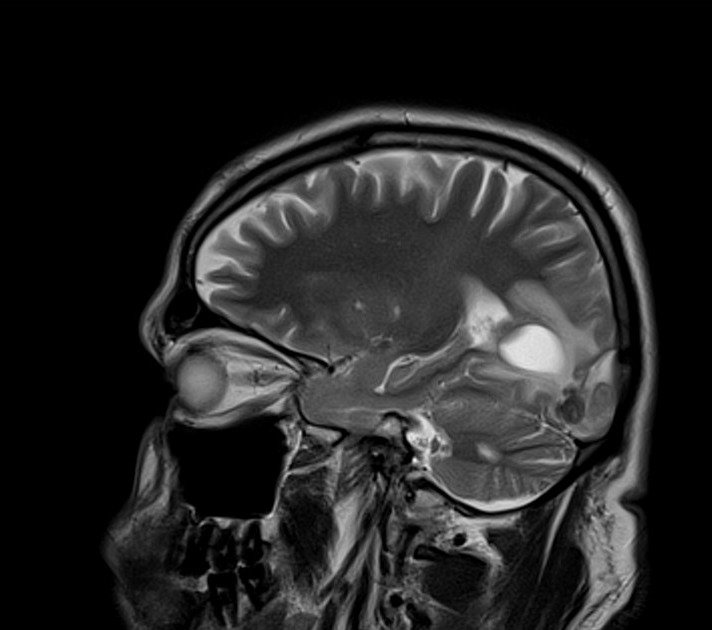
- On T2-weighted images, the appearance can be more variable. Often, the center of the tuberculoma appears hypointense due to the presence of caseous material, while the surrounding edema may show hyperintensity (bright). This creates a characteristic “bull’s-eye” appearance, which is typical but not exclusive to tuberculomas.
FLAIR (Fluid-Attenuated Inversion Recovery)
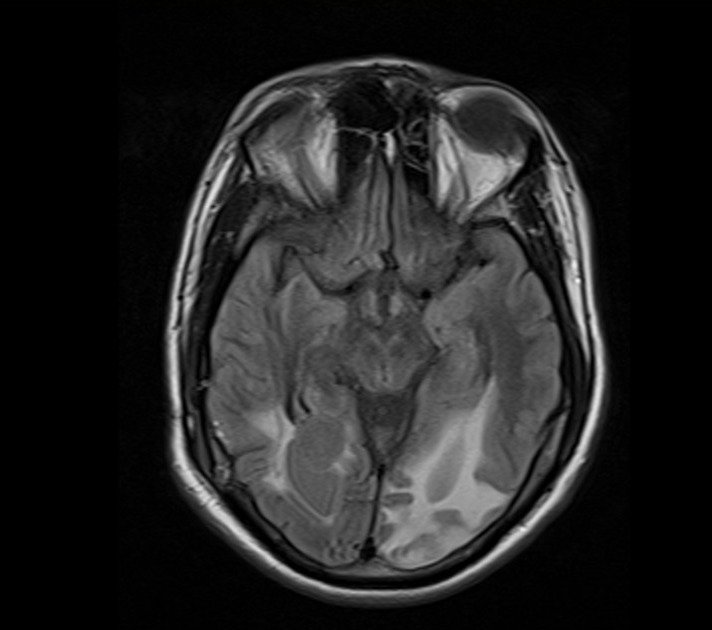
- Fluid-attenuated inversion recovery (FLAIR) imaging is particularly useful for identifying perilesional edema. Tuberculomas on FLAIR images appear as hypointense or isointense lesions with a surrounding hyperintense signal due to edema. This helps in distinguishing the lesion from the surrounding inflamed tissue.
DWI (Diffusion Weighted Imaging)
- Intracranial tuberculomas usually exhibit variable diffusion restriction depending on their composition.
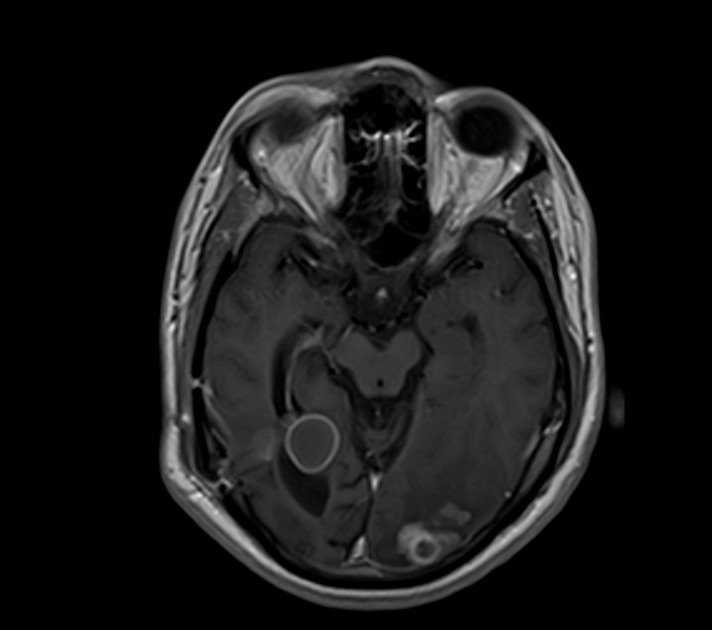
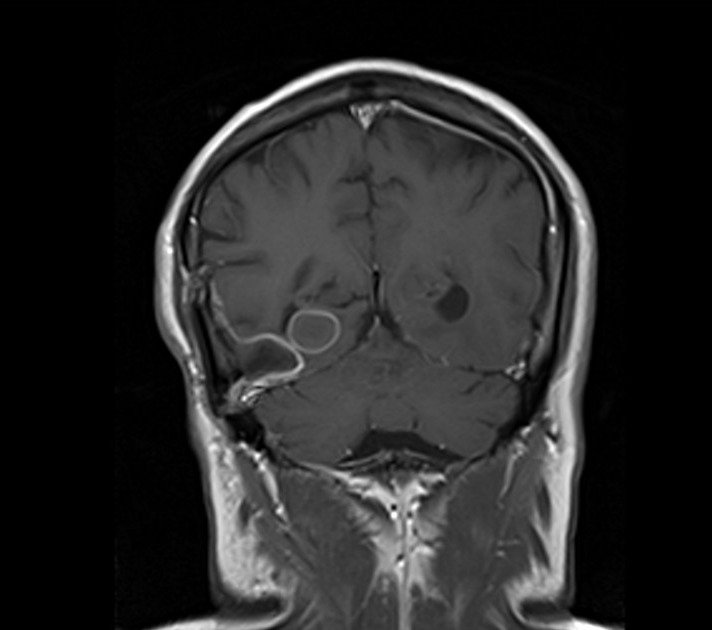
T1 Post-Contrast (Gadolinium)
- After the administration of contrast material, intracranial tuberculomas usually show a ring or nodular enhancement pattern. The “ring enhancement” is due to the presence of an enhancing capsule that forms around the necrotic caseous material in the center of the tuberculoma. This peripheral enhancement is a key diagnostic feature, indicating the vascular response to the infection.
T2 axial image shows Intracranial tuberculoma
FLAIR axial image shows Intracranial tuberculoma
T1 coronal image shows Intracranial tuberculoma
T2 sagittal image shows Intracranial tuberculoma
DWI b0 image shows Intracranial tuberculoma

DWI b1000 image shows Intracranial tuberculoma
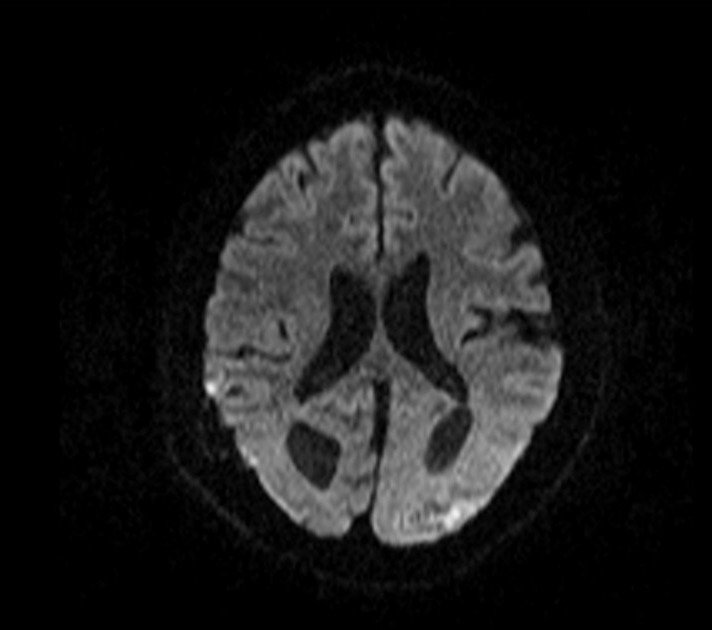
DWI ADC map image shows Intracranial tuberculoma
T1 post contrast axial image shows Intracranial tuberculoma
T1 post contrast coronal image shows Intracranial tuberculoma
References
- Ibrahim, I. G., Osman, A. A., Shikhow, M. G., Celik, C., Mutlu, E., Qalaf, M. S. H., Tahtabaşı, M., & Mohamed, Y. G. (2022). Magnetic resonance imaging findings of intracranial tuberculoma patients in a tertiary hospital in Mogadishu, Somalia: A retrospective study. Annals of Medicine and Surgery (London), 78, 103812. https://doi.org/10.1016/j.amsu.2022.103812
- Moussa, A. A., Mahmoud, M. E., & Yousef, H. A. (2018). Intracranial tuberculoma and recent advances in magnetic resonance imaging. Egyptian Journal of Neurosurgery, 33(Article 13). https://doi.org/10.1186/s41984-018-0013-2
Trivedi, R., Saksena, S., & Gupta, R. K. (2009). Magnetic resonance imaging in central nervous system tuberculosis. Indian Journal of Radiology and Imaging, 19(4), 256–265. https://doi.org/10.4103/0971-3026.57205 - Kumar, I., Shekhar, S., Yadav, T., Aggarwal, P., Singh, P.K., Shukla, R.C., & Verma, A. (2023). The many faces of intracranial tuberculosis: atypical presentations on MRI—a descriptive observational cohort study. Egyptian Journal of Radiology and Nuclear Medicine, 54(116).


