MRI Intracranial Tuberculosis
Intracranial tuberculosis is a serious, life-threatening infection of the brain caused by Mycobacterium tuberculosis, the bacteria responsible for tuberculosis (TB). It primarily affects the brain’s meninges, which are the protective layers covering the brain and spinal cord, but can also affect other parts of the central nervous system. Intracranial TB is a form of extrapulmonary tuberculosis, meaning it occurs outside of the lungs. The primary forms of intracranial TB include:
Tuberculous meningitis (TBM): It is the most common form of CNS tuberculosis and involves inflammation of the meninges, the layers that cover the brain and spinal cord.
Tuberculoma: This is a localized form of CNS tuberculosis, presenting as a granuloma or a mass in the brain or spinal cord.
Tuberculous abscess: This is a less common form, where there’s a collection of pus in the brain or spinal cord due to TB.
Tuberculous encephalopathy: A rare form with diffuse brain involvement without any evident meningitis or mass.
Symptoms of Intracranial Tuberculosis:
The symptoms of intracranial TB largely depend on the form and location of the disease, but they can include:
For Tuberculous meningitis:
- Gradual onset of symptoms
- Headache
- Fever
- Neck stiffness
- Vomiting
- Altered consciousness
- Seizures
- Cranial nerve palsies
For Tuberculoma and Tuberculous abscess:
- Focal neurological symptoms, depending on the location (like weakness in one part of the body or problems with speech)
- Seizures
- Headache
For Tuberculous encephalopathy:
- Rapidly progressing altered mental status
- Neurological deficits without other apparent causes.
Diagnosis:
A combination of clinical history, examination, and investigations like lumbar puncture, cerebrospinal fluid (CSF) analysis, imaging studies (like MRI and CT scan), and microbiological tests are used.
Treatment:
Antitubercular therapy (ATT): The cornerstone of treatment involves a combination of antitubercular drugs like isoniazid, rifampin, pyrazinamide, and ethambutol for an initial period, followed by continuation phase with isoniazid and rifampin. The exact duration and choice of drugs might vary based on the severity and the specific presentation, but treatment usually lasts for at least 12 months.
Corticosteroids: Especially for tuberculous meningitis, the use of adjunctive corticosteroids (like dexamethasone) has been shown to improve outcomes, especially in terms of reducing neurological complications.
Surgical intervention: In cases of large tuberculomas, abscesses, or hydrocephalus (increased fluid pressure in the brain), surgical procedures might be necessary.
Management of complications: Seizures, hydrocephalus, and other complications should be managed as they arise.
MRI appearance of Intracranial Tuberculosis (TB)
Intracranial Tuberculosis (TB) manifests differently in MRI sequences depending on its form and stage, such as Tuberculous Meningitis, Tuberculoma, or Abscess.
T1-Weighted Images:
In general, tuberculomas appear hypo- or isointense on T1-weighted images. Lesions may be multiple or solitary. The edema surrounding the lesion will appear hypointense.
T2-Weighted Images:
Tuberculomas can appear hypointense or iso-intense on T2-weighted images, often with a surrounding hypointense rim due to fibrosis. The edema surrounding the lesion will appear hyperintense.
FLAIR (Fluid-Attenuated Inversion Recovery):
Lesions typically appear hypointense or iso-intense on FLAIR images, aiding in the differentiation of lesions from the surrounding hyperintense edema.
DWI (Diffusion-Weighted Imaging):
Active tuberculomas and abscesses may restrict diffusion and appear hyperintense on DWI.
T1 Post-Contrast Images:
Enhancement patterns on post-contrast T1 images can be variable, ranging from ring enhancement, nodular enhancement to homogenous enhancement, especially in the case of tuberculomas and abscesses. Meningeal enhancement can be seen in tuberculous meningitis.
T2 axial image shows Intracranial Tuberculosis (TB)

FLAIR axial image shows Intracranial Tuberculosis (TB)

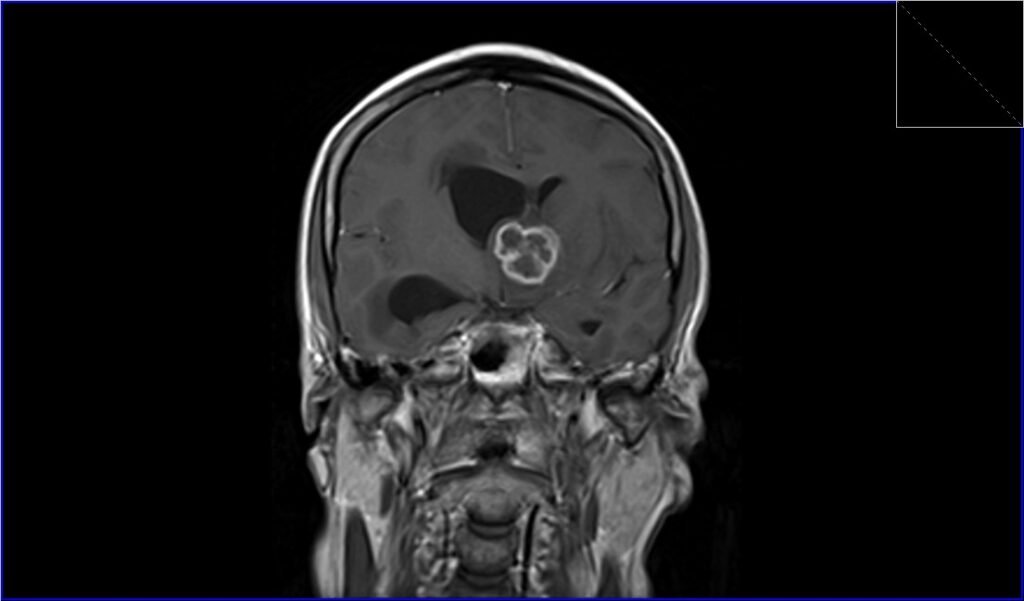
TI coronal image shows Intracranial Tuberculosis (TB)

T2 sagittal image shows Intracranial Tuberculosis (TB)

DWI b1000 axial image shows Intracranial Tuberculosis (TB)

DWI b0 axial image shows Intracranial Tuberculosis (TB)

ADC axial image shows Intracranial Tuberculosis (TB)

T1 post contrast axial image shows Intracranial Tuberculosis (TB)

T1 post contrast coronal image shows Intracranial Tuberculosis (TB)
References
Thakur K, Manoj V, Raj S, et al. (2018). MRI in CNS Tuberculosis: A Study of Two Hundred Patients. Journal of Clinical Imaging Science, 8, 48. DOI: 10.4103/jcis.JCIS_30_18
Misra UK, Kalita J, Nair PP. (1997). Role of aspirative cytology in the etiological diagnosis of tuberculous meningitis. Acta Cytologica, 41(5), 1364-1368. PMID: 9311116
Bernaerts A, Vanhoenacker FM, Parizel PM, et al. (2003). Tuberculosis of the central nervous system: overview of neuroradiological findings. European Radiology, 13(8), 1876-1890. DOI: 10.1007/s00330-003-1843-9
Gupta RK, Jena A, Sharma A, et al. (2008). Role of magnetic resonance (MR) in the diagnosis and management of intracranial tuberculomas. Clinical Neurology and Neurosurgery, 110(1), 1-6. DOI: 10.1016/j.clineuro.2007.08.018
Kashyap S, Mohapatra B, Das D, et al. (2018). Intracranial Tuberculosis: A Critical Review. Seminars in Roentgenology, 53(4), 266-280. DOI: 10.1053/j.ro.2018.08.004
Tandon PN, Kharbanda PS. (1983). Intracranial tuberculomas. Journal of Neurosurgery, 58(4), 516-522. DOI: 10.3171/jns.1983.58.4.0516
Gupta RK, Kathuria MK, Pradhan S, et al. (1999). MR imaging of intracranial tuberculosis. Acta Radiologica, 40(4), 359-365. DOI: 10.1080/02841859909172189
Kanekar SG, Mankad K, Castillo M. (2011). Imaging of Tuberculosis of the Central Nervous System. Neuroimaging Clinics of North America, 21(4), 659-677. DOI: 10.1016/j.nic.2011.06.008
Andronikou S, Wieselthaler N, Smith B, et al. (2002). CT scanning with intravenous contrast alone: the role of delayed scans in decision-making. Pediatric Radiology, 32(11), 797-802. DOI: 10.1007/s00247-002-0811-2
Bathla G, Khandelwal N, Maller VG, et al. (2010). Magnetic resonance imaging in intracranial tuberculosis. Acta Radiologica, 51(3), 305-312. DOI: 10.3109/0284185090347088
