Focal nodular hyperplasia (FNH)
Focal nodular hyperplasia (FNH) is a non-cancerous, benign liver condition characterized by the presence of a distinctive, well-defined lesion within the liver tissue. FNH is one of the most common benign liver lesions, often discovered incidentally during routine medical imaging studies.
- Appearance: FNH typically appears as a solitary, round or oval-shaped nodule within the liver. It is known for its unique imaging characteristics, which include a central scar or stellate scar at the core of the lesion. This scar gives FNH a characteristic “bull’s-eye” or “target” appearance on imaging scans.
- Origins: The lesion in FNH arises from the abnormal growth of liver cells, particularly hepatocytes, which are the main functional cells of the liver. The exact cause of FNH is not always clear, but it is believed to be related to abnormal blood flow within the liver.
- Symptoms: Many individuals with FNH are asymptomatic, meaning they do not experience any noticeable symptoms. When symptoms do occur, they are typically mild and may include vague discomfort or a feeling of fullness in the upper right abdomen. Severe pain or complications are rare.
- Diagnosis: FNH is often diagnosed incidentally when imaging studies such as ultrasound, computed tomography (CT) scans, or magnetic resonance imaging (MRI) scans are conducted for unrelated medical reasons. The presence of a characteristic central scar and a well-defined, non-invasive nature of the lesion help distinguish FNH from other liver conditions.
- Differential Diagnosis: Healthcare providers may need to differentiate FNH from other liver lesions or tumors, such as hepatocellular adenoma or hepatocellular carcinoma (liver cancer). Imaging studies, along with clinical evaluation, are used to make this distinction.
- Natural History: FNH is generally a stable condition, meaning it does not tend to grow or change significantly over time. It is not associated with a risk of developing into liver cancer. In most cases, FNH remains a benign and non-threatening liver lesion.
- Treatment: Treatment for FNH is usually unnecessary unless the lesion causes significant symptoms or if there is diagnostic uncertainty. In rare cases, when symptoms are severe or when there are concerns about potential complications, surgical removal of the FNH lesion may be considered. However, this is typically reserved for specific situations, and the decision to intervene is made on a case-by-case basis.
MRI appearance
The appearance of Focal nodular hyperplasia (FNH) on MRI imaging can vary depending on the sequences used and the individual characteristics of the lesion. Here is a general description of how FNH appears on different MRI sequences:
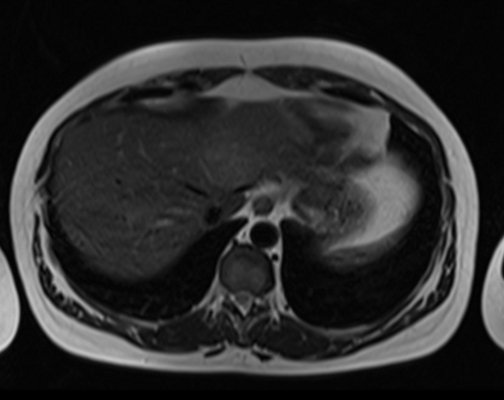
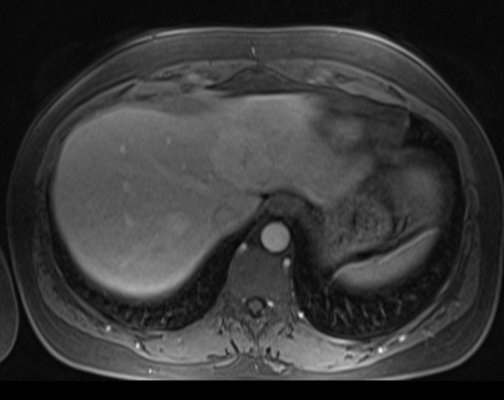
- T1-Weighted Imaging (T1WI):FNH lesions usually appear iso- to hypointense (similar to or slightly darker than normal liver tissue) on T1-weighted images. The central scar within the lesion may also appear hypointense.
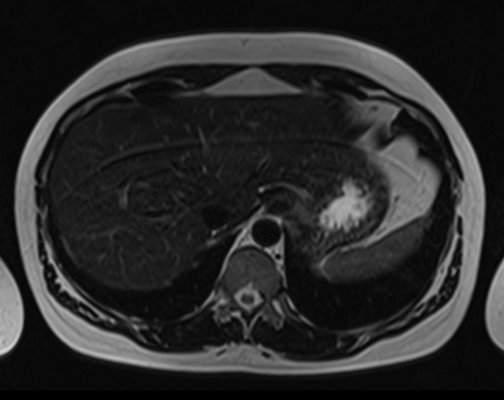
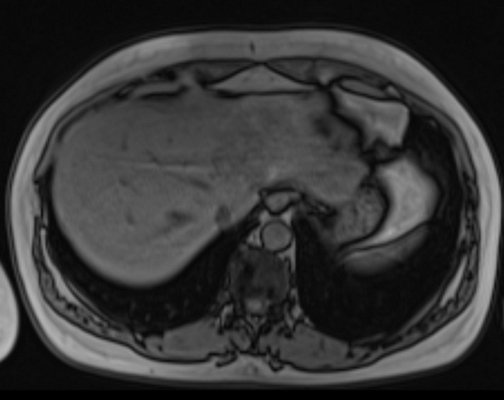
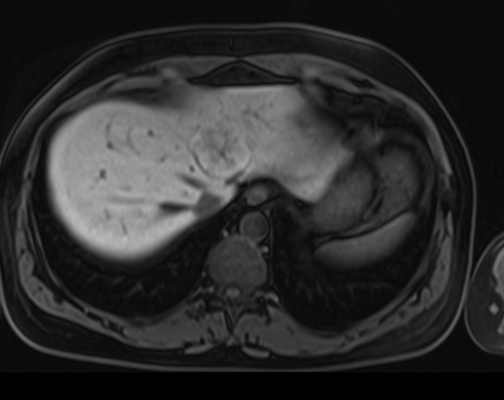
- T2-Weighted Imaging (T2WI):FNH lesions are typically hyperintense (brighter than normal liver tissue) on T2-weighted images. The central scar may vary in appearance but often remains hypointense.
- Diffusion-Weighted Imaging (DWI): FNH lesions usually have variable signal intensity on DWI, depending on their cellular density. They may appear hyperintense or isointense compared to surrounding liver tissue.
- In-phase and Out-of-phase Imaging (Chemical Shift Imaging):In-phase images are typically used to assess for fat content in liver lesions. FNH lesions may appear hyperintense in the in-phase images if they contain fat. In out-of-phase images, they may show signal loss due to the presence of fat.
- T1-Weighted Post-Contrast Imaging (Dynamic Contrast-Enhanced Imaging): FNH lesions show a characteristic enhancement pattern. They typically enhance brightly during the arterial phase (early post-contrast phase) due to their rich blood supply. This is followed by a washout during the portal venous and delayed phases, and they become isointense or hypointense compared to the surrounding liver tissue.
The central scar in FNH may or may not enhance with contrast, and its appearance can vary.

T2 fat saturated Axial
T2 Axial TE 90
T2 Axial TE 180

T1 IN PHASE
T1 out of phase
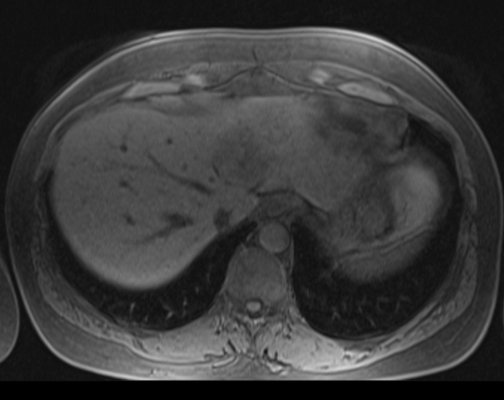
T1 pre contrast

T1 post contrast arterial phase
T1 post contrast venous phase

T1 post contrast 5 minutes
T1 post contrast 20 minutes
References
- Grazioli, L., Federle, M. P., Brancatelli, G., & Ichikawa, T. (2000). Focal nodular hyperplasia: Imaging findings with emphasis on multiphasic helical CT in 78 patients. Radiology, 215(1), 106-116.
- Vilgrain, V., Ronot, M., Duran, R., Van Nhieu, J. T., & Belghiti, J. (2008). Focal nodular hyperplasia: A review. Update on the imaging and management. Liver International, 28(6), 719-728.
- Chandarana, H., Robinson, E., Hajdu, C. H., & Drozhinin, L. (2010). Benign hepatocellular tumors: What the radiologist needs to know. Current Problems in Diagnostic Radiology, 39(5), 197-205.
- An, C., Rakhmonova, G., Choi, J. Y., Kim, M. J., & Kim, S. Y. (2016). Focal nodular hyperplasia of the liver: gadoxetic acid-enhanced MRI findings. Abdominal Imaging, 41(4), 746-755.
- Wang, W., Li, W., Fan, J., Huang, X., & Zhang, Z. (2020). Imaging features of focal nodular hyperplasia in the liver and the differential diagnosis from hepatocellular carcinoma. The British Journal of Radiology, 93(1115), 20190836.


