Subdural Haemorrhage
Subdural hemorrhage, often called subdural hematoma, is a medical term used to describe bleeding that occurs between the brain and its outermost protective covering called the dura mater. Imagine the brain as a delicate organ surrounded by protective layers like an onion. The dura mater is like the outermost peel of the onion.
Causes: Subdural hemorrhage is usually caused by a head injury or trauma that shakes or hits the brain inside the skull. This can happen in situations like car accidents, falls, or any event that causes the head to suddenly stop or change direction. When this happens, tiny blood vessels between the brain and the dura can tear, causing blood to leak into the space between them.
Effects: As blood collects between the brain and the dura, it creates pressure on the brain. This pressure can lead to various symptoms, such as headaches, confusion, dizziness, and even loss of consciousness. Since the brain is responsible for controlling everything our body does, any extra pressure on it can disrupt its normal functions.
Symptoms: Symptoms of subdural hemorrhage can vary. Some people might feel fine right after the injury but then develop symptoms gradually over hours or days. These can include a persistent headache that doesn’t go away with pain medication, changes in behavior, difficulty speaking or moving, and even seizures.
Diagnosis: Imaging like CT scans or MRI to see if there’s bleeding between the brain and the dura. These scans help them understand the location and size of the hemorrhage.
Treatment: Treatment depends on the severity of the hemorrhage. Small hemorrhages might not need surgical intervention and can be managed with observation and rest. However, larger hemorrhages that cause significant pressure on the brain might require surgery to remove the collected blood and relieve the pressure.
MRI appearance
T1-weighted Imaging (T1WI): Subdural hemorrhage typically exhibits varying levels of brightness, ranging from hyperintense (bright) to isointense or hypointense, depending on the stage of the hemorrhage—acute, subacute, or chronic—on T1-weighted images.
T2-weighted Imaging (T2WI): Subdural hemorrhage displays different degrees of brightness on T2-weighted images, appearing hyperintense (bright) or hypointense based on the stage of the hemorrhage—acute, subacute, or chronic.
Fluid-Attenuated Inversion Recovery (FLAIR) Imaging: FLAIR imaging is optimized to suppress the signal originating from cerebrospinal fluid (CSF), enhancing the visibility of lesions. In the context of subdural hemorrhage, FLAIR images can depict the hemorrhage as either hyperintense (bright) or hypointense, aligning with the acute, subacute, or chronic stage.
Diffusion-Weighted Imaging (DWI): Subdural hemorrhage commonly presents as hypointense (dark) on DWI. This occurrence arises from the fact that blood products hinder the movement of water molecules, leading to reduced signal intensity on diffusion-weighted images.
Susceptibility-Weighted Imaging (SWI): SWI is particularly attuned to the magnetic properties of blood products, especially those containing iron. Subdural hemorrhage may manifest as hypointense (black) on SWI due to the presence of deoxyhemoglobin and breakdown products of hemosiderin.
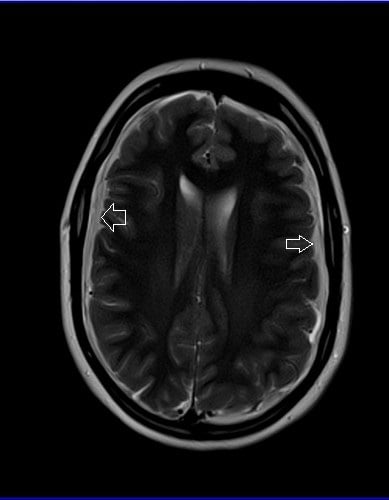
T2 Axial

Flair Axial

T1 Coronal

AXI DWI B0
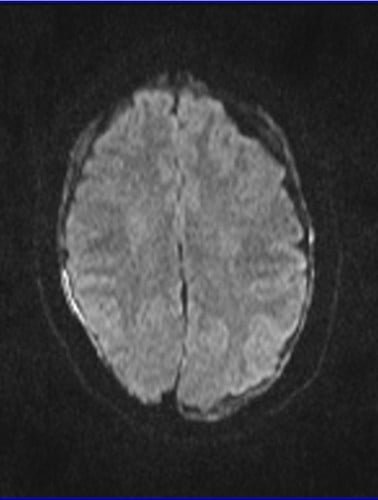
AXI DWI B 1000



