Pituitary Adenomas
Pituitary adenomas are non-cancerous tumors that develop in the pituitary gland, a small, pea-sized gland located at the base of the brain. Despite being benign, these tumors can cause significant health issues due to their location and the hormones they can produce or disrupt. The pituitary gland plays a crucial role in regulating various hormones that control growth, metabolism, reproduction, stress response, and other bodily functions.
Pituitary adenomas can be classified based on the hormones they secrete or their size. They are categorized as:
Functioning Adenomas: These tumors produce excessive amounts of hormones, leading to hormonal imbalances. Common types include prolactinomas (overproduction of prolactin), somatotropinomas (excessive growth hormone), corticotropinomas (overproduction of ACTH leading to Cushing’s disease), and thyrotropinomas (excess thyroid-stimulating hormone).
Non-Functioning Adenomas: These tumors do not produce significant amounts of hormones but can cause symptoms due to their size and compression of nearby structures.
Pituitary adenomas can be further classified based on their size into two main categories: microadenomas and macroadenomas. These classifications refer to the diameter of the tumor.
Microadenomas: Microadenomas are small pituitary adenomas, usually measuring less than 1 centimeter in diameter. Despite their small size, they can still cause significant hormonal imbalances due to their location within the pituitary gland. Microadenomas often present with symptoms related to hormone overproduction (functional microadenomas) or due to compression of nearby structures (non-functioning microadenomas).
Macroadenomas: Macroadenomas are larger pituitary adenomas, typically measuring 1 centimeter or more in diameter. Because of their size, macroadenomas can cause symptoms related to compression of nearby structures, such as the optic nerves, leading to visual disturbances. Like microadenomas, macroadenomas can also be functioning (producing excess hormones) or non-functioning (not producing significant hormones).
Symptoms of pituitary adenomas vary based on the type and size of the tumor. They may include hormonal imbalances, visual disturbances, headaches, fatigue, menstrual irregularities, growth abnormalities, and more. The diagnosis involves medical imaging, hormone level tests, and often consultation with endocrinologists and neurosurgeons.
Treatment options depend on factors such as tumor size, hormone production, and patient health. They can include medication, surgery to remove the tumor, radiation therapy, or a combination of these approaches. Pituitary adenomas are generally treatable, and early diagnosis and appropriate management can lead to improved outcomes.
MRI appearance
Pituitary adenomas can be characterized on MRI scans by their T1-weighted, T2-weighted, and post-contrast T1-weighted appearances. Here’s a general overview of how they might appear:
T1-weighted Imaging (T1WI): Pituitary adenomas typically appear as iso- to mildly hypointense compared to gray matter due to their solid nature. This is due to the relatively higher fat content and variable protein content in these tumors.
T2-weighted Imaging (T2WI): Pituitary adenomas usually appear hyperintense on T2WI due to their high water content. The signal intensity can vary based on the tumor’s consistency and cystic components.
Post-Contrast T1-weighted Imaging: After contrast administration (usually gadolinium-based contrast agents), pituitary adenomas can enhance. The degree and pattern of enhancement can vary, with some adenomas showing homogeneous enhancement while others might have areas of heterogeneous enhancement or rim enhancement.

T1 Sagittal Pre Contrast
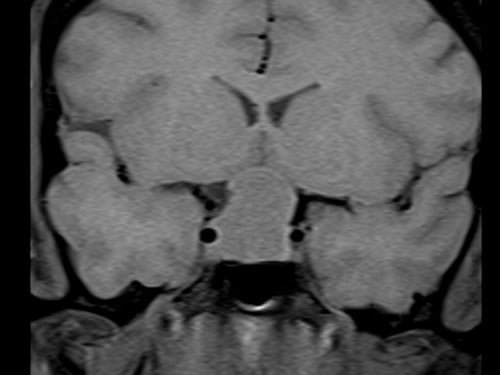
T1 Coronal Pre Contrast

T2 Coronal
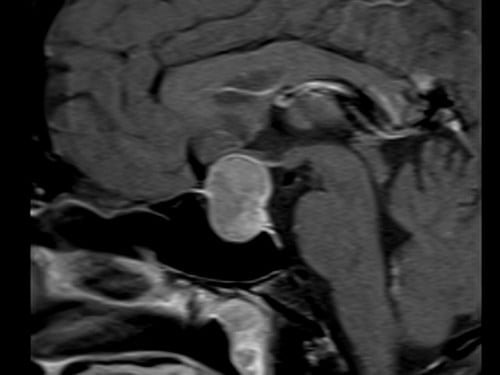
T1 Sagittal Post Contrast
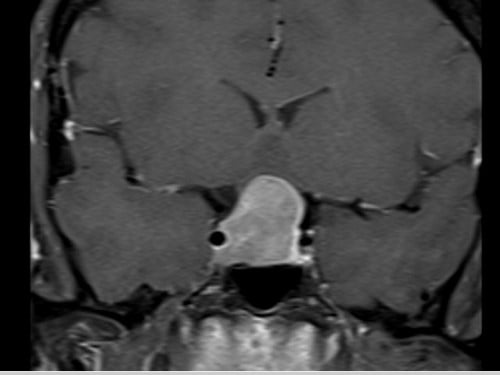
T1 Coronal Post Contrast
References
- Osborn, A. G., Preece, M. T. (2006). Intracranial tumors and masses: Radiology-Pathology Correlations from Head to Toe. Amirsys, Inc.
- Lee, D. K., & Lee, K. S. (2015). Magnetic resonance imaging of pituitary adenomas. Quantitative Imaging in Medicine and Surgery, 5(4), 576–591.
- Trouillas, J., & Jaffrain-Rea, M. L. (2009). Pituitary adenomas and related disorders. Springer.
- Barkhoudarian, G., & Kelly, D. F. (2011). Pituitary adenomas: Historical perspective, surgical management and future directions. CNS Oncology, 1(1), 29–41.
- Laws Jr, E. R., & Lopes, M. B. (2010). Pituitary tumors. Diagnostic pathology: Neuropathology. Amirsys.


